The purpose of this discussion is to elucidate several powerful tools of the expert to support and focus diagnostic reasoning of learners and novice health care professionals. Use of these methods serves to focus the thinking of the learner to direct them to pursue useful pathways of investigation and emphasize the likelihood of one illness over others.
Elements used in diagnostic reasoning
As learners progress from students to physicians, they develop and mature skills in clinical decision-making and problem-solving. A number of steps are involved—most importantly experience, exposure to many different clinical situations, and the benefits gained from the direction of an experienced teacher.
The initial step is learning the importance of semantic qualifiers , which are sets of terms that describe the presentation of a clinical problem. Semantic qualifiers assist in problem representation. These qualifiers are abstract concepts, often opposites, called forth in medicine to assist in applying experience to help reach and define a medical decision. The qualifiers may supply critical differentiating evidence for the assignment of an illness into existing medical categories. Examples of semantic qualifiers are: acute versus chronic, previously well versus chronically ill, productive cough versus dry cough, sharp versus dull pain, progressive versus unchanged (the semantic qualifiers are in italics) .
Semantic qualifiers are applied to the patient description and facilitate thinking about the problem, summarizing the problem and its solution, and defining the clinical problem. Using semantic qualifiers, a case may be seen and interpreted differently by a novice in contrast to an experienced master. Consider the radiology example of a 35-year-old female patient who presents for an ultrasound examination of a lower abdominal wall mass. Initial considerations are quite broad and include diverse processes such as hernia, abscess, lipoma, hematoma, endometrioma, metastases, and desmoid. Helpful semantic qualifiers include acute versus chronic , and painful versus nonpainful . The experienced physician, upon learning that this mass is chronic and painful , would then use additional semantic qualifiers regarding the painful nature, such as continuous versus intermittent , to determine that this intermittently (cyclic) painful mass likely represents an endometrioma.
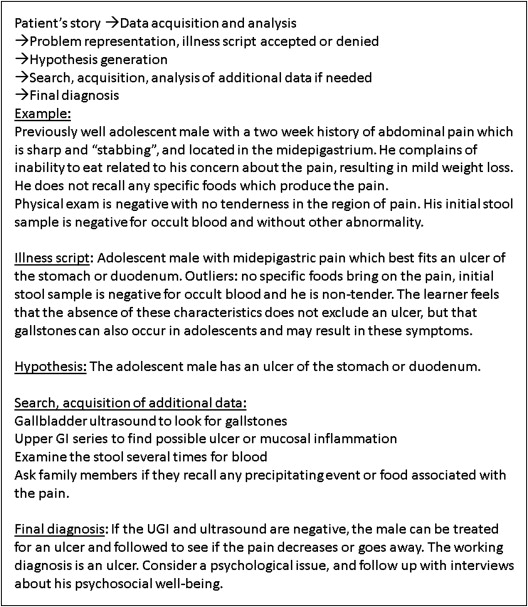
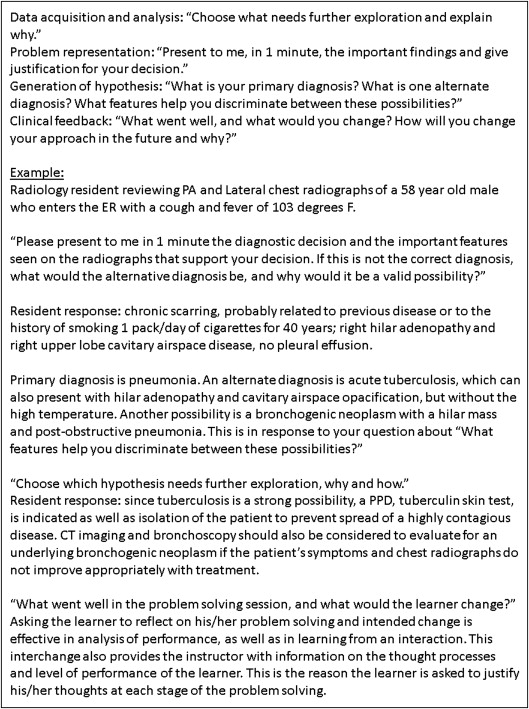
With experience, a physician also develops illness scripts that are built on the prototypical presentations of an illness. These scripts solve problems instantly in that the learner can specify the illness by its characteristics, identify typical differences or deviations, and recognize unexpected differences in a presentation from the expected prototype. Such differentiators serve as “red flags” to warn the physician not to make assumptions or leap to a conclusion about an illness based on some typical appearances. The expert owns many more illness scripts than does the novice. Although the scripts are designed to highlight differences, they may lead to early decisions that ignore minor appearances and result in errors of differentiation that are important in diagnosis or management as well as pathways of diagnosis. It has been shown that a clinical history with discordant physical findings substantially decreases diagnostic accuracy . Thus, although illness scripts serve as useful shortcuts, only the master or expert appropriately identifies outliers that require attention as differentiated from outliers that do not need specific attention.
Illness scripts are used in the hands of experienced experts who recognize an illness by its prototypical features and make their decision based on these facts. They are able to categorize an illness according to their own established categories of disease. This efficient way of defining a feature-based category of illness frees up reasoning resources to determine what, and if, additional features should be considered to change or challenge a diagnostic decision, pursue further testing to entertain a different diagnosis, or define the feature as belonging to the category in question. At the same time, missing but expected features are considered as part of the diagnostic decision. Using illness scripts introduces two types of error: making a decision too early and too decisively so that the diagnostician excludes other diagnostic possibilities, and becoming too attached to a diagnostic decision to foster questioning and investigation based on further study and testing. These types of errors can also be described as anchoring bias and premature closure. With anchoring bias, the physician becomes attached to a specific diagnosis too early and then interprets additional patient information in terms of that diagnosis. Once the physician has latched on to this initial diagnosis, an alternate diagnosis is not entertained. This results in premature closure, the “failure to consider other possibilities once an initial diagnosis has been reached” . Identifying what is missing in order to make a diagnosis requires that the diagnostician determine features critical to a diagnosis and those that are not essential in the face of “classic” features .
Two Radiology Examples
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Strategies used in teaching diagnostic reasoning skills
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Revisiting the Two Radiology Examples
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Conclusion
Get Radiology Tree app to read full this article<
Acknowledgment
Get Radiology Tree app to read full this article<
References
1. Bordage G., Lemieux M.: Semantic structures and diagnostic thinking of experts and novices. Acad Med 1991; 66: pp. S70-S72.
2. Bordage G.: Why did I miss the diagnosis? Some cognitive explanations and educational implications. Acad Med 1999; 74: pp. S138-S143.
3. Bordage G.: Prototypes and semantic qualifiers: from past to present. Med Educ 2007; 41: pp. 1117-1121.
4. Cohn J.: The robot will see you now. Atlantic 2013; pp. 59-65.
5. Charlin B., Tardif J., Boshuizen H.P.: Scripts and medical diagnostic knowledge; theory and applications for clinical reasoning, instruction and research. Acad Med 2000; 75: pp. 182-190.
6. Custers E.J., Regehr G., Norman G.R.: Mental representations of medical diagnostic knowledge: a review. Acad Med 1996; 71: pp. S55-S61.
7. Schmidt H.G., Norman G.R., Boshuizen H.P.: A cognitive perspective on medical expertise: theory and implications. Acad Med 1990; 65: pp. 611-621.
8. Sibbald M., Cavalcanti R.B.: The biasing effect of clinical history on physical examination diagnostic accuracy. Med Educ 2011; 45: pp. 827-834.
9. Graber M.L., Franklin N., Gordon R.: Diagnostic error in internal medicine. Arch Intern Med 2005; 165: pp. 1493-1499.
10. Hamstra S., Philibert I.: Simulation in graduate medical education: understanding uses and maximizing benefits. J Grad Med Educ 2012; 4: pp. 539-542.