Rationale and Objectives
Severe progressive multifocal heterotopic ossification (HO) is a rare occurrence seen predominantly in patients who have fibrodysplasia ossificans progressiva (FOP) and is difficult to quantitate owing to patient-, disease-, logistical-, and radiation-related issues. The purpose of this study was to develop and validate a scoring system based on plain radiographs for quantitative assessment of HO lesions in patients with FOP.
Materials and Methods
Institutional review board approval was obtained from the University of Pennsylvania, and all data comply with Health Insurance Portability and Accountability Act regulations. The University of Pennsylvania Institutional Animal Care and Use Committee approved the use of mice in this study. First, we used a mouse model of FOP-like HO to validate a semiquantitative analog scale for estimating relative heterotopic bone volume. Second, we used this validated scale to estimate the relative amount of HO from a retrospective analysis of plain radiographs from 63 patients with classic FOP. Finally, the scale was applied to a retrospective analysis of computed tomographic images from three patients with FOP.
Results
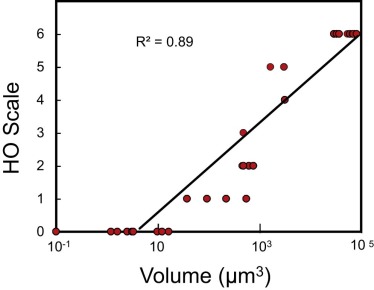
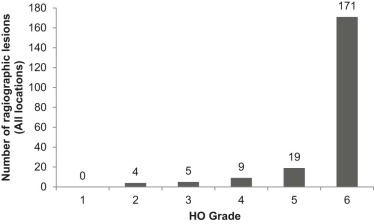
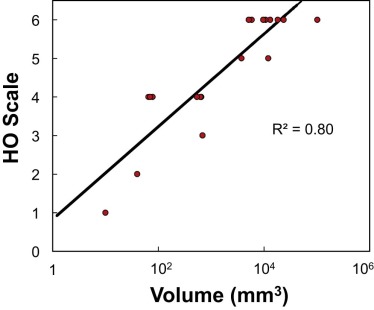
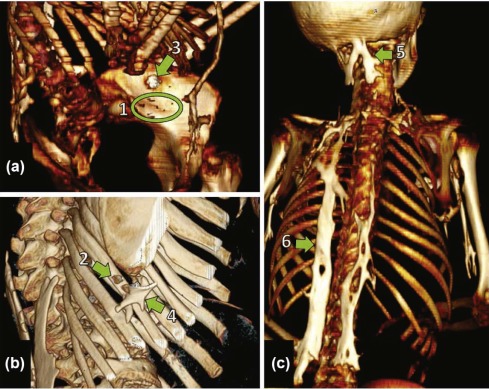
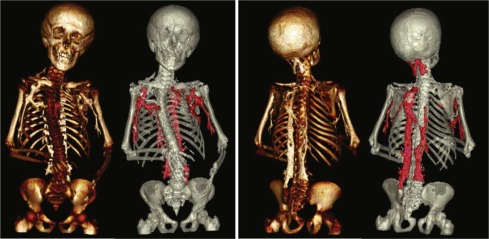
In the FOP-mouse model, the observed rating on the analog scale is highly correlated to heterotopic bone volumes measured by microcomputed tomography ( R 2 = 0.89). The scoring system that was applied to radiographs of patients with FOP captured the clinical range of HO typically present at all axial and appendicular sites. Analysis of computed tomographic scans of patients with FOP found that observed radiograph ratings were highly correlated with HO volume ( R 2 = 0.80).
Conclusions
The scoring system described here could enable practical, quantitative assessment of HO in clinical trials to evaluate new treatment modalities, especially for FOP. The development of the six-point analog scale described here provides and validates a much-needed, reproducible, and quantifiable method for describing and assessing HO in patients with FOP. This scale has the potential to be a key descriptor that can inform patients with FOP and clinicians about disease progression and response of HO lesions to interventions and treatments.
Introduction
Fibrodysplasia ossificans progressiva (FOP) (Mendelian Inheritance in Man #135100) is a severely disabling heritable disorder characterized by congenital malformations of the great toes and progressive heterotopic ossification (HO) that forms qualitatively normal bone at extraskeletal sites . During the first decade of life, affected children experience episodic exacerbations of painful soft tissue swellings (flare-ups), often precipitated by soft tissue injury, intramuscular injections, viral infection, muscular stretching, falls, or muscular fatigue . These flare-ups transform skeletal muscles, tendons, ligaments, fascia, and aponeuroses into heterotopic bone, rendering movement restricted or impossible. Classic FOP is caused by a recurrent activating mutation (c.617G>A; R206H) in the gene encoding activin A receptor type I/activin-like kinase 2 ( ACVR1/ALK2 ), a bone morphogenetic protein type I receptor . At present, there is no definitive treatment, but emerging drug development offers the possibility of beneficial interventions .
Although multiple classification systems grade the severity of focal HO , none is applicable to progressive multifocal HO, nor does any adequately measure volumetric bone by plain radiographs. A simple method for quantifying extraskeletal bone formation would be useful to assess the effectiveness of evolving treatments, especially for FOP, where rigid immobility because of progressive multifocal HO often precludes serial quantitative computed tomographic (CT) scans at major urban medical centers.
Get Radiology Tree app to read full this article<
Table 1
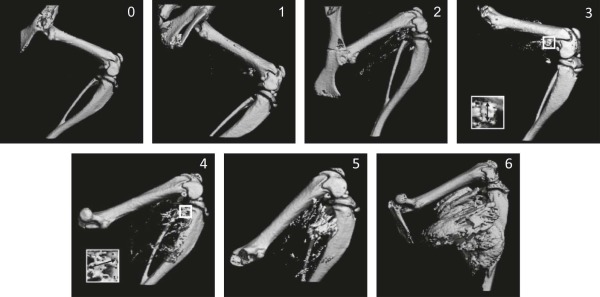
Analog Scale to Measure HO on Plain Radiographs in Patients with FOP \*
0 No HO 1 Single or multiple spicules (punctate) or islands (non-contiguous) of HO 2 Coalescing islands or reticular complexes of heterotopic bone 3 Single contiguous HO having longest dimension ≤one-half of the diameter of the reference normotopic bone \\ in any projection 4 Single contiguous HO with longest dimension >one-half but ≤1 of the diameter of the reference normotopic bone \\ in any projection 5 Single contiguous HO with longest dimension >1 but ≤2 of the diameter of reference normotopic bone \* in any projection 6 Single contiguous HO with longest dimension >2 diameters of reference normotopic bone \\ in any projection
HO, heterotopic ossification.
Ankle, tibial shaft; back or chest, height of cervical vertebral body nearest to HO midpoint; Distal lower extremity, tibial shaft; Distal upper extremity, radial shaft; Foot, metatarsal; Hip or proximal lower extremity, width of femoral neck; Jaw or chin, width of hyoid; Knee, femoral shaft; Neck, height of cervical vertebral body nearest to HO midpoint (lateral projection); Proximal upper extremity, humeral shaft; TMJ, height of cervical vertebral body nearest to HO midpoint.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Materials and Methods
Animals and Injury-induced HO Model
Get Radiology Tree app to read full this article<
Microcomputed Tomography
Get Radiology Tree app to read full this article<
Patients
Get Radiology Tree app to read full this article<
Assessment of Radiographs
Get Radiology Tree app to read full this article<
Clinical CT Imaging and HO Volume Analysis
Get Radiology Tree app to read full this article<
HO Scoring System
Get Radiology Tree app to read full this article<
Statistics
Get Radiology Tree app to read full this article<
Results
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Table 2
Localization and Grading of Radiographic HO Lesions
HO Grade Totals by Location 1 2 3 4 5 6 Neck 2 21 23 Back or chest 1 1 47 49 Shoulders 3 5 4 49 61 Elbows 2 8 10 Wrists 0 Hips 1 3 8 27 39 Knees 1 12 13 Distal lower extremities (incl. ankles or feet) 2 3 1 7 13 Totals by grade 0 4 5 9 19 171 208
HO, heterotopic ossification.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Discussion
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Acknowledgments
Get Radiology Tree app to read full this article<
References
1. Pignolo R.J., Shore E.M., Kaplan F.S.: Fibrodysplasia ossificans progressiva: clinical and genetic aspects. Orphanet J Rare Dis 2011; 6: pp. 80.
2. Kaplan F.S., Le Merrer M., Glaser D.L., et. al.: Fibrodysplasia ossificans progressiva. Best Pract Res Clin Rheumatol 2008; 22: pp. 191-205.
3. Shore E.M., Xu M., Feldman G.J., et. al.: A recurrent mutation in the BMP type I receptor ACVR1 causes inherited and sporadic fibrodysplasia ossificans progressiva. Nat Genet 2006; 38: pp. 525-527.
4. Kan L., Lounev V.Y., Pignolo R.J., et. al.: Substance P signaling mediates BMP-dependent heterotopic ossification. J Cell Biochem 2011; 112: pp. 2759-2772.
5. Kaplan F.S., Glaser D.L., Pignolo R.J., et. al.: A new era for fibrodysplasia ossificans progressiva: a druggable target for the second skeleton. Expert Opin Biol Ther 2007; 7: pp. 705-712.
6. Shimono K., Tung W.E., Macolino C., et. al.: Potent inhibition of heterotopic ossification by nuclear retinoic acid receptor-gamma agonists. Nat Med 2011; 17: pp. 454-460.
7. Yu P.B., Deng D.Y., Lai C.S., et. al.: BMP type I receptor inhibition reduces heterotopic [corrected] ossification. Nat Med 2008; 14: pp. 1363-1369.
8. Hatsell S.J., Idone V., Wolken D.M., et. al.: ACVR1R206H receptor mutation causes fibrodysplasia ossificans progressiva by imparting responsiveness to activin A. Sci Transl Med 2015; 7: pp. 303ra137.
9. Brooker A.F., Bowerman J.W., Robinson R.A., et. al.: Ectopic ossification following total hip replacement. Incidence and a method of classification. J Bone Joint Surg Am 1973; 55: pp. 1629-1632.
10. Kawaguchi Y., Urushisaki A., Seki S., et. al.: Evaluation of ossification of the posterior longitudinal ligament by three-dimensional computed tomography and magnetic resonance imaging. Spine J 2011; 11: pp. 927-932.
11. Kocic M., Lazovic M., Mitkovic M., et. al.: Clinical significance of the heterotopic ossification after total hip arthroplasty. Orthopedics 2010; 33: pp. 16.
12. Mavrogenis A.F., Guerra G., Staals E.L., et. al.: A classification method for neurogenic heterotopic ossification of the hip. J Orthop Traumatol 2012; 13: pp. 69-78.
13. Schuh A., Zeiler G.: [The modified Brooker classification for evaluation of heterotopic ossifications in total hip replacement]. Zentralbl Chir 2005; 130: pp. 293-296.
14. Fukuda T., Scott G., Komatsu Y., et. al.: Generation of a mouse with conditionally activated signaling through the BMP receptor, ALK2. Genesis 2006; 44: pp. 159-167.
15. Brownley R.C., Agarwal S., Loder S., et. al.: Characterization of heterotopic ossification using radiographic imaging: evidence for a paradigm shift. PLoS ONE 2015; 10: pp. e0141432.
16. Kaplan F.S., Shore E.M., Pignolo R.J.: The medical management of fibrodysplasia ossificans progressiva: current treatment considerations. Clin Proc Intl Clin Consort FOP 2011; 4: pp. 1-100.
17. Kaplan F.S., Strear C.M., Zasloff M.A.: Radiographic and scintigraphic features of modeling and remodeling in the heterotopic skeleton of patients who have fibrodysplasia ossificans progressiva. Clin Orthop Relat Res 1994; 304: pp. 238-247.
18. Kaplan F.S., Xu M., Seemann P., et. al.: Classic and atypical fibrodysplasia ossificans progressiva (FOP) phenotypes are caused by mutations in the bone morphogenetic protein (BMP) type I receptor ACVR1. Hum Mutat 2009; 30: pp. 379-390.
19. Mahboubi S., Glaser D.L., Shore E.M., et. al.: Fibrodysplasia ossificans progressiva. Pediatr Radiol 2001; 31: pp. 307-314.