Rationale and Objectives
To assess image quality, radiation dose, and diagnostic accuracy of 70-kVp high-pitch computed tomography pulmonary angiography (CTPA) using 40 mL contrast agent and sinogram affirmed iterative reconstruction (SAFIRE) compared to 100-kVp CTPA using 60 mL contrast agent and filtered back projection.
Materials and Methods
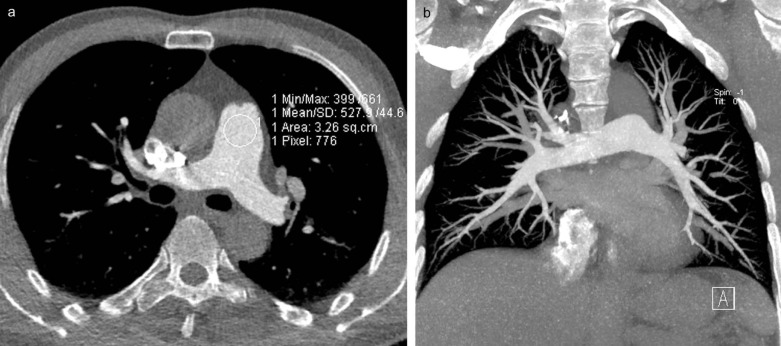
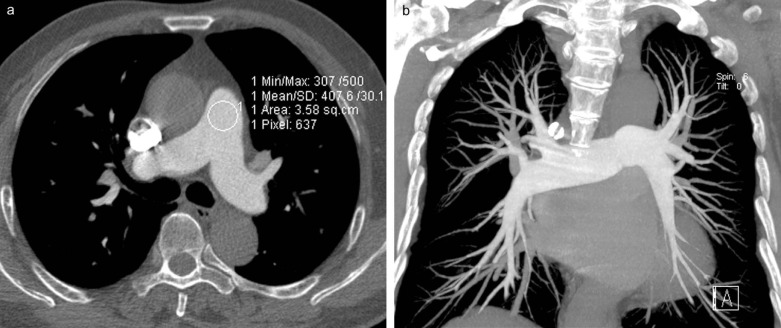
Eighty patients underwent CTPA at either 70 kVp (group A, n = 40; 3.2 pitch, 40 mL contrast medium, and SAFIRE) or 100 kVp (group B, n = 40; 1.2 pitch, 60 mL contrast medium, and filtered back projection). Signal-to-noise ratio and contrast-to-noise ratio were calculated. Subjective image quality was evaluated using a five-grade scale, and diagnostic accuracy was assessed. Radiation doses were compared.
Results
Computed tomography values, signal-to-noise ratio, and contrast-to-noise ratio of pulmonary arteries were higher in group A compared to group B (all P < 0.001). Subjective image quality showed no difference between the two groups ( P = 0.559) with good interobserver agreement (κ = 0.647). No difference was found regarding diagnostic accuracy between the two groups ( P > 0.05). The effective dose for group A was lower by 80% compared to group B ( P < 0.001).
Conclusions
70-kVp high-pitch CTPA with reduced contrast media and SAFIRE provides comparable image quality and substantial radiation dose savings compared to a routine CTPA protocol.
Introduction
Pulmonary embolism (PE) is considered the third most common acute cardiovascular disease after myocardial infarction and stroke . The prompt diagnosis and early initiation of appropriate medical treatment can reduce mortality of acute PE . Therefore, it is imperative to correctly diagnose PE in a timely fashion. Currently, computed tomography pulmonary angiography (CTPA) is established as the first-line imaging procedure to exclude PE . Wide availability and overuse of CTPA may result in substantial radiation exposure to patients, especially those requiring multiple follow-up CTPA studies for the evaluation of PE. Thus, increasing attention is now being paid to the optimization of radiation exposure from CTPA examinations . An additional concern is the contrast-induced nephropathy related to the administration of large doses of iodinated contrast media . In recent years, usage of reduced contrast agent volume has been advocated for CTPA .
Multiple strategies have been developed to reduce radiation dose and contrast volume of computed tomography angiography (CTA), including tube current modulation techniques, reduced tube voltage, automatic tube potential selection, high-pitch acquisition, iterative reconstruction algorithms, and combinations of these techniques . Among these dose-saving techniques, reduced tube voltage acquisition has been shown to be a powerful tool to lower radiation dose and contrast volume. A tube voltage of 80 kVp has been confirmed to be feasible for CTPA, with substantial reduction of radiation dose . Recently, Wichmann et al. demonstrated the feasibility of 70-kVp CTPA with 1.2 pitch and 70 mL contrast agent, and the lowest effective dose (ED) reported was 0.94 ± 0.17 mSv for single-source CTPA . By combining reduced tube voltage, high-pitch acquisition, and iterative reconstruction techniques, radiation dose and contrast agent volume can be substantially lowered. Lu et al. obtained sufficient image quality and a mean ED as low as 0.9 mSv in patients with suspected PE who underwent 80-kVp high-pitch CTPA with iterative reconstruction .
Get Radiology Tree app to read full this article<
Materials and Methods
Patients
Get Radiology Tree app to read full this article<
Computed Tomography (CT) Scanning Protocol
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Image Quality Evaluation
Objective Image Quality Evaluation
Get Radiology Tree app to read full this article<
SNR=CT valuepulmonary artery/background noise SNR
=
CT value
pulmonary artery
/
background noise
CNR=(CT valuepulmonary artery−CT valuemuscle)/background noise CNR
=
(
CT value
pulmonary artery
−
CT value
muscle
)
/
background noise
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Subjective Image Quality Evaluation
Get Radiology Tree app to read full this article<
Detection of Pulmonary Emboli
Get Radiology Tree app to read full this article<
Radiation Dose Estimation
Get Radiology Tree app to read full this article<
Statistical Analysis
Get Radiology Tree app to read full this article<
Results
Subjects
Get Radiology Tree app to read full this article<
Image Quality Evaluation
Get Radiology Tree app to read full this article<
TABLE 1
Objective Image Quality Measurements in the Two CTPA Groups
Location Group A Group B_P_ Value MPA CT number (HU) 712.2 ± 129.3 401.4 ± 81.6 <0.001 SNR 41.8 ± 12.5 29.1 ± 14.3 <0.001 CNR 36.9 ± 11.7 25.4 ± 13.0 <0.001 RPA CT number (HU) 682.1 ± 105.8 384.6 ± 74.1 <0.001 SNR 40.1 ± 11.7 28.0 ± 14.3 <0.001 CNR 35.2 ± 10.8 24.3 ± 13.0 <0.001 LPA CT number (HU) 678.0 ± 107.4 379.4 ± 79.5 <0.001 SNR 39.9 ± 11.8 27.6 ± 14.1 <0.001 CNR 35.0 ± 11.0 23.9 ± 12.8 <0.001 RULA CT number (HU) 650.7 ± 117.8 359.6 ± 88.0 <0.001 SNR 38.3 ± 12.3 26.0 ± 12.1 <0.001 CNR 33.4 ± 11.5 22.2 ± 11.0 <0.001 RILA CT number (HU) 633.3 ± 85.1 350.3 ± 77.0 <0.001 SNR 37.3 ± 10.8 25.6 ± 13.8 <0.001 CNR 32.4 ± 9.9 21.8 ± 12.5 <0.001 LULA CT number (HU) 653.1 ± 99.2 345.2 ± 102.1 <0.001 SNR 38.6 ± 12.3 25.1 ± 13.9 <0.001 CNR 33.7 ± 11.4 21.4 ± 12.7 <0.001 LILA CT number (HU) 677.3 ± 83.3 347.5 ± 77 <0.001 SNR 39.8 ± 11.2 25.4 ± 13.6 <0.001 CNR 34.9 ± 10.3 21.7 ± 12.3 <0.001 Muscle CT number (HU) 84.0 ± 21.3 52.0 ± 8.6 <0.001 Noise (HU) 17.9 ± 4.2 14.8 ± 2.9 <0.001
CNR, contrast-to-noise ratio; CT, computed tomography; CTPA, computed tomography pulmonary angiography; HU, Hounsfield units; LILA, left inferior lobe pulmonary artery; LPA, left pulmonary artery; LULA, left upper lobe pulmonary artery; MPA, main pulmonary artery; RILA, right inferior lobe pulmonary artery; RPA, right pulmonary artery; RULA, right upper lobe pulmonary artery; SNR, signal-to-noise ratio.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
TABLE 2
Subjective Image Quality Evaluation in the Two CTPA Groups
Readers Group A Group B_P_ Value Reader 1 1.05 ± 0.22 1.08 ± 0.27 0.646 Reader 2 1.03 ± 0.16 1.08 ± 0.27 0.308 Both readers 1.03 ± 0.16 1.05 ± 0.22 0.559 Kappa value 0.655 0.640 —
CTPA, computed tomography pulmonary angiography.
Get Radiology Tree app to read full this article<
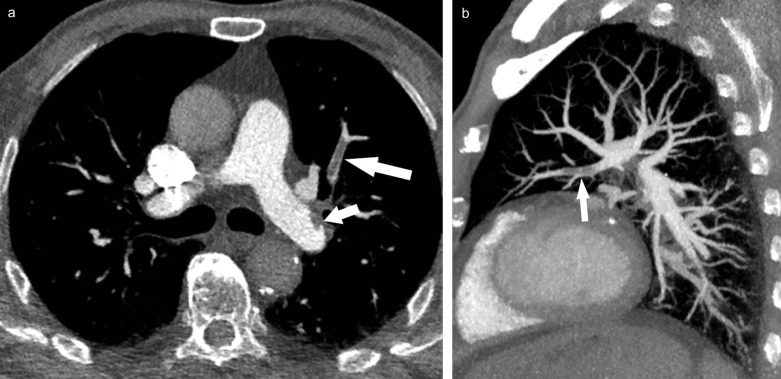
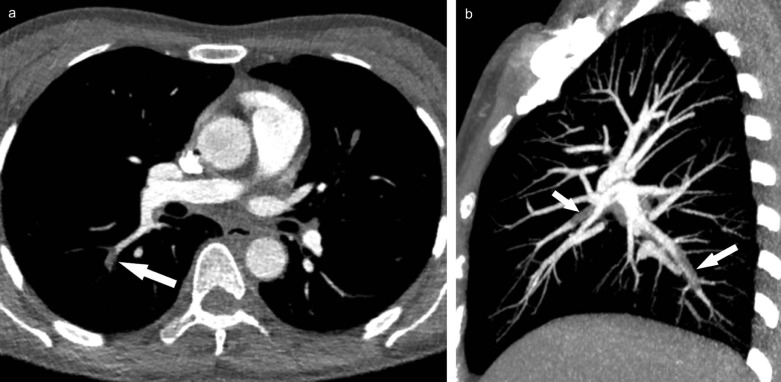
Detection of Pulmonary Emboli
Get Radiology Tree app to read full this article<
TABLE 3
Pulmonary Embolism Detected by Two Readers
True Positive False Negative False Positive True Negative Group A Group B Group A Group B Group A Group B Group A Group B Patients Reader 1 7 7 0 0 0 0 33 33 Reader 2 6 7 1 0 0 0 33 33 Central PE Reader 1 15 8 0 0 0 0 345 352 Reader 2 15 8 0 0 0 0 345 352 Peripheral PE Reader 1 23 29 1 3 2 3 774 765 Reader 2 21 27 3 5 1 2 775 766
PE, pulmonary embolism.
The data for the central arteries refer to the number of affected main and lobar pulmonary arteries. The data for the peripheral arteries refer to the number of affected pulmonary segmental and subsegmental arteries.
TABLE 4
Diagnostic Accuracy Comparison of the Two CTPA Protocols
Sensitivity Specificity PPV NPV Accuracy_P_ Value Group A Group B Group A Group B Group A Group B Group A Group B Group A Group B Patients Reader 1 100
(59.0–100) 100
(59.0–100) 100
(89.4–100) 100
(89.4–100) 100
(59.0–100) 100
(59.0–100) 100
(89.4–100) 100
(89.4–100) 100
(71.4–100) 100
(71.4–100) >0.99 Reader 2 85.7
(42.1–99.6) 100
(59.0–100) 100
(89.4–100) 100
(89.4–100) 100
(54.1–100) 100
(59.0–100) 100
(84.7–99.9) 100
(89.4–100) 97.5
(69.3–100) 100
(71.4–100) 0.91 Central PE Reader 1 100
(78.2–100) 100
(63.1–100) 100
(98.9–100) 100
(99.0–100) 100
(78.2–100) 100
(63.1–100) 100
(98.9–100) 100
(99.0–100) 100
(89.9–100) 100
(89.9–100) >0.99 Reader 2 100
(78.2–100) 100
(63.1–100) 100
(98.9–100) 100
(99.0–100) 100
(78.2–100) 100
(63.1–100) 100
(98.9–100) 100
(99.0–100) 100
(89.9–100) 100
(89.9–100) >0.99 Peripheral PE Reader 1 95.8
(78.9–99.9) 90.6
(75.0–98.0) 99.7
(99.1–100) 99.6
(98.9–99.9) 92.0
(74.0–99.0) 90.6
(75.0–98) 99.9
(99.3–100) 99.6
(98.9–99.9) 99.6
(92.8–100) 99.3
(92.5–100) 0.94 Reader 2 87.5
(67.6–97.3) 84.4
(67.2–94.7) 99.9
(99.3–100) 99.8
(99.1–100) 95.5
(77.2–99.9) 93.1
(77.2–99.2) 99.6
(98.9–99.9) 99.4
(98.5–99.8) 99.5
(92.7–100) 99.1
(92.3–100) 0.94
CTPA, computed tomography pulmonary angiography; NPV, negative predictive value; PPV, positive predictive value; PE, pulmonary embolism.
Data in parentheses indicate a 95% confidence interval.
Get Radiology Tree app to read full this article<
Radiation Dose Comparison
Get Radiology Tree app to read full this article<
TABLE 5
Radiation Dose Estimation and Comparison in This Study
Parameters Group A Group B_P_ Value CTDIvol (mGy) 0.8 ± 0.1 4.3 ± 0.9 <0.001 DLP (mGy × cm) 28.6 ± 8.3 142.7 ± 27.1 <0.001 ED (mSv) 0.4 ± 0.1 2.0 ± 0.4 <0.001
CTDIvol, volume CT dose index; DLP, dose–length product; ED, effective dose.
Get Radiology Tree app to read full this article<
Discussion
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
References
1. Zhang L.J., Zhang Z., Li S.J., et. al.: Pulmonary embolism and renal vein thrombosis in patients with nephrotic syndrome: prospective evaluation of prevalence and risk factors with CT. Radiology 2014; 273: pp. 897-906.
2. Burns S.K., Haramati L.B.: Diagnostic imaging and risk stratification of patients with acute pulmonary embolism. Cardiol Rev 2012; 20: pp. 15-24.
3. Mayo J., Thakur Y.: Pulmonary CT angiography as first-line imaging for PE: image quality and radiation dose considerations. AJR Am J Roentgenol 2013; 200: pp. 522-528.
4. Zhang L.J., Zhao Y.E., Wu S.Y., et. al.: Pulmonary embolism detection with dual-energy CT: experimental study of dual-source CT in rabbits. Radiology 2009; 252: pp. 61-70.
5. Zamboni G.A., Guariglia S., Bonfante A., et. al.: Low voltage CTPA for patients with suspected pulmonary embolism. Eur J Radiol 2012; 81: pp. e580-e584.
6. Costello J.E., Cecava N.D., Tucker J.E., et. al.: CT radiation dose: current controversies and dose reduction strategies. AJR Am J Roentgenol 2013; 201: pp. 1283-1290.
7. Ronco C., Stacul F., McCullough P.A.: Subclinical acute kidney injury (AKI) due to iodine-based contrast media. Eur Radiol 2013; 23: pp. 319-323.
8. Stacul F., van der Molen A.J., Reimer P., et. al.: Contrast induced nephropathy: updated ESUR Contrast Media Safety Committee guidelines. Eur Radiol 2011; 21: pp. 2527-2541.
9. Faggioni L., Neri E., Sbragia P., et. al.: 80-kV pulmonary CT angiography with 40 mL of iodinated contrast material in lean patients: comparison of vascular enhancement with iodixanol (320 mg I/mL) and iomeprol (400 mg I/mL). AJR Am J Roentgenol 2012; 199: pp. 1220-1225.
10. Wu C.C., Lee E.W., Suh R.D., et. al.: Pulmonary 64-MDCT angiography with 30 mL of IV contrast material: vascular enhancement and image quality. AJR Am J Roentgenol 2012; 199: pp. 1247-1251.
11. Wang Z., Chen Y., Wang Y., et. al.: Feasibility of low-dose contrast medium high pitch CT angiography for the combined evaluation of coronary, head and neck arteries. PLoS ONE 2014; 9: pp. e90268.
12. Goble E.W., Abdulkarim J.A.: CT pulmonary angiography using a reduced volume of high-concentration iodinated contrast medium and multiphasic injection to achieve dose reduction. Clin Radiol 2014; 69: pp. 36-40.
13. Schindera S.T., Nauer C., Treier R., et. al.: Strategies for reducing the CT radiation dose. Radiologe 2010; 50: pp. 1122-1127.
14. Newhouse J.H., RoyChoudhury A.: Quantitating contrast medium-induced nephropathy: controlling the controls. Radiology 2013; 267: pp. 4-8.
15. Szucs-Farkas Z., Megyeri B., Christe A., et. al.: Prospective randomised comparison of diagnostic confidence and image quality with normal-dose and low-dose CT pulmonary angiography at various body weights. Eur Radiol 2014; 24: pp. 1868-1877.
16. Viteri-Ramirez G., Garcia-Lallana A., Simon-Yarza I., et. al.: Low radiation and low-contrast dose pulmonary CT angiography: comparison of 80 kVp/60 ml and 100 kVp/80 ml protocols. Clin Radiol 2012; 67: pp. 833-839.
17. Wichmann J.L., Hu X., Kerl J.M., et. al.: 70 kVp computed tomography pulmonary angiography: potential for reduction of iodine load and radiation dose. J Thorac Imaging 2015; 30: pp. 69-76.
18. Lu G.M., Luo S., Meinel F.G., et. al.: High-pitch computed tomography pulmonary angiography with iterative reconstruction at 80 kVp and 20 mL contrast agent volume. Eur Radiol 2014; 24: pp. 3260-3268.
19. Hwang H.J., Seo J.B., Lee H.J., et. al.: Low-dose chest computed tomography with sinogram-affirmed iterative reconstruction, iterative reconstruction in image space, and filtered back projection: studies on image quality. J Comput Assist Tomogr 2013; 37: pp. 610-617.
20. Li Q., Yu H., Zhang L., et. al.: Combining low tube voltage and iterative reconstruction for contrast-enhanced CT imaging of the chest—initial clinical experience. Clin Radiol 2013; 68: pp. e249-e253.
21. Hou D.J., Tso D.K., Davison C., et. al.: Clinical utility of ultra high pitch dual source thoracic CT imaging of acute pulmonary embolism in the emergency department: are we one step closer towards a non-gated triple rule out?. Eur J Radiol 2013; 82: pp. 1793-1798.
22. Bauer R.W., Kramer S., Renker M., et. al.: Dose and image quality at CT pulmonary angiography—comparison of first and second generation dual-energy CT and 64-slice CT. Eur Radiol 2011; 21: pp. 2139-2147.
23. Szucs-Farkas Z., Schaller C., Bensler S., et. al.: Detection of pulmonary emboli with CT angiography at reduced radiation exposure and contrast material volume: comparison of 80 kVp and 120 kVp protocols in a matched cohort. Invest Radiol 2009; 44: pp. 793-799.
24. Laqmani A., Regier M., Veldhoen S., et. al.: Improved image quality and low radiation dose with hybrid iterative reconstruction with 80 kV CT pulmonary angiography. Eur J Radiol 2014; 83: pp. 1962-1969.
25. Co S.J., Mayo J., Liang T., et. al.: Iterative reconstructed ultra high pitch CT pulmonary angiography with cardiac bowtie-shaped filter in the acute setting: effect on dose and image quality. Eur J Radiol 2013; 82: pp. 1571-1576.
26. Sodickson A.: Strategies for reducing radiation exposure in multi-detector row CT. Radiol Clin North Am 2012; 50: pp. 1-14.
27. Gunn M.L., Kohr J.R.: State of the art: technologies for computed tomography dose reduction. Emerg Radiol 2010; 17: pp. 209-218.
28. Szucs-Farkas Z., Christe A., Megyeri B., et. al.: Diagnostic accuracy of computed tomography pulmonary angiography with reduced radiation and contrast material dose: a prospective randomized clinical trial. Invest Radiol 2014; 49: pp. 201-208.
29. Qi L., Meinel F.G., Zhou C.S., et. al.: Image quality and radiation dose of lower extremity CT angiography using 70 kVp, high pitch acquisition and sinogram-affirmed iterative reconstruction. PLoS ONE 2014; 9: pp. e99112.
30. Zhang L.J., Qi L., Wang J., et. al.: Feasibility of prospectively ECG-triggered high-pitch coronary CT angiography with 30 mL iodinated contrast agent at 70 kVp: initial experience. Eur Radiol 2014; 24: pp. 1537-1546.
31. Zhang L.J., Qi L., De Cecco C.N., et. al.: High-pitch coronary CT angiography at 70 kVp with low contrast medium volume: comparison of 80 and 100 kVp high-pitch protocols. Medicine (Baltimore) 2014; 93: pp. e92.
32. Chen G.Z., Zhang L.J., Schoepf U.J., et. al.: Radiation dose and image quality of 70 kVp cerebral CT angiography with optimized sinogram-affirmed iterative reconstruction: comparison with 120 kVp cerebral CT angiography. Eur Radiol 2015; 25: pp. 1453-1463.
33. De Zordo T., von Lutterotti K., Dejaco C., et. al.: Comparison of image quality and radiation dose of different pulmonary CTA protocols on a 128-slice CT: high-pitch dual source CT, dual energy CT and conventional spiral CT. Eur Radiol 2012; 22: pp. 279-286.