Rationale and Objectives
To evaluate interobserver agreement with the use of and the positive predictive value (PPV) of Prostate Imaging Reporting and Data System version 2 (PI-RADS v2) for the localization of intermediate- and high-grade prostate cancers on multiparametric magnetic resonance imaging (mpMRI).
Materials and Methods
In this retrospective, institutional review board-approved study, 131 consecutive patients who had mpMRI followed by transrectal ultrasound-MR imaging fusion-guided biopsy of the prostate were included. Two readers who were blinded to initial mpMRI reports, clinical data, and pathologic outcomes reviewed the MR images, identified all prostate lesions, and scored each lesion based on the PI-RADS v2. Interobserver agreement was assessed by intraclass correlation coefficient (ICC), and PPV was calculated for each PI-RADS category.
Results
PI-RADS v2 was found to have a moderate level of interobserver agreement between two readers of varying experience, with ICC of 0.74, 0.72, and 0.67 for all lesions, peripheral zone lesions, and transitional zone lesions, respectively. Despite only moderate interobserver agreement, the calculated PPV in the detection of intermediate- and high-grade prostate cancers for each PI-RADS category was very similar between the two readers, with approximate PPV of 0%, 12%, 64%, and 87% for PI-RADS categories 2, 3, 4, and 5, respectively.
Conclusions
In our study, PI-RADS v2 has only moderate interobserver agreement, a similar finding in studies of the original PI-RADS and in initial studies of PI-RADS v2. Despite this, PI-RADS v2 appears to be a useful system to predict significant prostate cancer, with PI-RADS scores correlating well with the likelihood of intermediate- and high-grade cancers.
Introduction
In an attempt to standardize image interpretation and reporting of multiparametric magnetic resonance imaging (mpMRI) of the prostate, the European Society of Urogenital Radiology published the first Prostate Imaging Reporting and Data System (PI-RADS 1.0) in 2012. PI-RADS 1.0 is based on assessment of T2-weighted MRI, diffusion weighted imaging (DWI), and dynamic contrast enhanced-MRI (DCE-MRI) with or without MR spectroscopy for each lesion according to a 5-point scale and assigning a sum score ranging from 3 to 15 without MR spectroscopy (MRS) and from 4 to 20 with MRS . Several studies have validated the original PI-RADS in terms of accuracy; however, interobserver agreement was only moderate . Recent studies also suggest that assigning a score for T2-weighted imaging (T2WI) to transitional zone lesions and for DWI to peripheral zone lesion is adequate for stratification of patients for further diagnostic workup . On the other hand, MRS was rarely used in recent studies, and DCE-MRI curve-type analysis does not seem to add significant value in the characterization of prostate lesions .
Based on these new data, the PI-RADS steering committee of the American College of Radiology and the European Society of Urogenital Radiology prostate MRI working group revised PI-RADS and published PI-RADS version 2.0 in early 2015 . In this new version of PI-RADS, a primary determinant MRI sequence is used to evaluate each prostate lesion based on location. For peripheral zone lesions, DWI is the dominant sequence, and for transitional zone lesions, T2-weighted sequence is the dominant sequence. On DCE-MRI, results are scored as positive or negative based on the presence or absence of focal early enhancement, and the previously used curve-type analysis was abandoned. DCE-MRI is used strictly for characterization of peripheral zone lesions and is applied only if it makes a clinically relevant difference in cases where a lesion is upgraded from PI-RADS 3 to 4. Finally, a final score of 1–5 is assigned to each prostate lesion based on the revised rules.
Get Radiology Tree app to read full this article<
Materials and Methods
Study Design and Patient Population
Get Radiology Tree app to read full this article<
MR Imaging Protocol
Get Radiology Tree app to read full this article<
TABLE 1
Magnetic Resonance Imaging Sequence Parameters
Parameter Repetition Time (ms) Echo Time (ms) Flip Angle (°) Slice Thickness (mm) Acquisition Matrix Imaging Time FOV (cm) NEX Scan Mode No. of Repetitions Repetition Time (s) T2WI 3427 102 180 4 320 × 320 5:11 20 4 Zoom – – T1WI 500 Minimum full 180 4 224 × 256 4:56 20 1 Zoom – – DWI 3800 Minimum full 180 4 128 × 128 2:24 20 1 (b value of 0)
12 (b value of 600)
1 (b value of 1000) Zoom – – DCE 3 Minimum full 15 4 160 × 160 6:07 20 1 Zoom 53 7
DCE, dynamic contrast-enhanced; DWI, diffusion weighted imaging; FOV, field of view; T1WI, T1-weighted imaging; T2WI, T2-weighted imaging.
Get Radiology Tree app to read full this article<
Prostate Biopsy
Get Radiology Tree app to read full this article<
MR Analysis
Get Radiology Tree app to read full this article<
Radiologic-Pathologic Correlation
Get Radiology Tree app to read full this article<
Statistical Analysis
Get Radiology Tree app to read full this article<
Results
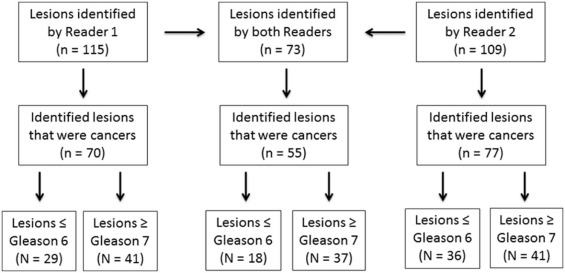
Lesion Characteristics
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Interobserver Agreement
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
TABLE 2
Interobserver Agreement—Intraclass Correlation Coefficient Based on Lesion Type
Lesion Type Intraclass Correlation Coefficient All 0.74 (95% CI: 0.60, 0.83) All PZ lesions 0.72 (95% CI: 0.56, 0.83) All TZ lesions 0.67 (95% CI: 0.22, 0.89) All intermediate- and high-grade lesions 0.60 (95% CI: 0.34, 0.78)
CI, confidence interval; PZ, peripheral zone; TZ, transitional zone.
Get Radiology Tree app to read full this article<
Positive Predictive Value
Get Radiology Tree app to read full this article<
TABLE 3
Positive Predictive Value for Each PI-RADS Score
PI-RADS Score PPV (%) Reader 1 2 0 3 13.0 (95% CI: 6.5, 23.8) 4 64.9 (95% CI: 47.4, 79.3) 5 88.9 (95% CI: 50.7, 99.4) Reader 2 2 0 3 11.9 (95% CI: 5.3, 23.5) 4 62.2 (95% CI: 44.8, 77.1) 5 84.6 (95% CI: 53.7, 97.3)
CI, confidence interval; PI-RADS, Prostate Imaging Reporting and Data System; PPV, positive predictive value.
Get Radiology Tree app to read full this article<
Discussion
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
References
1. Barentsz J.O., Richenberg J., Clements R., et. al.: ESUR prostate MR guidelines 2012. Eur Radiol 2012; 22: pp. 746-757.
2. Hamoen E.H., de Rooij M., Witjes J.A., et. al.: Use of the Prostate Imaging Reporting and Data System (PI-RADS) for prostate cancer detection with multiparametric magnetic resonance imaging: a diagnostic meta-analysis. Eur Urol 2015; 67: pp. 1112-1121.
3. Renard-Penna R., Mozer P., Cornud F., et. al.: Prostate imaging reporting and data system and Likert scoring system: multiparametric MR imaging validation study to screen patients for initial biopsy. Radiology 2015; 275: pp. 458-468.
4. Vache T., Bratan F., Mege-Lechevallier F., et. al.: Characterization of prostate lesions as benign or malignant at multiparametric MR imaging: comparison of three scoring systems in patients treated with radical prostatectomy. Radiology 2014; 272: pp. 446-455.
5. Thompson J.E., van Leeuwen P.J., Moses D., et. al.: The diagnostic performance of multiparametric magnetic resonance imaging to detect significant prostate cancer. J Urol 2015; 195: pp. 1428-1435.
6. Baur A.D., Maxeiner A., Franiel T., et. al.: Evaluation of the prostate imaging reporting and data system for the detection of prostate cancer by the results of targeted biopsy of the prostate. Invest Radiol 2014; 49: pp. 411-420.
7. Junker D., Quentin M., Nagele U., et. al.: Evaluation of the PI-RADS scoring system for mpMRI of the prostate: a whole-mount step-section analysis. World J Urol 2015; 33: pp. 1023-1030.
8. Hansford B.G., Peng Y., Jiang Y., et. al.: Dynamic contrast-enhanced MR imaging curve-type analysis: is it helpful in the differentiation of prostate cancer from healthy peripheral zone?. Radiology 2015; 275: pp. 448-457.
9. American College of Radiology : PIRADS v2. Reston, VA: American College of Radiology2014.
10. Ukimura O., Desai M.M., et. al., Palmer S: 3-Dimensional elastic registration system of prostate biopsy location by real-time 3-dimensional transrectal ultrasound guidance with magnetic resonance/transrectal ultrasound image fusion. J Urol 2012; 187: pp. 1080-1086.
11. Baco E., Ukimura O., Rud E., et. al.: Magnetic resonance imaging-transrectal ultrasound image-fusion biopsies accurately characterize the index tumor: correlation with step-sectioned radical prostatectomy specimens in 135 patients. Eur Urol 2015; 67: pp. 787-794.
12. Vaché T., Bratan F., Mège-Lechevallier F., et. al.: Characterization of prostate lesions as benign or malignant at multiparametric MR imaging: comparison of three scoring systems in patients treated with radical prostatectomy. Radiology 2014; 272: pp. 446-455.
13. Schimmöller L., Quentin M., Arsov C., et. al.: Inter-reader agreement of the ESUR score for prostate MRI using in-bore MRI-guided biopsies as the reference standard. Eur Radiol 2013; 23: pp. 3185-3190.
14. Renard-Penna R., Mozer P., Cornud F., et. al.: Prostate imaging reporting and data system and Likert scoring system: multiparametric MR imaging validating study to screen patients for initial biopsy. Radiology 2015; 275: pp. 458-468.
15. Muller B.G., Shih J.H., Sankineni S., et. al.: Prostate cancer: interobserver agreement and accuracy with the revised prostate imaging reporting and data system at multiparametric MR imaging. Radiology 2015; 277: pp. 741-750.
16. Rosenkrantz A.B., Ginocchio L.A., Cornfeld D., et. al.: Interobserver reproducibility of the PI-RADS version 2 lexicon: a multicenter study of six experienced prostate radiologists. Radiology 2016; 280: pp. 793-804.
17. Vargas H.A., Hotker A.M., Goldman D.A., et. al.: Updated prostate imaging reporting and data system (PIRADS v2) recommendations for the detection of clinically significant prostate cancer using multiparametric MRI: critical evaluation using whole-mount pathology as standard of reference. Eur Radiol 2016; 26: pp. 1606-1612.
18. NiMhurchu E., O’Kelly F., Murphy I.G., et. al.: Predictive value of PI-RADS classification in MRI-directed transrectal ultrasound guided prostate biopsy. Clin Radiol 2016; 71: pp. 375-380.