Rationale and Objectives
Ongoing concerns over the rising cost of health care are driving large-scale changes in the way that health care is practiced and reimbursed in the United States.
Materials and Methods
To effectively implement and thrive within this new health care delivery environment, academic medical institutions will need to modify financial and business models and adapt institutional cultures. In this article, we review the expected features of the new health care environment from the perspective of academic radiology departments.
Conclusions
Our review will include background on accountable care organizations, identify challenges associated with the new managed care model, and outline key strategies—including expanding the use of existing information technology infrastructure, promoting continued medical innovation, balancing academic research with clinical care, and exploring new roles for radiologists in efficient patient management—that will ensure continued success for academic radiology.
Continued growth in health care spending with a constantly aging population has propelled concerns about the solvency of the current health care system in the United States. Health expenditure has risen dramatically over the past 50 years (17.4% of gross domestic product compared to 11.4% for Canada in 2009); however, US health performance lags behind by comparison based on indicators such as life expectancy, quality, access, efficiency, and equity . Nonalignment of cost with performance triggered the 2010 panel discussion by the Institute of Medicine. Factors identified by the Institute of Medicine as contributing to the cost-performance nonalignment included prevalence of chronic disease, lifestyle, and population health demographics (such as the obesity epidemic), but also inefficient delivery of services (excess administrative costs, unnecessary services, high pricing, deficiency in preventive care, and fraud, amounting to $765 billion) . Furthermore, considerable variation in quality of care (as indicated by readmission rates per Medicare beneficiary) has been reported without correlation to regional costs .
In this article, we will broadly review the landscape of the new health care delivery environment from the perspective of academic medical institutions and anticipated impact on the future of radiology. Our review will include a background on accountable care organizations (ACOs) and challenges associated with the new managed care environment, use of technology for managing data-intensive environments, role of radiologists in medical innovation, defining new boundaries and roles for radiology in patient management, and implications of balancing academics and clinical care.
Patient Protection and Affordable Care Act
Payment reform is based on the premise that the current fee-for-service (FFS) payment incentivizes physicians to increase services with consequent excess utilization. Overuse of subspecialty services relative to perceived appropriate level of management in the primary care environment has resulted in the targeting of subspecialist physicians including radiologists and procedure-centric physicians such as interventional cardiologists or gastroenterologists. In an attempt to avoid overuse of imaging and subspecialist referral, several payment models have been put forward ranging from prospective payment for discrete episodes of care to global payment or risk-based care .
Direct Mechanisms for Reduced Reimbursement
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
ACOs
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Payment Structure for Providers Under the ACO Model
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Providing Value for Radiology within an ACO
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Promoting Quality, Safety, and Best Practices
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Health information technology: A key to data management
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Data-Intensive Environment
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Connectivity, Interoperability, and Image Transfer
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Research and innovation in radiology
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Walking the Academic–Clinical Tight Rope
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Redefining radiology boundaries
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Service
Get Radiology Tree app to read full this article<
Quality Control
Get Radiology Tree app to read full this article<
Organization
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
A Broader Picture of Patient Care and Information Management
Get Radiology Tree app to read full this article<
Radiologists as Consultants
Get Radiology Tree app to read full this article<
Direct Patient Communication
Get Radiology Tree app to read full this article<
Radiologist Management of Imaging Follow-up
Get Radiology Tree app to read full this article<
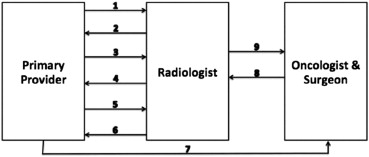
Imaging as the Basis of Subspecialist Referral
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Conclusion
Get Radiology Tree app to read full this article<
References
1. Fineberg H.V.: Shattuck Lecture. A successful and sustainable health system–how to get there from here. N Engl J Med 2012; 366: pp. 1020-1027.
2. Davis K., SC , Stremikis K.: Mirror, mirror on the wall: how the performance of the U.S. health care system compares internationally.2010.Commonwealth FundNew York
3. Yong P.L.Saunders R.S.Olsen L.A.The healthcare imperative: lowering costs and improving outcomes: workshop series summary.2010.The National Academies PressWashington, DC:
4. McCarthy D., Howe S.K.H., Schoen C., et. al.: Aiming higher: results from a state scorecard on health system performance.2009.The Commonwealth FundNew York, NY
5. Fisher E.S., Wennberg D.E., Stukel T.A., et. al.: The implications of regional variations in Medicare spending. Part 1: the content, quality, and accessibility of care. Ann Intern Med 2003; 138: pp. 273-287.
6. Landon B.E.: Keeping score under a global payment system. N Engl J Med 2012; 366: pp. 393-395.
7. Payment Policies Under the Physician Fee Schedule, Five-Year Review of Work Relative Value Units, Clinical Laboratory Fee Schedule: Signature on Requisition, and Other Revisions to Part B for CY 2012; Final Rule. Fed Reg 2012; 76:288.
8. Revisions to Payment Policies Under the Physician Fee Schedule, DME Face-to-Face Encounters, Elimination of the Requirement for Termination of Non-Random Prepayment Complex Medical Review and Other Revisions to Part B for CY 2013. Fed Reg 2012; 77:222.
9. Seidel R.L., Baumgarten D.A.: Pay for performance: survey of diagnostic radiology faculty and trainees. J Am Coll Radiol 2007; 4: pp. 411-415.
10. Moser J.W., Wilcox P.A., Bjork S.S., et. al.: Pay for performance in radiology: ACR white paper. J Am Coll Radiol 2006; 3: pp. 650-664.
11. McVey L.R.: Pay-for-performance radiology: a new concept. Radiol Manage 1999; 21: pp. 18-21.
12. Allen B., Levin D.C., Brant-Zawadzki M., et. al.: ACR white paper: strategies for radiologists in the era of health care reform and accountable care organizations: a report from the ACR Future Trends Committee. J Am Coll Radiol 2011; 8: pp. 309-317.
13. Becker G.J., Bosma J.L., Burleson J., et. al.: Introduction to value-based payment modifiers. J Am Coll Radiol 2012; 9: pp. 718-724.
14. Enzmann D.R.: Radiology’s value chain. Radiology 2012; 263: pp. 243-252.
15. Kahn C.E.: Artificial intelligence in radiology: decision support systems. Radiographics 1994; 14: pp. 849-861.
16. Rosenthal D.I., Weilburg J.B., Schultz T., et. al.: Radiology order entry with decision support: initial clinical experience. J Am Coll Radiol 2006; 3: pp. 799-806.
17. Kaplan B.: Evaluating informatics applications–clinical decision support systems literature review. Int J Med Inform 2001; 64: pp. 15-37.
18. Miller R.A.: Medical diagnostic decision support systems–past, present, and future: a threaded bibliography and brief commentary. J Am Med Inform Assoc 1994; 1: pp. 8-27.
19. Kruskal J.B., Reedy A., Pascal L., et. al.: Quality initiatives: lean approach to improving performance and efficiency in a radiology department. Radiographics 2012; 32: pp. 573-587.
20. Ondategui-Parra S., Bhagwat J.G., Gill I.E., et. al.: Essential practice performance measurement. J Am Coll Radiol 2004; 1: pp. 559-566.
21. Johnson C.D., Krecke K.N., Miranda R., et. al.: Quality initiatives: developing a radiology quality and safety program: a primer. Radiographics 2009; 29: pp. 951-959.
22. Mendiratta-Lala M., Eisenberg R.L., Steele J.R., et. al.: Quality initiatives: measuring and managing the procedural competency of radiologists. Radiographics 2011; 31: pp. 1477-1488.
23. Lee C.I., Enzmann D.R.: Measuring radiology’s value in time saved. J Am Coll Radiol 2012; 9: pp. 713-717.
24. Thompson T.G., Brailer D.J.: The decade of health information technology: delivering consumer-centric and information-rich health care.2004.US Department of Health and Human ServicesWashington, DC
25. Chaudhry B., Wang J., Wu S., et. al.: Systematic review: impact of health information technology on quality, efficiency, and costs of medical care. Ann Intern Med 2006; 144: pp. 742-752.
26. Blumenthal D.: Stimulating the adoption of health information technology. N Engl J Med 2009; 360: pp. 1477-1479.
27. Flanagan P.T., Relyea-Chew A., Gross J.A., et. al.: Using the internet for image transfer in a regional trauma network: effect on CT repeat rate, cost, and radiation exposure. J Am Coll Radiol 2012; 9: pp. 648-656.
28. Buntin M.B., Burke M.F., Hoaglin M.C., et. al.: The benefits of health information technology: a review of the recent literature shows predominantly positive results. Health Affairs 2011; 30: pp. 464-471.
29. Channin D.S., Bowers G., Nagy P.: Should radiology IT be owned by the chief information officer?. J Digit Imaging 2009; 22: pp. 218-221.
30. Arenson R.L.: PACS: current status and cost-effectiveness. Eur Radiol 2000; 10: pp. S354-S356.
31. Roberson G.H., Shieh Y.Y.: Radiology information systems, picture archiving and communication systems, teleradiology–overview and design criteria. J Digit Imaging 1998; 11: pp. 2-7.
32. Boochever S.S.: HIS/RIS/PACS integration: getting to the gold standard. Radiol Manage 2004; 26: pp. 16-24. quiz 25–27
33. Sung J.C., Sodickson A., Ledbetter S.: Outside CT imaging among emergency department transfer patients. J Am Coll Radiol 2009; 6: pp. 626-632.
34. Gupta R., Greer S.E., Martin E.D.: Inefficiencies in a rural trauma system: the burden of repeat imaging in interfacility transfers. J Trauma 2010; 69: pp. 253-255.
35. Pitts S.R., Niska R.W., Xu J., et. al.: National Hospital Ambulatory Medical Care Survey: 2006 emergency department summary. Natl Health Stat Report 2008; pp. 1-38.
36. Pinthus J.H., Farrokhyar F., Hassouna M.M., et. al.: Single-session primary high-intensity focused ultrasonography treatment for localized prostate cancer: biochemical outcomes using third generation-based technology. Br J Urol Int 2012; 110: pp. 1142-1148.
37. Rouviere O., Glas L., Girouin N., et. al.: Prostate cancer ablation with transrectal high-intensity focused ultrasound: assessment of tissue destruction with contrast-enhanced US. Radiology 2011; 259: pp. 583-591.
38. Kim H.S., Baik J.-H., Pham L.D., et. al.: MR-guided high-intensity focused ultrasound treatment for symptomatic uterine leiomyomata: long-term outcomes. Acad Radiol 2011; 18: pp. 970-976.
39. Kim Y.-S., Kim J.-H., Rhim H., et. al.: Volumetric MR-guided high-intensity focused ultrasound ablation with a one-layer strategy to treat large uterine fibroids: initial clinical outcomes. Radiology 2012; 263: pp. 600-609.
40. Cho Z.-H., Kang C.-K., Han J.-Y., et. al.: Observation of lenticulostriate arteries in the human brain in vivo using 7.0T MR angiography. Stroke 2008; 39: pp. 1604-1606.
41. Conijn M.M., Geerlings M.I., Biessels G.J., et. al.: Cerebral microbleeds on MR imaging: comparison between 1.5 and 7T. Am J Neuroradiol 2011; 32: pp. 1043-1049.
42. Manglaviti G., Tresoldi S., Guerrer C.S., et. al.: In vivo evaluation of the chemical composition of urinary stones using dual-energy CT. AJR Am J Roentgenol 2011; 197: pp. W76-W83.
43. Song K.D., Kim C.K., Park B.K., et. al.: Utility of iodine overlay technique and virtual unenhanced images for characterization of renal masses by dual-energy CT. AJR Am J Roentgenol 2011; 197: pp. W1076-W1082.
44. Neville A.M., Gupta R.T., Miller C.M., et. al.: Detection of renal lesion enhancement with dual-energy multidetector CT. Radiology 2011; 259: pp. 173-183.
45. Massoud T.F.: Molecular imaging in living subjects: seeing fundamental biological processes in a new light. Genes Develop 2003; 17: pp. 545-580.
46. Contag C.H.: In vivo pathology: seeing with molecular specificity and cellular resolution in the living body. Annu Rev Pathol Mech Dis 2007; 2: pp. 277-305.
47. Miller J.C., Thrall J.H.: Clinical molecular imaging. J Am Coll Radiol 2004; 1: pp. 4-23.
48. Weissleder R., Mahmood U.: Molecular imaging. Radiology 2001; 219: pp. 316-333.
49. Margulis A.R.: Molecular imaging: love it or lose it. Radiology 2012; 264: pp. 5.
50. Nathan D.G., Varmus H.E.: The National Institutes of Health and clinical research: a progress report. Nat Med 2000; 6: pp. 1201-1204.
51. Lee C.I., Forman H.P.: What we can and cannot see coming. Radiology 2010; 257: pp. 313-314.
52. Budoff M.J., Hamirani Y.S., Gao Y.L., et. al.: Measurement of thoracic bone mineral density with quantitative CT. Radiology 2010; 257: pp. 434-440.
53. Shemesh J., Henschke C.I., Shaham D., et. al.: Ordinal scoring of coronary artery calcifications on low-dose CT scans of the chest is predictive of death from cardiovascular disease. Radiology 2010; 257: pp. 541-548.
54. Gondrie M.J., Mali W.P., Jacobs P.C., et. al.: Cardiovascular disease: prediction with ancillary aortic findings on chest CT scans in routine practice. Radiology 2010; 257: pp. 549-559.
55. Krestin G.P.: Maintaining identity in a changing environment: the professional and organizational future of radiology. Radiology 2009; 250: pp. 612-617.
56. Arenson R., Dunnick N.R.: Training a better radiologist. J Am Coll Radiol 2006; 3: pp. 389-393.
57. Campbell E.G., Weissman J.S., Blumenthal D.: Relationship between market competition and the activities and attitudes of medical school faculty. JAMA 1997; 278: pp. 222-226.
58. Enzmann D.R., Schomer D.F.: Analysis of radiology business models. J Am Coll Radiol 2012; 10: pp. 175-180.
59. Levin D.C., Rao V.M.: Turf wars in radiology: introduction. J Am Coll Radiol 2004; 1: pp. 23-25.
60. Levin D.C., Rao V.M.: Turf wars in radiology: the overutilization of imaging resulting from self-referral. J Am Coll Radiol 2004; 1: pp. 169-172.
61. Hendee W.R.: An opportunity for radiology. Radiology 2006; 238: pp. 389-394.
62. Amis E.S., Dunnick N.R.: Improvement in radiology education: joint efforts of the American Board of Radiology and the Diagnostic Radiology Residency Review Committee. J Am Coll Radiol 2009; 6: pp. 103-105.
63. Breslau J., Lexa F.J.: A radiologist’s primer on accountable care organizations. J Am Coll Radiol 2011; 8: pp. 164-168.
64. Nachiappan A.C., Wynne D.M., Katz D.P., et. al.: A proposed medical physics curriculum: preparing for the 2013 ABR examination. J Am Coll Radiol 2011; 8: pp. 53-57.
65. Nachiappan A.C., Lee S.R., Willis M.H., et. al.: Clinically oriented three-year medical physics curriculum: a new design for the future. AJR Am J Roentgenol 2012; 199: pp. 635-643.
66. Shortell S.M., Casalino L.P., Fisher E.S.: How the center for Medicare and Medicaid innovation should test accountable care organizations. Health Aff (Millwood) 2010; 29: pp. 1293-1298.
67. Bernardy M., Ullrich C.G., Rawson J.V., et. al.: Strategies for managing imaging utilization. J Am Coll Radiol 2009; 6: pp. 844-850.
68. Hillman B.J., Goldsmith J.C.: The uncritical use of high-tech medical imaging. N Engl J Med 2010; 363: pp. 4-6.
69. Levin D.C., Rao V.M.: Turf wars in radiology: updated evidence on the relationship between self-referral and the overutilization of imaging. J Am Coll Radiol 2008; 5: pp. 806-810.
70. Hillman B.J., Joseph C.A., Mabry M.R., et. al.: Frequency and costs of diagnostic imaging in office practice–a comparison of self-referring and radiologist-referring physicians. N Engl J Med 1990; 323: pp. 1604-1608.
71. Berbaum K.S., Franken E.A., el-Khoury G.Y.: Impact of clinical history on radiographic detection of fractures: a comparison of radiologists and orthopedists. AJR Am J Roentgenol 1989; 153: pp. 1221-1224.
72. Loy C.T., Irwig L.: Accuracy of diagnostic tests read with and without clinical information: a systematic review. JAMA 2004; 292: pp. 1602-1609.
73. Mullins M.E., Lev M.H., Schellingerhout D., et. al.: Influence of availability of clinical history on detection of early stroke using unenhanced CT and diffusion-weighted MR imaging. AJR Am J Roentgenol 2002; 179: pp. 223-228.
74. Chiunda A.B., Mohammed T.L.: Knowledge of ACR thoracic imaging Appropriateness Criteria(R) among trainees: one institution’s experience. Acad Radiol 2012; 19: pp. 635-639.
75. Bautista A.B., Burgos A., Nickel B.J., et. al.: Do clinicians use the American College of Radiology appropriateness criteria in the management of their patients?. AJR Am J Roentgenol 2009; 192: pp. 1581-1585.
76. Blackmore C.C., Mecklenburg R.S., Kaplan G.S.: Effectiveness of clinical decision support in controlling inappropriate imaging. J Am Coll Radiol 2011; 8: pp. 19-25.
77. Georgiou A., Prgomet M., Markewycz A., et. al.: The impact of computerized provider order entry systems on medical-imaging services: a systematic review. J Am Med Inform Assoc 2011; 18: pp. 335-340.
78. Sanders D.L., Miller R.A.: The effects on clinician ordering patterns of a computerized decision support system for neuroradiology imaging studies. Proc AMIA Symp 2001; pp. 583-587.
79. Cascade P.N.: The American College of Radiology. ACR Appropriateness Criteria project. Radiology 2000; 214: pp. 3-46.
80. Khorasani R., Silverman S.G., Meyer J.E., et. al.: Design and implementation of a new radiology consultation service in a teaching hospital. AJR Am J Roentgenol 1994; 163: pp. 457-459.
81. Basu P.A., Ruiz-Wibbelsmann J.A., Spielman S.B., et. al.: Creating a patient-centered imaging service: determining what patients want. AJR Am J Roentgenol 2011; 196: pp. 605-610.
82. Berlin L.: Communicating results of all radiologic examinations directly to patients: has the time come?. AJR Am J Roentgenol 2007; 189: pp. 1275-1282.
83. Berlin L.: Communicating results of all outpatient radiologic examinations directly to patients: the time has come. AJR Am J Roentgenol 2009; 192: pp. 571-573.
84. Brandt-Zawadski M., Kerlan R.K.: Patient-centered radiology: use it or lose it!. Acad Radiol 2009; 16: pp. 521-523.
85. Kuhlman M., Meyer M., Krupinski E.A.: Direct reporting of results to patients: the future of radiology?. Acad Radiol 2012; 19: pp. 646-650.
86. Margulis A.R., Sostman H.D.: Radiologist-patient contact during the performance of cross-sectional examinations. J Am Coll Radiol 2004; 1: pp. 162-163.
87. Berlin L.: Failure of radiologic communication: an increasing cause of malpractice litigation and harm to patients. App Radiol 2010; 39: pp. 17-23.
88. Yetisgen-Yildiz M., Gunn M.L., Xia F., et. al.: Automatic identification of critical follow-up recommendation sentences in radiology reports. AMIA Annu Symp Proc 2011; 2011: pp. 1593-1602.
89. Radiology and primary care in Europe. Insights imaging 2010; 1: pp. 46-52.
90. Apthorp L.A., Daly C.A., Morrison I.D., et. al.: Direct access MRI for general practitioners–influence on patient management. Clin Radiol 1998; 53: pp. 58-60.
91. Knechtges P.M., Carlos R.C.: The evolving role of radiologists within the health care system. J Am Coll Radiol 2007; 4: pp. 626-635.
92. Royal College of General Practitioners: Clinical radiology and the patients of general practitioners: joint statement of the Royal College of General Practitioners and Royal College of Radiology.2004.The Royal College of RadiologistsLondon, UK