Rationale and Objectives
Breast cancer is the leading cause of mortality in women worldwide. Lymphatic mapping with sentinel node biopsy has the potential to reduce the morbidity associated with breast cancer staging in women after neoadjuvant therapy.
Materials and Methods
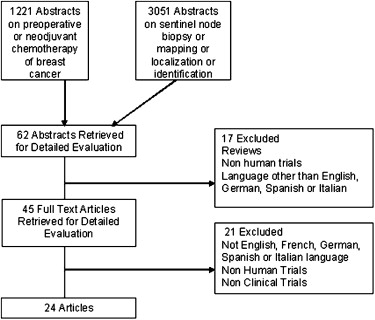
A systematic search of world literature between 1996 and 2007 of sentinel node mapping in patients with early-stage breast carcinoma after chemotherapy was undertaken. Potentially eligible studies were identified using database-specific search strategies incorporating appropriate Boolean combinations of the keywords sentinel node biopsy or sentinel node localization or lymphatic mapping; breast cancer or malignancy or neoplasm; and preoperative or neoadjuvant chemotherapy. The electronic searches were augmented with a manual search of reference lists from identified articles. Successful lymph node mapping, defined as successful identification rate (SIR), and false-negative rate (FNR) was summarized using a bivariate random effects mixed model. The extent of heterogeneity was assessed using the inconsistency statistic. The effect of study level covariates, such as use of immunohistochemistry or dual mapping technique, and individual quality criteria, such as study design or multi-institution participation, on SIR and FNR were analyzed using metaregression.
Results
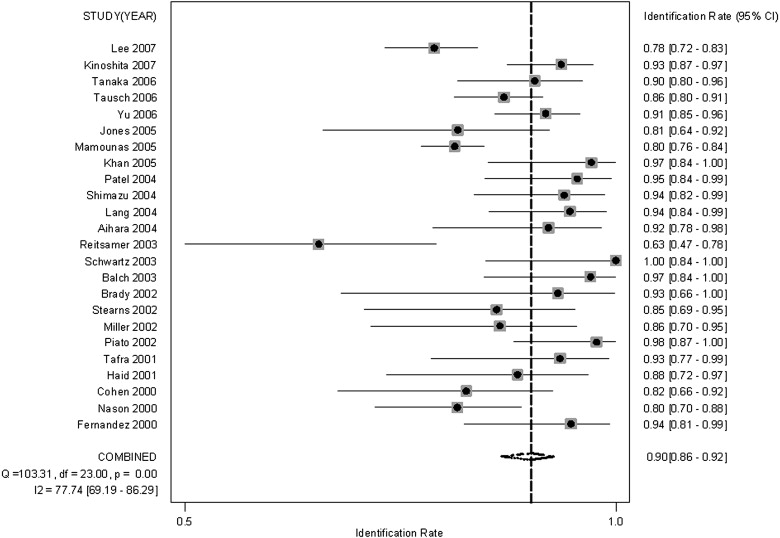
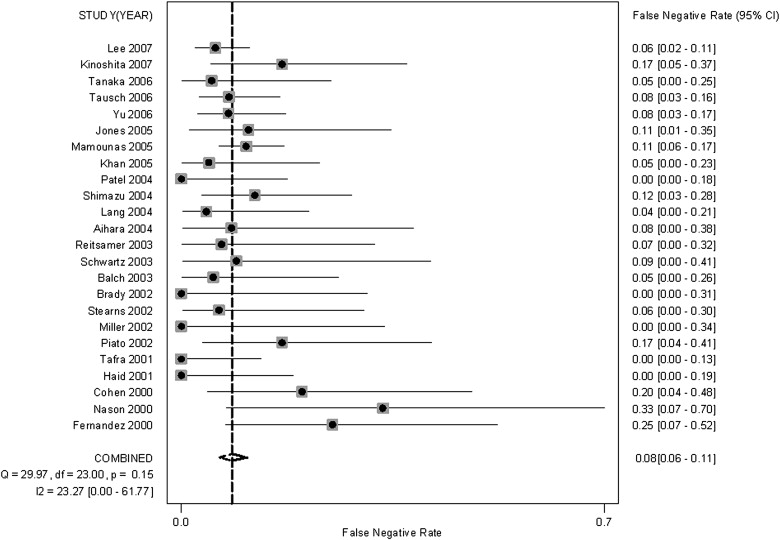
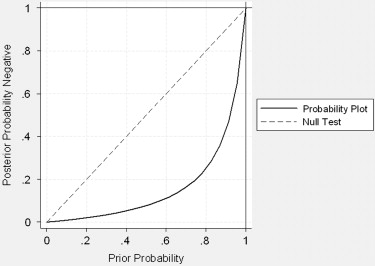
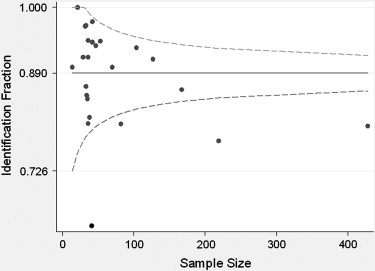
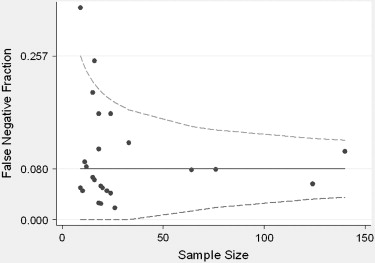
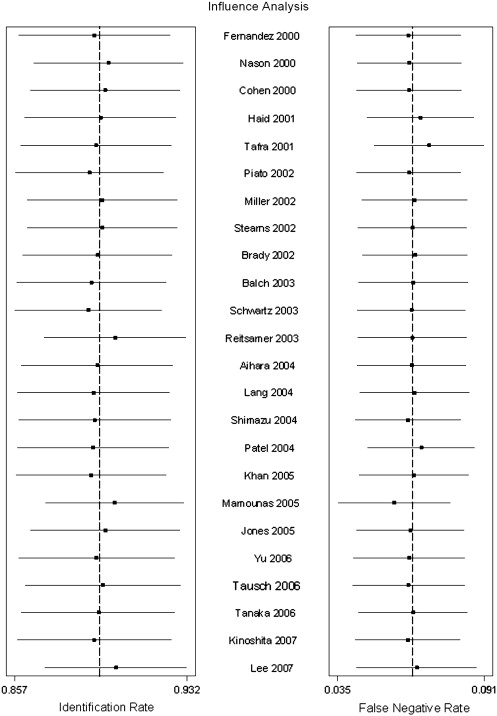
A total of 24 trials of 1799 subjects were reported that met eligibility criteria. All studies identified were published between 2000 and 2007. Lymph node involvement was found in 758 patients (37%) and ranged from 25% to 96% across studies. The proportion of patients who had successful lymph node mapping ranged from 63% to 100%, with 79% of studies reporting a rate of less than 95%. The summary successful identification rate was 0.896 (95% confidence interval [CI] 0.860–0.923) with moderate heterogeneity. The summary FNR was 0.084 (95% CI 0.064–0.109) with no significant heterogeneity. Increasing prevalence of lymph node involvement and same-day mapping and lymph node dissection both significantly reduced the FNR.
Conclusions
The present systematic review demonstrates robust estimates of successful identification rate and false-negative rates of sentinel lymph node mapping and biopsy after neoadjuvant therapy for early-stage breast cancer patients. With a 90% SIR and 8% FNR, this technique is a reliable tool for planning treatment in this population as an alternative to completion axillary lymph node dissection.
Breast cancer is the leading cause of cancer mortality in women worldwide, according to the World Health Organization . Most patients are currently diagnosed with localized non-metastatic breast cancer (Stages 0–1) on mammography . The most important determinant of prognosis for breast cancer patients are tumor size and the status of the axillary lymph nodes . The presence of regional metastases in the axillary basin reduces a patients’ 5-year survival by approximately 28% to 40% . Staging of the axilla was formerly performed at surgery with a level I and II axillary lymph node dissection. Axillary lymph node dissection has significant side effects of lymphedema and arm swelling . Since the early 1990s, sentinel lymph node mapping and subsequent biopsy has shown much promise in the axillary staging and surgical management of breast cancer . The sentinel node biopsy is based on the sentinel node hypothesis proposed by Cabanas . The aim of the technique is to demonstrate which patients have axillary metastasis and resulting direct subsequent lymph node dissection. Many studies have demonstrated the accuracy of sentinel lymph node mapping in the staging of early breast cancer . Reported identification rates and false-negative rates (FNR) in patients who have not received chemotherapy range from 84% to 100% and 0% to 13%, respectively . Sentinel lymph node mapping is rapidly replacing axillary lymph node dissection in the primary staging of breast cancer .
Preoperative (or neoadjuvant) chemotherapy has become the standard of care in patients with locally advanced breast cancer (Stage IIIB) and is being used increasingly in patients with localized non-metastatic disease (Stages 0–1) . Although it has not improved the survival rate compared to adjuvant chemotherapy, neoadjuvant chemotherapy can decrease the magnitude of the operative procedure required, converting many patients from mastectomy to breast conservation surgery . The use of sentinel lymph node mapping in patients after preoperative chemotherapy has been proposed, but its role is less certain. Studies in the literature report identification rates of 76.3% to 100% and accuracies of 79% to 98% . The question of whether sentinel node biopsy is feasible and accurate after neoadjuvant chemotherapy is one of great importance because neoadjuvant chemotherapy has been shown to downstage axillary lymph nodes in a significant proportion of patients .
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Methods
Study Search Strategy
Get Radiology Tree app to read full this article<
Study Selection Criteria
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Data Extraction
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Assessment of Methodological Quality and Publication Bias
Get Radiology Tree app to read full this article<
Summary of Diagnostic Test Performance
Get Radiology Tree app to read full this article<
Sensitivity Analyses of Study-level Characteristics and Summary Performance
Get Radiology Tree app to read full this article<
Exploratory Analyses
Get Radiology Tree app to read full this article<
Results
Study Identification
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Study Characteristics
Get Radiology Tree app to read full this article<
Table 1
Individual Study Characteristics and Performance
Author Year Journal Origin Mean Age Number of Patients NPV SIR FNR Aihara et al 2004Journal of Surgical Oncology Japan 62 endo, 47 chemo 16 endo, 20 chemo 0.929 0.85 0.08 Balch et al 2003Annals of Surgical Oncology USA 51 32 0.923 0.97 0.05 Brady et al 2002The Breast Journal USA 44 14 1 0.93 0.00 Cohen et al 2000The American Journal of Surgical Pathology USA 45 ∗ 38 0.813 0.82 0.20 Fernandez et al 2000Nuclear Medicine Communications Spain 55 36 0.778 0.94 0.25 Haid et al 2001Cancer Austria 53 33 1 0.88 0.00 Jones et al 2005American Journal of Surgery USA N/A 36 0.846 0.81 0.16 Khan et al 2005Annals of Surgical Oncology USA 40 ∗ 33 0.857 0.96 0.05 Kinoshita et al 2007Breast Cancer Japan 50.2 104 0.938 0.94 0.19 Lang et al 2004Journal of the American College of Surgery USA 51 ∗ 53 0.967 0.94 0.04 Lee et al 2007Breast Cancer Results Treatment Korea 46.1 219 0.868 0.78 0.16 Mahmounas et al 2005Journal of Clinical Oncology USA N/A 428 0.931 0.80 0.11 Miller et al 2002Annals of Surgical Oncology USA N/A 35 1 0.86 0.00 Nason et al 2000Cancer USA N/A 82 0.571 0.80 0.33 Patel et al 2004The American Surgeon USA N/A 42 1 0.95 0.00 Piato et al 2002European Journal of Surgical Oncology Brazil N/A 42 0.885 0.98 0.17 Reitsamer et al 2003Journal of Surgical Oncology Austria 31–74 41 0.917 0.63 0.07 Schwartz et al 2003The Breast Journal USA 50 21 0.909 1.00 0.09 Shimazu et al 2004Cancer Japan 51.3 47 0.733 0.94 0.12 Stearns et al 2002Annals of Surgical Oncology USA 46 34 0.875 0.85 0.06 Tafra et al 2001American Journal of Surgery USA N/A 29 1 0.93 0.00 Tanaka et al 2006Oncology Reports Japan N/A 70 0.958 0.90 0.03 Tausch et al 2006Annals of Surgical Oncology Austria 50 ∗ 167 0.931 0.84 0.06 Yu et al 2006Annals of Surgical Oncology Taiwan 42.6 127 0.912 0.91 0.08
Chemo: chemotherapy; Endo: endocrine therapy; FNR: false-negative rate; NPV: negative predictive value; SIR: identification rate.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Assessment of Quality
Get Radiology Tree app to read full this article<
Table 2
Quality Characteristics by Study
Author Year Prospective Study Design Size >30 Verification Test Index Test Reference Test Subjects Report Consecutive Broad Blind Multiple Institutions Aihara et al 2004 Yes Yes Yes Yes Yes Yes No Yes No No Not described Balch et al 2003 Yes Yes Yes Yes Yes Yes No Yes Yes No Single institution, multiple surgeons Brady et al 2002 No No Yes Yes Yes No No Yes Yes No Single institution, single surgeon Cohen et al 2000 Yes Yes Yes Yes Yes Yes No Yes Yes No Single institution Fernandez et al 2000 Yes Yes Yes Yes Yes Yes No Yes Yes No Single institution Haid et al 2001 Yes Yes Yes Yes Yes Yes No No Yes No Single institution Jones et al 2005 No Yes Yes No No No Yes Yes Yes No Multicenter trial Khan et al 2005 No Yes Yes Yes Yes Yes Yes Yes Yes No Single institution Kinoshita et al 2007 Yes Yes Yes Yes No Yes Yes Yes Yes No Single institution Lang et al 2004 Yes Yes Yes Yes Yes Yes No Yes Yes No Single institution Lee et al 2007 Yes Yes Yes Yes Yes Yes Yes Yes Yes No Single institution, multiple surgeons Mahmounas et al 2005 Yes Yes Yes Yes Yes Yes No Yes Yes No Multicenter trial Miller et al 2002 Yes Yes Yes Yes Yes No No Yes Yes No Single institution Nason et al 2000 Yes Yes Yes Yes Yes Yes No Yes Yes No Single institution, multiple surgeons Patel et al 2004 No Yes Yes Yes Yes Yes No No Yes No Single institution, multiple surgeons Piato et al 2002 Yes Yes Yes Yes Yes Yes No Yes Yes No Single institution Reitsamer et al 2003 Yes Yes Yes Yes Yes Yes No Yes Yes No Not described Schwartz et al 2003 Yes No Yes Yes Yes Yes No Yes Yes No Single institution, single surgeon Shimazu et al 2004 Yes Yes Yes Yes Yes Yes No Yes Yes No Single institution Stearns et al 2002 Yes No Yes Yes Yes Yes Yes Yes Yes No Single institution, multiple surgeons Tafra et al 2001 Yes No Yes Yes Yes Yes No Yes Yes No Multicenter trial Tanaka et al 2006 Yes Yes Yes Yes Yes Yes Yes Yes Yes No Single institution Tausch et al 2006 No Yes Yes Yes Yes No Yes Yes Yes No Multicenter trial Yu et al 2006 Yes Yes Yes Yes Yes Yes Yes Yes Yes No Single institution
Get Radiology Tree app to read full this article<
Summary of Diagnostic Test Performance
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Sensitivity Analyses of Study-level Characteristics and Summary Performance
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Table 3
Effect of Study-level Covariates on Successful Identification Rates and False-negatives Rates
Successful Identification Rate False-Negative Rate Covariate Covariate = Yes Covariate = No Covariate = Yes Covariate = No Dual mapping technique 0.898 0.877 0.095 0.066 Immunohistochemistry 0.857 0.929 0.087 0.071 Same-day mapping and axillary node dissection ∗ 0.900 0.893 0.058 0.115 Use of gamma probe 0.884 0.889 0.088 0.066 Peritumoral injection 0.889 0.884 0.067 0.116
The estimates of each parameter in the presence or absence of each covariate were evaluated using univariate metaregression.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Assessment of Publication Bias
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Exploratory Analyses
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Discussion
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Conclusion
Get Radiology Tree app to read full this article<
Appendix 1
Individual quality criteria in assessment of studies
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
References
1. World Health Organization. Annex Table 2: Deaths by cause, sex and mortality stratum in WHO regions, estimates for 2002. Available online at: http://www.who.int/whr/2004/annex/topic/en/annex_2_en.pdf . Accessed on January 12, 2009. 2004.
2. Edwards B.K., Brown M.L., Wingo P.A., et. al.: Annual report to the nation on the status of cancer, 1975–2002, featuring population-based trends in cancer treatment. J Natl Cancer Inst 2005; 97: pp. 1407-1427.
3. Weir H.K., Thun M.J., Hankey B.F., et. al.: Annual report to the nation on the status of cancer, 1975–2000, featuring the uses of surveillance data for cancer prevention and control. J Natl Cancer Inst 2003; 95: pp. 1276-1299.
4. Carter C.L., Allen C., Henson D.E.: Relation of tumor size, lymph node status, and survival in 24,740 breast cancer cases. Cancer 1989; 63: pp. 181-187.
5. Nemoto T., Vana J., Bedwani R.N., et. al.: Management and survival of female breast cancer: results of a national survey by the American College of Surgeons. Cancer 1980; 45: pp. 2917-2924.
6. Warmuth M.A., Bowen G., Prosnitz L.R., et. al.: Complications of axillary lymph node dissection for carcinoma of the breast: a report based on a patient survey. Cancer 1998; 83: pp. 1362-1368.
7. Shaw J.H., Rumball E.M.: Complications and local recurrence following lymphadenectomy. Br J Surg 1990; 77: pp. 760-764.
8. Giuliano A.E., Kirgan D.M., Guenther J.M., et. al.: Lymphatic mapping and sentinel lymphadenectomy for breast cancer. Ann Surg 1994; 220: pp. 391-398. discussion 398–401
9. Canavese G., Gipponi M., Catturich A., et. al.: Sentinel lymph node mapping in early-stage breast cancer: technical issues and results with vital blue dye mapping and radioguided surgery. J Surg Oncol 2000; 74: pp. 61-68.
10. Cabanas R.M.: The concept of the sentinel lymph node. Recent Results Cancer Res 2000; 157: pp. 109-120.
11. Gurleyik G., Aker F., Sekmen U., et. al.: Accuracy of sentinel lymph node biopsy for the assessment of axillary status in patients with early (T1) breast carcinoma. J Coll Physicians Surg Pak 2005; 15: pp. 697-700.
12. Miltenburg D.M., Miller C., Karamlou T.B., et. al.: Meta-analysis of sentinel lymph node biopsy in breast cancer. J Surg Res 1999; 84: pp. 138-142.
13. Fraile M., Rull M., Julian F.J., et. al.: Sentinel node biopsy as a practical alternative to axillary lymph node dissection in breast cancer patients: an approach to its validity. Ann Oncol 2000; 11: pp. 701-705.
14. Trocha S.D., Giuliano A.E.: Sentinel node in the era of neoadjuvant therapy and locally advanced breast cancer. Surg Oncol 2003; 12: pp. 271-276.
15. Lyman G.H., Giuliano A.E., Somerfield M.R., et. al.: American Society of Clinical Oncology guideline recommendations for sentinel lymph node biopsy in early-stage breast cancer. J Clin Oncol 2005; 23: pp. 7703-7720.
16. Estevez L.G., Gradishar W.J.: Evidence-based use of neoadjuvant taxane in operable and inoperable breast cancer. Clin Cancer Res 2004; 10: pp. 3249-3261.
17. Xing Y., Cormier J.N., Kuerer H.M., et. al.: Sentinel lymph node biopsy following neoadjuvant chemotherapy: review of the literature and recommendations for use in patient management. Asian J Surg 2004; 27: pp. 262-267.
18. Aihara T., Munakata S., Morino H., et. al.: Feasibility of sentinel node biopsy for breast cancer after neoadjuvant endocrine therapy: a pilot study. J Surg Oncol 2004; 85: pp. 77-81.
19. Balch G.C., Mithani S.K., Richards K.R., et. al.: Lymphatic mapping and sentinel lymphadenectomy after preoperative therapy for stage II and III breast cancer. Ann Surg Oncol 2003; 10: pp. 616-621.
20. Brady E.W.: Sentinel lymph node mapping following neoadjuvant chemotherapy for breast cancer. Breast J 2002; 8: pp. 97-100.
21. Cohen L.F., Breslin T.M., Kuerer H.M., et. al.: Identification and evaluation of axillary sentinel lymph nodes in patients with breast carcinoma treated with neoadjuvant chemotherapy. Am J Surg Pathol 2000; 24: pp. 1266-1272.
22. Fernandez A., Cortes M., Benito E., et. al.: Gamma probe sentinel node localization and biopsy in breast cancer patients treated with a neoadjuvant chemotherapy scheme. Nucl Med Commun 2001; 22: pp. 361-366.
23. Haid A., Tausch C., Lang A., et. al.: Is sentinel lymph node biopsy reliable and indicated after preoperative chemotherapy in patients with breast carcinoma?. Cancer 2001; 92: pp. 1080-1084.
24. Jones J.L., Zabicki K., Christian R.L., et. al.: A comparison of sentinel node biopsy before and after neoadjuvant chemotherapy: timing is important. Am J Surg 2005; 190: pp. 517-520.
25. Khan A., Sabel M.S., Nees A., et. al.: Comprehensive axillary evaluation in neoadjuvant chemotherapy patients with ultrasonography and sentinel lymph node biopsy. Ann Surg Oncol 2005; 12: pp. 697-704.
26. Kinoshita T.: Sentinel lymph node biopsy is feasible for breast cancer patients after neoadjuvant chemotherapy. Breast Cancer 2007; 14: pp. 10-15.
27. Lang J.E., Esserman L.J., Ewing C.A., et. al.: Accuracy of selective sentinel lymphadenectomy after neoadjuvant chemotherapy: effect of clinical node status at presentation. J Am Coll Surg 2004; 199: pp. 856-862.
28. Lee S., Kim E.Y., Kang S.H., et. al.: Sentinel node identification rate, but not accuracy, is significantly decreased after pre-operative chemotherapy in axillary node-positive breast cancer patients. Breast Cancer Res Treat 2007; 102: pp. 283-288.
29. Mamounas E.P., Brown A., Anderson S., et. al.: Sentinel node biopsy after neoadjuvant chemotherapy in breast cancer: results from National Surgical Adjuvant Breast and Bowel Project Protocol B-27. J Clin Oncol 2005; 23: pp. 2694-2702.
30. Miller A.R., Thomason V.E., Yeh I.T., et. al.: Analysis of sentinel lymph node mapping with immediate pathologic review in patients receiving preoperative chemotherapy for breast carcinoma. Ann Surg Oncol 2002; 9: pp. 243-247.
31. Nason K.S., Anderson B.O., Byrd D.R., et. al.: Increased false negative sentinel node biopsy rates after preoperative chemotherapy for invasive breast carcinoma. Cancer 2000; 89: pp. 2187-2194.
32. Patel N.A., Piper G., Patel J.A., et. al.: Accurate axillary nodal staging can be achieved after neoadjuvant therapy for locally advanced breast cancer. Am Surg 2004; 70: pp. 696-699. discussion 699–700
33. Piato J.R., Barros A.C., Pincerato K.M., et. al.: Sentinel lymph node biopsy in breast cancer after neoadjuvant chemotherapy. A pilot study. Eur J Surg Oncol 2003; 29: pp. 118-120.
34. Reitsamer R., Peintinger F., Rettenbacher L., et. al.: Sentinel lymph node biopsy in breast cancer patients after neoadjuvant chemotherapy. J Surg Oncol 2003; 84: pp. 63-67.
35. Schwartz G.F., Meltzer A.J.: Accuracy of axillary sentinel lymph node biopsy following neoadjuvant (induction) chemotherapy for carcinoma of the breast. Breast J 2003; 9: pp. 374-379.
36. Shimazu K., Tamaki Y., Taguchi T., et. al.: Sentinel lymph node biopsy using periareolar injection of radiocolloid for patients with neoadjuvant chemotherapy-treated breast carcinoma. Cancer 2004; 100: pp. 2555-2561.
37. Stearns V., Ewing C.A., Slack R., et. al.: Sentinel lymphadenectomy after neoadjuvant chemotherapy for breast cancer may reliably represent the axilla except for inflammatory breast cancer. Ann Surg Oncol 2002; 9: pp. 235-242.
38. Tafra L., Verbanac K.M., Lannin D.R.: Preoperative chemotherapy and sentinel lymphadenectomy for breast cancer. Am J Surg 2001; 182: pp. 312-315.
39. Tanaka Y., Maeda H., Ogawa Y., et. al.: Sentinel node biopsy in breast cancer patients treated with neoadjuvant chemotherapy. Oncol Rep 2006; 15: pp. 927-931.
40. Tausch C., Konstantiniuk P., Kugler F., et. al.: Sentinel lymph node biopsy after preoperative chemotherapy for breast cancer: findings from the Austrian Sentinel Node Study Group. Ann Surg Oncol 2006;
41. Yu J.C., Hsu G.C., Hsieh C.B., et. al.: Role of sentinel lymphadenectomy combined with intraoperative ultrasound in the assessment of locally advanced breast cancer after neoadjuvant chemotherapy. Ann Surg Oncol 2007; 14: pp. 174-180.
42. Mamounas E.P.: Sentinel lymph node biopsy after neoadjuvant systemic therapy. Surg Clin North Am 2003; 83: pp. 931-942.
43. Xing Y., Foy M., Cox D.D., et. al.: Meta-analysis of sentinel lymph node biopsy after preoperative chemotherapy in patients with breast cancer. Br J Surg 2006; 93: pp. 539-546.
44. Moher D., Cook D.J., Eastwood S., et. al.: Improving the quality of reports of meta-analyses of randomised controlled trials: the QUOROM statement. Quality of Reporting of Meta-analyses. Lancet 1999; 354: pp. 1896-1900.
45. Honest H., Khan K.S.: Reporting of measures of accuracy in systematic reviews of diagnostic literature. BMC Health Serv Res 2002; 2: pp. 4.
46. Jackson D C.J., Sutton A.J.: Modelling reporting bias: the operative mortality rate for ruptured abdominal aortic aneurysm repair. J Royal Statist Soc 2005; 168: pp. 737-752.
47. van Houwelingen H.C., Arends L.R., Stijnen T.: Advanced methods in meta-analysis: multivariate approach and meta-regression. Stat Med 2002; 21: pp. 589-624.
48. Higgins J.P., Thompson S.G., Deeks J.J., et. al.: Measuring inconsistency in meta-analyses. Bmj 2003; 327: pp. 557-560.
49. Khoshdel A., Attia J., Carney S.L.: Basic concepts in meta-analysis: a primer for clinicians. Int J Clin Pract 2006; 60: pp. 1287-1294.
50. Thompson S.G., Higgins J.P.: How should meta-regression analyses be undertaken and interpreted?. Stat Med 2002; 21: pp. 1559-1573.
51. Jemal A., Ward E., Thun M.J.: Recent trends in breast cancer incidence rates by age and tumor characteristics among U.S. women. Breast Cancer Res 2007; 9: R28
52. Jemal A., Siegel R., Ward E., et. al.: Cancer statistics, 2007. CA Cancer J Clin 2007; 57: pp. 43-66.
53. NCCN Clinical Practice Guidlines in Oncology. Breast cancer. In: http://www.nccn.org/professionals/physician_gls/PDF/breast.pdf : National Comprehensive Cancer Network, 2007.