Rationale and Objectives
As both contrast and radiation dose affect the quality of CT images, a constant image quality in abdominal contrast-enhanced multidetector computed tomography (CE-MDCT) could be obtained balancing radiation and contrast media dose according to the age of the patients.
Materials and Methods
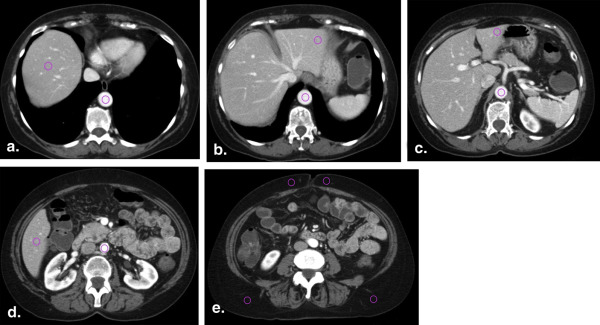
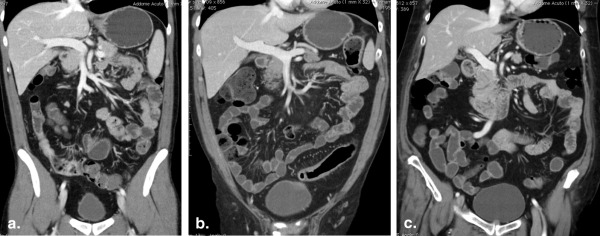
Seventy-two (38 Men; 34 women; aged 20–83 years) patients underwent a single-pass abdominal CE-MDCT. Patients were divided into three different age groups: A (20–44 years); B (45–65 years); and C (>65 years). For each group, a different noise index (NI) and contrast media dose (370 mgI/mL) was selected as follows: A (NI, 15; 2.5 mL/kg), B (NI, 12.5; 2 mL/kg), and C (NI, 10; 1.5 mL/kg). Radiation exposure was reported as dose–length product (DLP) in mGy × cm. For quantitative analysis, signal-to-noise (SNR) and contrast-to-noise (CNR) ratios were calculated for both the liver (L) and the abdominal aorta (A). Statistical analysis was performed with a one-way analysis of variance. Standard imaging criteria were used for qualitative analysis.
Results
Although peak hepatic enhancement was 152 ± 16, 128 ± 12, and 101 ± 14 Hounsfield units ( P < .001) for groups A, B, and C, respectively, no significant differences were observed in the corresponding SNR L with 9.2 ± 1.4, 9.1 ± 1.2, and 9.2 ± 3. Radiation (mGy × cm) and contrast media dose (mL) administered were 476 ± 147 and 155 ± 27 for group A, 926 ± 291 and 130 ± 16 for group B, and 1981 ± 451 and 106 ± 15 for group C, respectively ( P < .001). None of the studies was graded as poor or inadequate by both readers, and the prevalence-adjusted bias-adjusted kappa ranged between 0.48 and 0.93 for all but one criteria.
Conclusions
A constant image quality in CE-MDCT can be obtained balancing radiation and contrast media dose administered to patients of different age.
As radiation exposure resulting from multidetector computed tomography (MDCT) technology has become a major issue in the radiologic community, radiologists should accept the primary responsibility of minimizing the radiation dose delivered to patients while preserving the image quality and diagnostic efficacy of the CT examination . As the lifetime risk of radiation-induced cancer is greater the younger is the patient at the time of exposure, this radiation consciousness should be greatest with patients aged <30 years .
Several technical and electronic dose reduction strategies have been developed and successfully applied in clinical practice such as the automatic tube current modulation and the use of iterative reconstruction algorithms in place of the filtered back projection . Moreover, with the advent of dual-source CT, the effect of low-kilovoltage protocols on radiation dose and image quality has also been investigated . In particular, it has been shown that a significant reduction of the radiation dose with an acceptable image quality can be obtained by coupling the reduction of the peak kilovoltage with the use of adaptive iterative reconstruction algorithms .
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Materials and methods
Population
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
CT Technique
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Tdelay=CI+25−TSD T
d
e
l
a
y
=
C
I
+
25
−
T
S
D
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Image Analysis
Get Radiology Tree app to read full this article<
Quantitative Analysis
Get Radiology Tree app to read full this article<
SNRL=μL/meanSDL;SNRA=μA/meanSDA. S
N
R
L
=
μ
L
/
m
e
a
n
S
D
L
;
S
N
R
A
=
μ
A
/
m
e
a
n
S
D
A
.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
CNRL=(μL−μF)/σ;CNRA=(μA−μF)/σ C
N
R
L
=
(
μ
L
−
μ
F
)
/
σ
;
C
N
R
A
=
(
μ
A
−
μ
F
)
/
σ
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
FOML=CNR2L/ED F
O
M
L
=
C
N
R
L
2
/
E
D
Get Radiology Tree app to read full this article<
Qualitative Analysis
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Statistical Analysis
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Results
Patient Characteristics
Get Radiology Tree app to read full this article<
Table 1
Patient Characteristics
Characteristic Group A ( n = 27) Group B ( n = 28) Group C ( n = 17)P Value Age (years) 20–44 (35 ± 9) 45–65 (56 ± 8) >65 (74 ± 7) — Gender M ( n = 14); F ( n = 13) M ( n = 14); F ( n = 14) M ( n = 10); F ( n = 7) — Weight (kg) 62 ± 12 65 ± 9 71 ± 10 NS Height (cm) 167 ± 9 165 ± 7 167 ± 8 NS BMI (kg/m 2 ) 21.6 ± 3 24 ± 2 26 ± 4 NS GFR (mL/min) 106 ± 25 98 ± 40 41 ± 13 <.01 Creatinine (mg/mL) 0.84 ± 0.16 0.80 ± 0.23 1.65 ± 0.42 <.01
BMI, body mass index; F, female; GFR, glomerular filtration rate; M, male; NS, not significant.
Get Radiology Tree app to read full this article<
Nonionic Iodinated Contrast Media
Get Radiology Tree app to read full this article<
Table 2
Dose–Length Products (DLP), Effective Doses (ED), Volumes of Contrast Media (CM) Injected, Iodine Loads, and Scan Delays of the CT Acquisition Performed in Each Group
Parameter Group A Group B Group C_P_ Value DLP (mGy *cm) 476 ± 147 926 ± 291 1981 ± 451 <.001 ED (mSv) 7.1 ± 2.2 13.9 ± 4.3 29.7 ± 6.7 <.001 CM (cc) 155 ± 27 130 ± 16 106 ± 15 <.001 Iodine load (g) 58 ± 11 49 ± 6 39 ± 5 <.001 Scan delay (s) 77 ± 7 78 ± 6 82 ± 8 NS
NS, not significant.
Get Radiology Tree app to read full this article<
Effective Absorbed Dose
Get Radiology Tree app to read full this article<
Scan Delays
Get Radiology Tree app to read full this article<
Quantitative Image Analysis
Get Radiology Tree app to read full this article<
Table 3
Mean Attenuation Values (HU), Contrast-to-Noise Ratios (CNR), and Signal-to-Noise Ratios (SNR) for Liver ( L ) and Abdominal Aorta ( A ) Are Shown Along with the Figure of Merit for CNR L and the Image Noise (σ) for Each Group
Parameter Group A Group B Group C_P_ Value Mean liver (HU) 152 ± 16 128 ± 12 101 ± 14 <.01 CNR L 16.7 ± 2 18.8 ± 3 21.7 ± 4.4 <.01 SNR L 9.2 ± 1.4 9.1 ± 1.2 9.2 ± 3 NS FOM 41.8 ± 17 30 ± 17 16 ± 6 <.001 Mean aorta (HU) 221 ± 23 224 ± 51 205 ± 35 NS CNR A 21 ± 2.4 26.6 ± 5.5 32 ± 6 <.01 SNR A 12 ± 2.4 14.5 ± 3.3 17.4 ± 5.5 <.01 Sigma (σ) 15 ± 0.6 12 ± 0.5 10 ± 1.7 <.01
HU, Hounsfield unit; NS, not significant.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
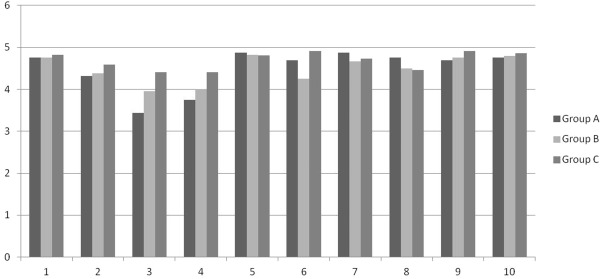
Qualitative Image Analysis
Get Radiology Tree app to read full this article<
Table 4
Qualitative Analysis: Prevalence-Adjusted Bias-Adjusted Kappa (PABAK) and Grade of Interobserver Agreement for Each Image Quality Criteria Are Shown
Sharp Reproduction PABAK Agreement Intrahepatic portal veins 0.81 Almost perfect Hepatic veins 0.81 Almost perfect CBD 0.29 Fair CBD in the pancreas 0.48 Moderate Gallbladder walls 0.93 Almost perfect Splenic artery 0.5 Moderate Portal vein and SMV 0.75 Substantial Aorta and IVC 0.87 Almost perfect Coeliac trunk 0.87 Almost perfect SMA 0.81 Almost perfect
CBD, common biliary duct; IVC, inferior vena cava; SMA, superior mesenteric artery; SMV, superior mesenteric vein.
Get Radiology Tree app to read full this article<
Discussion
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Acknowledgment
Get Radiology Tree app to read full this article<
References
1. Thrall J.H.: Radiation exposure in CT scanning and risk: where are we?. Radiology 2012; 264: pp. 325-328.
2. Brenner D.J., Hall E.J.: Computed tomography: an increasing source of radiation exposure. N Engl J Med 2007; 357: pp. 2277-2284.
3. Rizzo S., Kalra M., Schmidt B., et. al.: Comparison of angular and combined automated tube current modulation techniques with constant tube current CT of abdomen and pelvis. AJR Am J Roentgenol 2006; 186: pp. 673-679.
4. Silva A.C., Lawder H.J., Hara A., et. al.: Innovations in CT dose reduction strategy: application of the adaptive statistical iterative reconstruction algorithm. AJR Am J Roentgenol 2010; 194: pp. 191-199.
5. Hough D.M., Fletcher J.C., Grant K.L., et. al.: Lowering kilo-voltage to reduce radiation dose in contrast enhanced abdominal CT: initial assessment of a prototype automated kilo-voltage selection tool. AJR Am J Roentgenol 2012; 199: pp. 1070-1077.
6. Nakaura T., Nakamura S., Maruyama N., et. al.: Low contrast agent and radiation dose protocol for hepatic dynamic CT of thin adults at 256-detector row CT: effect of low tube voltage and hybrid iterative reconstruction algorithm on image quality. Radiology 2012; 264: pp. 445-454.
7. Kaza R.K., Plat J.F., Al-Hawary M.M., et. al.: CT enterography at 80 kVp with adaptive statistical iterative reconstruction versus at 120 kVp with standard reconstruction: image quality, diagnostic adequacy and dose reduction. AJR Am J Roentgenol 2012; 198: pp. 1084-1092.
8. Itatani R., Oda S., Utsunomiya D., et. al.: Reduction in radiation and contrast medium dose via optimization of low-kilovoltage CT protocols using a hybrid iterative reconstruction algorithm at 256-slice body CT: Phantom study and clinical correlation. Clin Radiol 2013; 68: pp. 128-135.
9. Watanabe H., Kanematsu M., Miyoshi T., et. al.: Improvement of image quality of low radiation dose abdominal CT by increasing contrast enhancement. AJR Am J Roentgenol 2010; 195: pp. 986-992.
10. Falt T., Soderberg M., Horberg L., et. al.: Seesaw balancing radiation dose and IV contrast dose: evaluation of a new abdominal CT protocol for reducing age-specific risk. AJR Am J Roentgenol 2013; 200: pp. 383-388.
11. Coakley F.V., Gould R., Yeh B.M., et. al.: CT radiation dose: what can you do right now in your practice?. AJR Am J Roentgenol 2011; 196: pp. 619-625.
12. Johnson P.T., Fishman E.K.: Routine use of pre-contrast and delayed acquisitions in abdominal CT: time for change. Abdom Imaging 2013; 38: pp. 215-223.
13. Fletcher J.G.: CT enterography: theme and variations. Abdom Imaging 2009; 34: pp. 283-288.
14. Bae K.T.: Intravenous contrast medium administration and scan timing at CT: considerations and approaches. Radiology 2010; 256: pp. 32-61.
15. Kondo H., Kanematsu M., Goshima S., et. al.: Body size indices to determine iodine mass with contrast-enhanced multi-detector computed tomography of the upper abdomen: does body surface area outperform total body weight or lean body weight?. Eur Radiol 2013; 23: pp. 1855-1861.
16. van der Molen A.J., Thomsen H.S., Morcos S.K.: Effect of iodinated contrast media on thyroid function in adults. Eur Radiol 2004; 14: pp. 902-907.
17. Stacul F., van der Molen A.J., Reimer P., et. al.: Contrast induced nephropathy: updated ESUR contrast media safety committee guidelines. Eur Radiol 2011; 21: pp. 2527-2541.
18. Marin D., Nelson R.C., Schindera S.T., et. al.: Low-tube-voltage, high-tube-current multi-detector abdominal CT: improved image quality and decreased radiation dose with adaptive statistical iterative reconstruction algorithm-initial clinical experience. Radiology 2010; 254: pp. 145-153.
19. Bongartz G., Golding S.J., Jurik A.G., et. al.: European Guidelines on quality criteria for Computed Tomography. Report EUR 16262.1999.European CommissionLuxembourg
20. Sim J., Wright C.C.: The kappa statistic in reliability studies: use, interpretation and sample size requirements. Phys Ther 2005; 85: pp. 257-268.
21. Cicchetti D.V., Alvan R.: High agreement but low kappa: II. Resolving the paradoxes. J Clin Epidemiol 1990; 43: pp. 551-558.
22. Hough D.M., Yu L., Shiung M.M., et. al.: Individualization of abdominopelvic CT protocols with lower tube voltage to reduce IV contrast dose or radiation dose. AJR Am J Roentgenol 2013; 201: pp. 147-153.
23. Maldijan P.D., Goldman A.R.: Reducing radiation dose in body CT: a primer on dose metrics and key CT technical parameters. AJR Am J Roentgenol 2013; 200: pp. 741-747.
24. Yamashita Y., Komohara Y., Takahashi M., et. al.: Abdominal helical CT: evaluation of optimal doses of intravenous contrast material—a prospective randomized study. Radiology 2000; 216: pp. 718-723.
25. Ploussi A., Alexopoulou E., Economopoulos N., et. al.: Patient radiation exposure and image quality evaluation with the use of iDose 4 iterative reconstruction algorithm in chest-abdomen-pelvis CT examinations. Radiat Prot Dosimetry 2014; 158: pp. 399-405.
26. Kalra M.K., Maher M.M., Sahani D.V., et. al.: Low-dose of the abdomen: evaluation of image improvement with use of noise reduction filters—pilot study. Radiology 2003; 228: pp. 251-256.
27. Kalra M.K., Maher M.M., Toth T.L., et. al.: Techniques and applications of automated tube current modulation for CT. Radiology 2004; 233: pp. 649-657.
28. Guite K.M., Hinshaw J.L., Ranallo F.N., et. al.: Ionizing radiation in abdominal CT: unindicated multiphase scans are an important source of medically unnecessary exposure. J Am Coll Radiol 2011; 8: pp. 756-761.