Rationale and Objectives
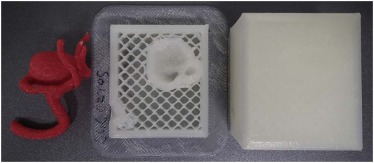
Three-dimensional (3D) printing is attracting increasing attention in the medical field. This study aimed to apply 3D printing to the production of hollow splenic artery aneurysm models for use in the simulation of endovascular treatment, and to evaluate the precision and accuracy of the simulation model.
Materials and Methods
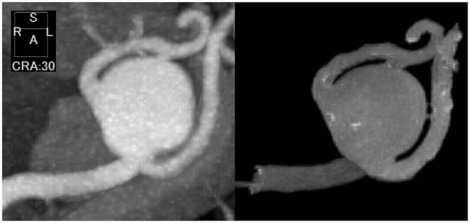
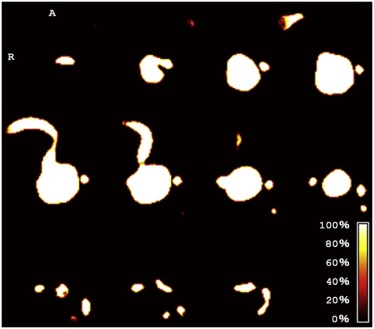
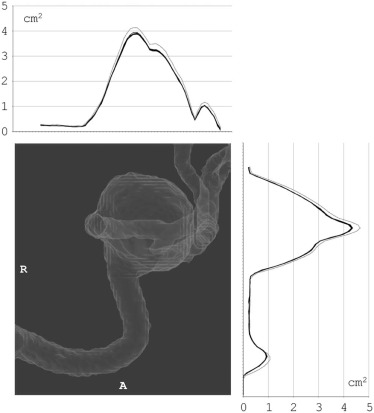
From 3D computed tomography (CT) angiography data of a splenic artery aneurysm, 10 hollow models reproducing the vascular lumen were created using a fused deposition modeling-type desktop 3D printer. After filling with water, each model was scanned using T2-weighted magnetic resonance imaging for the evaluation of the lumen. All images were coregistered, binarized, and then combined to create an overlap map. The cross-sectional area of the splenic artery aneurysm and its standard deviation (SD) were calculated perpendicular to the x - and y -axes.
Results
Most voxels overlapped among the models. The cross-sectional areas were similar among the models, with SDs <0.05 cm 2 . The mean cross-sectional areas of the splenic artery aneurysm were slightly smaller than those calculated from the original mask images. The maximum mean cross-sectional areas calculated perpendicular to the x - and y -axes were 3.90 cm 2 (SD, 0.02) and 4.33 cm 2 (SD, 0.02), whereas those calculated from the original mask images were 4.14 cm 2 and 4.66 cm 2 , respectively. The mean cross-sectional areas of the afferent artery were, however, almost the same as those calculated from the original mask images.
Conclusion
The results suggest that 3D simulation modeling of a visceral artery aneurysm using a fused deposition modeling-type desktop 3D printer and computed tomography angiography data is highly precise and accurate.
Introduction
Three-dimensional (3D) printing, also known as additive manufacturing or rapid prototyping, is a technology in which a 3D object is synthesized from digital data. 3D printing is attracting increasing attention in the medical field. Although a range of 3D printing techniques, including stereolithography (STL), selective laser sintering, inkjet printing, and fused deposition modeling (FDM), have been developed for industrial use, cost and speed are important considerations for the clinical “bedside” application of the technique. In FDM, one of the most widely used and least costly techniques, a 3D model is built on a layer-by-layer basis by extruding a melted filament of thermoplastic material from a nozzle.
The safety and effectiveness of interventional radiology procedures depend on the operator’s experience and the extent of understanding of the patient’s anatomy. In this regard, it would be useful if 3D printing could be applied to the preoperative simulation of the anatomy relevant to interventional radiology procedures. Previous studies have investigated the application of 3D printing to the production of hollow intracranial aneurysm models for the simulation of surgical and endovascular treatments . However, its application to visceral artery aneurysms has been extremely limited . Because of the way it works, it is difficult to construct complex structures such as hollow vascular models compared to simpler structures. For success in pre-procedure simulation and subsequent treatment, the model must precisely and accurately resemble the anatomic feature; however, to our knowledge, no study has evaluated the precision of aneurysm models.
Get Radiology Tree app to read full this article<
Materials and Methods
Model Fabrication
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Model Evaluation
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Results
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Discussion
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Acknowledgments
Get Radiology Tree app to read full this article<
References
1. Wetzel S.G., Ohta M., Handa A., et. al.: From patient to model: stereolithographic modeling of the cerebral vasculature based on rotational angiography. AJNR Am J Neuroradiol 2005; 26: pp. 1425-1427.
2. Kimura T., Morita A., Nishimura K., et. al.: Simulation of and training for cerebral aneurysm clipping with 3-dimensional models. Neurosurgery 2009; 65: pp. 719-725. discussion 25-6
3. Kono K., Shintani A., Okada H., et. al.: Preoperative simulations of endovascular treatment for a cerebral aneurysm using a patient-specific vascular silicone model. Neurol Med Chir (Tokyo) 2013; 53: pp. 347-351.
4. Mashiko T., Otani K., Kawano R., et. al.: Development of three-dimensional hollow elastic model for cerebral aneurysm clipping simulation enabling rapid and low cost prototyping. World Neurosurg 2015; 83: pp. 351-361.
5. Namba K., Higaki A., Kaneko N., et. al.: Microcatheter shaping for intracranial aneurysm coiling using the 3-dimensional printing rapid prototyping technology: preliminary result in the first 10 consecutive cases. World Neurosurg 2015; 84: pp. 178-186.
6. Anderson J.R., Thompson W.L., Alkattan A.K., et. al.: Three-dimensional printing of anatomically accurate, patient specific intracranial aneurysm models. J Neurointerv Surg 2016; 8: pp. 517-520.
7. Frolich A.M., Spallek J., Brehmer L., et. al.: 3D printing of intracranial aneurysms using fused deposition modeling offers highly accurate replications. AJNR Am J Neuroradiol 2016; 37: pp. 120-124.
8. Itagaki M.W.: Using 3D printed models for planning and guidance during endovascular intervention: a technical advance. Diagn Interv Radiol 2015; 21: pp. 338-341.