Rationale and Objectives
The objective of this study was to assess the feasibility of single-inhalation xenon-enhanced computed tomography (XeCT) to provide clinically practical, high-resolution pulmonary ventilation imaging to clinics with access to only a single-energy computed tomography scanner, and to reduce the subject’s overall exposure to xenon by utilizing a higher (70%) concentration for a much shorter time than has been employed in prior studies.
Materials and Methods
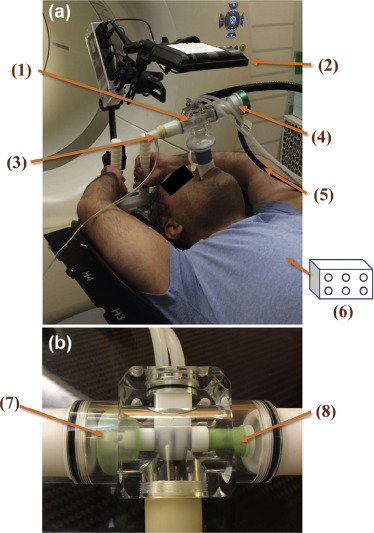
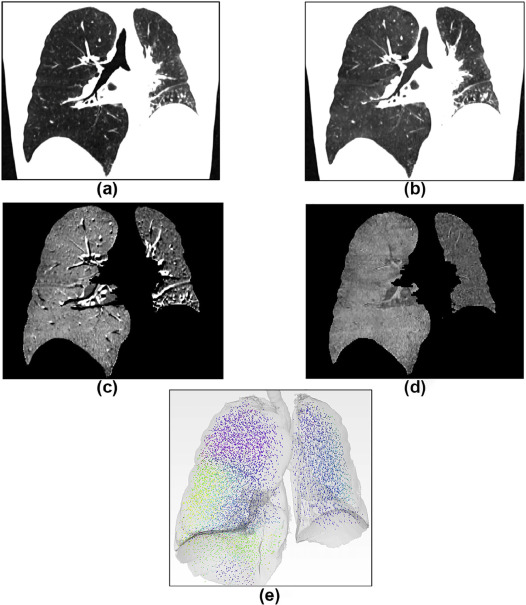
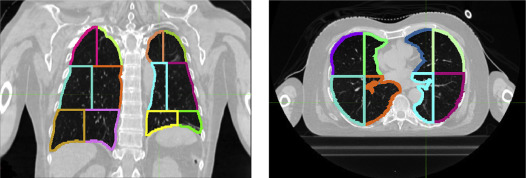
We conducted an institutional review board-approved prospective feasibility study of XeCT for 15 patients undergoing thoracic radiotherapy. For XeCT, we acquired two breath-hold single-energy computed tomography images of the entire lung with a single inhalation each of 100% oxygen and a mixture of 70% xenon and 30% oxygen, respectively. A video biofeedback system for coached patient breathing was used to achieve reproducible breath holds. We assessed the technical success of XeCT acquisition and side effects. We then used deformable image registration to align the breath-hold images with each other to accurately subtract them, producing a map of lung xenon distribution. Additionally, we acquired ventilation single-photon emission computed tomography-computed tomography (V-SPECT-CT) images for 11 of the 15 patients. For a comparative analysis, we partitioned each lung into 12 sectors, calculated the xenon concentration from the Hounsfield unit enhancement in each sector, and then correlated this with the corresponding V-SPECT-CT counts.
Results
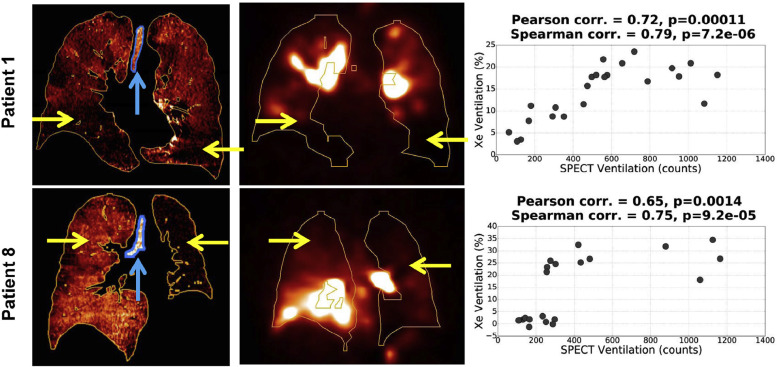
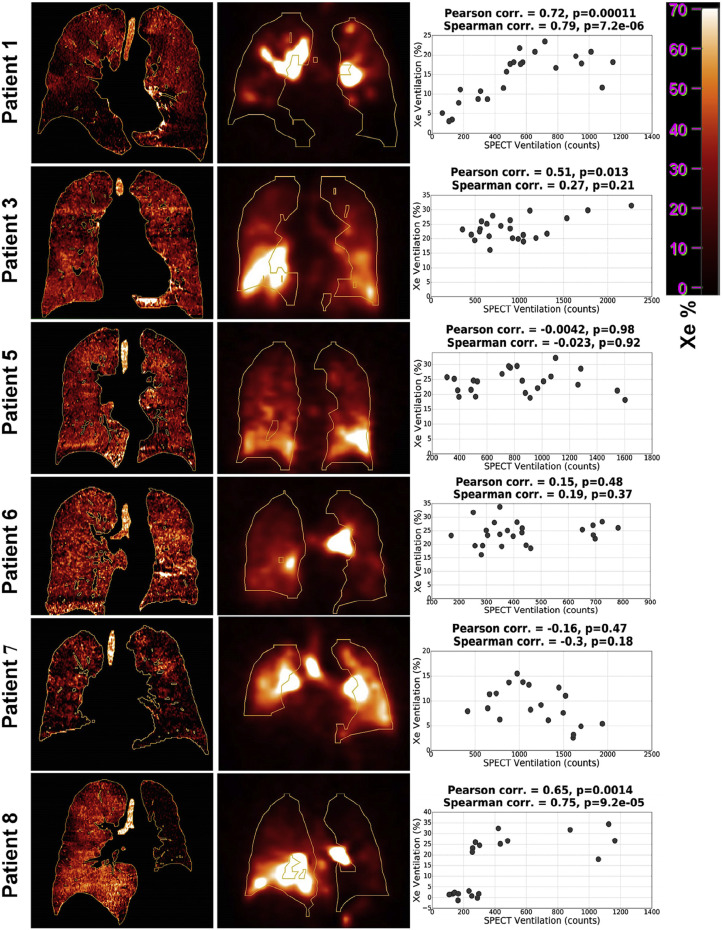
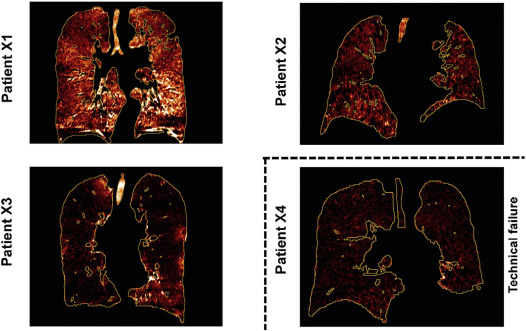
XeCT scans were tolerated well overall, with a mild (grade 1) dizziness as the only side effect in 5 of the 15 patients. Technical failures in five patients occurred because of inaccurate breathing synchronization with xenon gas delivery, leaving seven patients analyzable for XeCT and single-photon emission computed tomography correlation. Sector-wise correlations were strong (Spearman coefficient >0.75, Pearson coefficient >0.65, P value <.002) for two patients for whom ventilation deficits were visibly pronounced in both scans. Correlations were nonsignificant for the remaining five who had more homogeneous XeCT ventilation maps, as well as strong V-SPECT-CT imaging artifacts attributable to airway deposition of the aerosolized imaging agent. Qualitatively, XeCT demonstrated higher resolution and no central airway deposition artifacts compared to V-SPECT-CT.
Conclusions
In this pilot study, single-breath XeCT ventilation imaging was generally feasible for patients undergoing thoracic radiotherapy, using an imaging protocol that is clinically practical and potentially widely available. In the future, the xenon delivery failures can be addressed by straightforward technical improvements to the patient biofeedback coaching system.
Introduction
Xenon (Xe) is a radio-opaque and inert gas; therefore, it may be a viable and safe gas-phase computed tomography (CT) contrast agent to quantify regional pulmonary ventilation in humans. In order for such a contrast agent to be adopted widely, several clinical traits must be met: safety, convenience for the patient, and ease of implementation. Numerous studies have already explored the technical advantages of xenon-enhanced computed tomography (XeCT), such as its ability to provide reasonably safe high-resolution ventilation images. Dual-energy XeCT has been reported in patient and phantom studies , but most XeCT studies, to date, have used a multiple breath-hold technique in which patients inhale xenon for 1–2 minutes to reach equilibrium before image acquisition and xenon washout .
There have also been research efforts to compare XeCT against currently available three-dimensional ventilation imaging, that is, single-photon emission computed tomography (SPECT) . Substantial agreement has recently been observed between XeCT and krypton-81m (Kr-81m) ventilation SPECT images in an intermodality blind analysis of lung ventilation defects . With this result lending further credence to the use of gas-phase CT contrast agents for ventilation imaging, we aim to further expand upon its potential for future clinical implementation. By increasing the relative xenon concentration by a factor of two relative to prior studies, but reducing the xenon exposure to a single breath-hold duration (a factor of 5 or more reduction in exposure time compared to the studies noted earlier), a more rapid image acquisition may be possible with an overall reduction in patients’ total exposure to xenon gas, a known anesthetic agent.
Get Radiology Tree app to read full this article<
Materials and Methods
Patients
Get Radiology Tree app to read full this article<
Assessment of Adverse Events
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
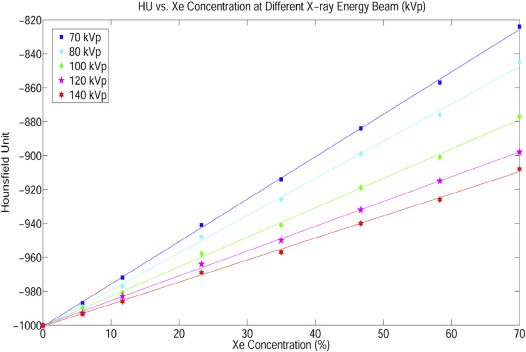
Relation of Hounsfield Unit and Xenon Concentration at Different X-ray Energies
Get Radiology Tree app to read full this article<
Video Biofeedback System
Get Radiology Tree app to read full this article<
XeCT Imaging
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Deformable Image Registration Method
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
SPECT-CT Imaging
Get Radiology Tree app to read full this article<
Analysis of XeCT Images and Correlation with V-SPECT-CT
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Statistical Analysis
Get Radiology Tree app to read full this article<
Results
Patient Characteristics
Get Radiology Tree app to read full this article<
TABLE 1
Individual Patient Data
Patient Gender Xe~V-SPECT-CT Spearman Coefficient ( P Value) Xe~V-SPECT-CT Pearson Coefficient ( P Value) Mean Xenon Enhancement: Trachea (HU) Lung Volume (L, at Inspiration) Lung Volume Difference (%) (Xe vs O 2 ) FEV 1 % COPD (GOLD Score) 1 M 0.79 (.000007) 0.72 (.00011) 97.8 7.9 −4.0 39 3 2 \* M −0.34 −0.16 10.3 5.1 −1.0 61 1 3 F 0.27 (.21) 0.51 (.013) 115.1 3.9 1.2 79 No COPD 4 \* M 0.39 0.51 16.5 4.2 −25.8 60 1 5 M 0.02 (.92) 0.004 (.98) 131.0 7.1 11.8 107 No COPD 6 M 0.19 (.37) 0.15 (.48) 113.3 4.6 −1.4 59 No COPD 7 F −0.3 (.18) −0.16 (.47) 127.2 3.7 13.7 64 1 8 M 0.75 (.00009) 0.65 (.0014) 134.2 6.0 0.9 62 1 9 M 0.33 (.12) 0.4 (.059) 100.8 8.2 −4.1 59 2 10 \* M −0.04 0.02 47.0 5.1 3.1 No PFT No PFT 11 \* F 0.45 0.27 −2.4 3.2 −7.5 59 2 X1 M — — 118.5 6.2 −1.4 75 1 X2 M — — 87.0 3.6 10.5 81 No COPD X3 F — — 132.2 6.1 −0.4 21 4 X4 \* M — — 6.4 4.4 0.4 87 No COPD
COPD, chronic obstructive pulmonary disease; F, female; FEV 1 %, forced expiratory volume; GOLD, Global Initiative for Chronic Obstructive Lung Disease; M, male; PFT, pulmonary function test; V-SPECT, ventilation single-photon emission computed tomography.
The third and fourth columns show the Spearman correlation coefficients ( P value) and the Pearson correlation coefficients ( P value), respectively, between xenon concentration and single-photon emission computed tomography ventilation image at corresponding sectors. The fifth and sixth columns show the Hounsfield unit enhancement in the trachea and the lung volume difference from the consecutive computed tomography images. The eighth and ninth columns show the PFT FEV 1 % and GOLD score for each patient, respectively. Patients X1–X4 participated in xenon-enhanced computed tomography imaging, but have no single-photon emission computed tomography ventilation. Patients 2, 4, 10, 11, and X4 had technical failure of xenon-enhanced computed tomography and were excluded from the correlation analysis. The patient ages ranged from 55 to 79 years (average 66 ± 7 years).
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Technical Feasibility and Side Effects
Get Radiology Tree app to read full this article<
Relation of Hounsfield Unit and Xenon Concentration at Different X-ray Energies
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Ventilation Maps
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Discussion
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Appendix
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
References
1. Chae E.J., Seo J.B., Goo H.W., et. al.: Xenon ventilation CT with a dual-energy technique of dual-source CT: initial experience. Radiology 2008; 248: pp. 615-624.
2. Park E.-A., Goo J.M., Park S.J., et. al.: Chronic obstructive pulmonary disease: quantitative and visual ventilation pattern analysis at xenon ventilation CT performed by using a dual-energy technique. Radiology 2010; 256: pp. 985-997.
3. Goo H., Yang D., Hong S.-J., et. al.: Xenon ventilation CT using dual-source and dual-energy technique in children with bronchiolitis obliterans: correlation of xenon and CT density values with pulmonary function test results. Pediatr Radiol 2010; 40: pp. 1490-1497.
4. Thieme S., Hoegl S., Nikolaou K., et. al.: Pulmonary ventilation and perfusion imaging with dual-energy CT. Eur Radiol 2010; 20: pp. 2882-2889.
5. Honda N., Osada H., Watanabe W., et. al.: Imaging of ventilation with dual-energy CT during breath hold after single vital-capacity inspiration of stable xenon. Radiology 2012; 262: pp. 262-268.
6. Murphy D.M., Nicewicz J.T., Zabbatino S.M., et. al.: Local pulmonary ventilation using nonradioactive xenon-enhanced ultrafast computed tomography. Chest 1989; 96: pp. 799-804.
7. Yanagita H., Honda N., Nakayama M., et. al.: Prediction of postoperative pulmonary function: preliminary comparison of single-breath dual-energy xenon CT with three conventional methods. Jpn J Radiol 2013; 31: pp. 377-385.
8. Ohno Y., Yoshikawa T., Takenaka D., et. al.: Xenon-enhanced CT using subtraction CT: basic and preliminary clinical studies for comparison of its efficacy with that of dual-energy CT and ventilation SPECT/CT to assess regional ventilation and pulmonary functional loss in smokers. Eur J Radiol 2017; 86: pp. 41-51.
9. Gomez F.P., Rodriguez-Roisin R.: Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines for chronic obstructive pulmonary disease. Curr Opin Pulm Med 2002; 8: pp. 81-86.
10. Yu A.S., von Eyben R., Yamamoto T., et. al.: Anatomic optimization of lung tumor stereotactic ablative radiation therapy. Pract Radiat Oncol 2015; 5: pp. e607-e613.
11. Klein S., Staring M., Murphy K., et. al.: Elastix: a toolbox for intensity-based medical image registration. IEEE Trans Med Imaging 2010; 29: pp. 196-205.
12. Shamonin D.P., Bron E.E., Lelieveldt B.P., et. al.: Disease neuroimaging, fast parallel image registration on CPU and GPU for diagnostic classification of Alzheimer’s disease. Front Neuroinform 2013; 7: pp. 50.
13. Nie K., Chuang C., Kirby N., et. al.: Site-specific deformable imaging registration algorithm selection using patient-based simulated deformations. Med Phys 2013; 40: 041911
14. Negahdar M., Fasola C.E., Yu A.S., et. al.: Noninvasive pulmonary nodule elastometry by CT and deformable image registration. Radiother Oncol 2015; 115: pp. 35-40.
15. Sato Y., Nakajima S., Shiraga N., et. al.: Three-dimensional multi-scale line filter for segmentation and visualization of curvilinear structures in medical images. Med Image Anal 1998; 2: pp. 143-168.
16. Schembri G.P., Roach P.J., Bailey D.L., et. al.: Artifacts and anatomical variants affecting ventilation and perfusion lung imaging. Semin Nucl Med 2015; 45: pp. 373-391.
17. Sase S., Nakano H., Suzuki H., et. al.: Subtraction lung image for evaluating pulmonary ventilation in xenon-enhanced CT. Med Phys 2010; 37: pp. 4464-4474.
18. Ding K., Bayouth J.E., Buatti J.M., et. al.: 4DCT-based measurement of changes in pulmonary function following a course of radiation therapy. Med Phys 2010; 37: pp. 1261-1272.
19. Munawar I., Yaremko B.P., Craig J., et. al.: Intensity modulated radiotherapy of non-small-cell lung cancer incorporating SPECT ventilation imaging. Med Phys 2010; 37: pp. 1863-1872.
20. Huang T.-C., Hsiao C.-Y., Chien C.-R., et. al.: IMRT treatment plans and functional planning with functional lung imaging from 4D-CT for thoracic cancer patients. Radiat Oncol 2013; 8: pp. 3.
21. Bates E.L., Bragg C.M., Wild J.M., et. al.: Functional image-based radiotherapy planning for non-small cell lung cancer: a simulation study. Radiother Oncol 2009; 93: pp. 32-36.
22. Vinogradskiy Y., Schubert L., Diot Q., et. al.: Regional lung function profiles of stage I and III lung cancer patients: an evaluation for functional avoidance radiation therapy. Int J Radiat Oncol 2016; 95: pp. 1273-1280.
23. Yamamoto T., Kabus S., Bal M., et. al.: The first patient treatment of computed tomography ventilation functional image-guided radiotherapy for lung cancer. Radiother Oncol 2016; 118: pp. 227-231.
24. Bellani G., Rouby J.J., Constantin J.M., et. al.: Looking closer at acute respiratory distress syndrome: the role of advanced imaging techniques. Curr Opin Crit Care 2017; 23: pp. 30-37.
25. Hwang H.J., Seo J.B., Lee S.M., et. al.: Assessment of regional xenon ventilation, perfusion, and ventilation-perfusion mismatch using dual-energy computed tomography in chronic obstructive pulmonary disease patients. Invest Radiol 2016; 51: pp. 306-315.
26. Hofman M.S., Beauregard J.-M., Barber T.W., et. al.: 68Ga PET/CT ventilation–perfusion imaging for pulmonary embolism: a pilot study with comparison to conventional scintigraphy. J Nucl Med 2011; 52: pp. 1513-1519.
27. Ament S.J., Maus S., Reber H., et. al.: PET lung ventilation/perfusion imaging using (68)Ga aerosol (Galligas) and (68)Ga-labeled macroaggregated albumin. Recent Results Cancer Res 2013; 194: pp. 395-423.
28. Bajc M., Neilly J.B., Miniati M., et. al.: EANM guidelines for ventilation/perfusion scintigraphy: part 1. Pulmonary imaging with ventilation/perfusion single photon emission tomography. Eur J Nucl Med Mol Imaging 2009; 36: pp. 1356-1370.
29. Jogi J., Jonson B., Ekberg M., et. al.: Ventilation-perfusion SPECT with 99mTc-DTPA versus Technegas: a head-to-head study in obstructive and nonobstructive disease. J Nucl Med 2010; 51: pp. 735-741.
30. Parameswaran K., Knight A.C., Keaney N.P., et. al.: Ventilation and perfusion lung scintigraphy of allergen-induced airway responses in atopic asthmatic subjects. Can Respir J 2007; 14: pp. 285-291.
31. Hachulla A.-L., Pontana F., Wemeau-Stervinou L., et. al.: Krypton ventilation imaging using dual-energy CT in chronic obstructive pulmonary disease patients: initial experience. Radiology 2012; 263: pp. 253-259.
32. Chon D., Beck K.C., Simon B.A., et. al.: Effect of low-xenon and krypton supplementation on signal/noise of regional CT-based ventilation measurements. J Appl Physiol 2007; 102: pp. 1535-1544.