Rationale and Objective
The objective of this study was to evaluate breast lesion outcomes in patients after canceled MRI-guided breast biopsy due to lesion nonvisualization.
Materials and Methods
Electronic medical records (January 2007–December 2014) were searched for patients with canceled magnetic resonance imaging (MRI)-guided breast biopsies due to lesion nonvisualization. A total of 1403 MRI-detected lesions were scheduled for MRI-guided biopsy and 89 were canceled because of nonvisualization. Imaging studies and medical records were reviewed for patient demographics, lesion characteristics, and subsequent malignancy. Patients without adequate MRI follow-up imaging were excluded. Statistical analysis was employed to determine if patient demographics or lesion characteristics were predictive of lesion resolution or lesion biopsy after subsequent follow-up.
Results
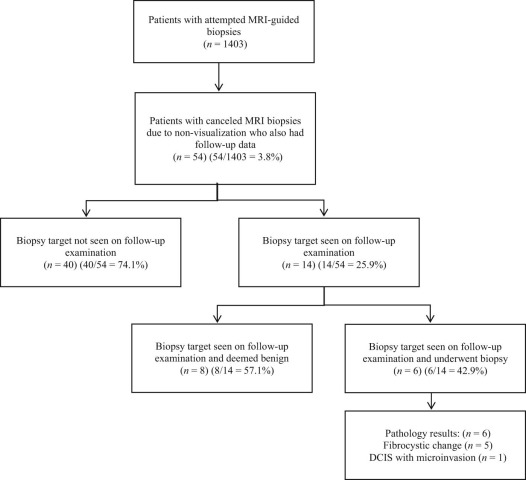
Eighty-nine (6.3% [89/1403]; 95% confidence interval, 5.2%–7.7%) biopsies in 89 women were canceled because of nonvisualization. Follow-up MRIs greater than 5.5 months were available for 60.7% (54/89) of women. In 74.1% (40/54) of these patients, the lesions completely resolved on follow-up. In 25.9% (14/54) of the patients, the lesion persisted on follow-up; 42.9% (6/14) of these patients underwent biopsy. One case (1.9% [1/54]) yielded ductal carcinoma in situ with microinvasion at the 6-month follow-up. No patient demographics or lesion features were associated with lesion resolution or lesion biopsy.
Conclusions
The majority of canceled MRI-guided biopsy lesions resolved on later follow-up; however, because of the small possibility of a missed malignancy, follow-up MRI imaging at 6 months is recommended.
Introduction
Numerous studies have demonstrated the diagnostic utility of magnetic resonance imaging (MRI) breast cancer detection compared to mammography and ultrasound, particularly in high-risk patient populations . Additionally, the advent of MRI-guided vacuum-assisted biopsy has provided a relatively quick and safe method of sampling tissue, sparing patients the time and invasiveness of a surgical biopsy . In some instances, however, MRI-guided biopsies may be canceled; reported rates of biopsy cancellation have ranged from 8% to 13%, most often because of nonvisualization of the initial biopsy target on the scheduled day of biopsy . Lesions may not be visualized because the lesion has resolved at the time of biopsy and may have only been due to background parenchymal enhancement (BPE), now no longer seen. In other cases, however, lesions may be canceled for technical reasons such as poor patient positioning or compression, which may impede contrast delivery to the breast. These canceled biopsies can thus be a source of confusion and frustration for both clinicians and patients. Only a few studies have specifically investigated the clinical course of these nonvisualized lesions; the reported frequency of subsequent malignancy has ranged from 0% to 10% .
A better understanding of the longer term outcomes after nonvisualization of an MRI-guided biopsy target is warranted to help guide decisions regarding appropriate follow-up and treatment. The purpose of the present study, therefore, was to evaluate outcomes—including subsequent development of ipsilateral quadrant malignancy—in patients who had a canceled MRI-guided breast biopsy due to nonvisualization of the lesion on the day of biopsy. A secondary purpose was to determine if any patient demographics or lesion characteristics were predictive of lesion resolution or lesion biopsy after subsequent follow-up.
Materials and Methods
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
MRI Technique
Get Radiology Tree app to read full this article<
MRI-Biopsy Imaging Technique
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Patient Characteristics
Get Radiology Tree app to read full this article<
Imaging Findings
Get Radiology Tree app to read full this article<
Follow-up
Get Radiology Tree app to read full this article<
Data Collection and Statistical Analysis
Get Radiology Tree app to read full this article<
Results
Get Radiology Tree app to read full this article<
Patient Characteristics
Get Radiology Tree app to read full this article<
TABLE 1
Patient Demographics and Lesion Characteristics in the Initial Diagnostic Study
Patient/Lesion Characteristics ( n = 54)n (%) Patient age (y) 45.5 (range, 23.0–67.0) Menopausal status Premenopausal 38 (70.3) Postmenopausal 16 (29.6) Family history of breast cancer Yes 26 (48.1) No 28 (51.9) Personal history of breast cancer Yes 27 (50.0) Prior 9 (33.3) Current 18 (66.7) No 27 (50.0) Indication for MRI Screening 34 (63.0) Diagnostic 20 (37.0) Background enhancement Minimal 12 (22.2) Mild 16 (29.6) Moderate 22 (40.7) Marked 4 (7.4) Lesion type on initial MRI Focus 1 (1.9) Nonmass enhancement 38 (70.4) Mass 15 (27.8) Lesion size (cm) on initial MRI Mean 2.2 Median 1.0 Range 0.3–8.0 Lesion kinetics on initial MRI Persistent 40 (74.1) Plateau 12 (22.2) Washout 2 (3.7) BI-RADS (lesion) 3 1 (1.9) 4a 33 (61.1) 4b 20 (37.0) 4c 0 (0) 5 0 (0)
BI-RADS, Breast Imaging Reporting and Data Systems; MRI, magnetic resonance imaging.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Imaging Findings
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
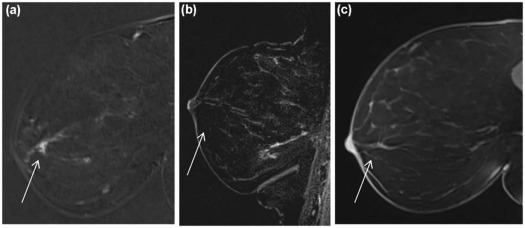
Follow-up—Benign Lesions
Get Radiology Tree app to read full this article<
TABLE 2
Characteristics of Lesions Undergoing Subsequent Biopsy
Case Size on Initial MRI Lesion Morphology on Initial MRI Lesion Kinetics on Initial MRI BI-RADs on Initial MRI Time to Subsequent Bx (mo) Lesion Size on Fup MRI Lesion Morphologyon Fup MRI Lesion Kinetics on Fup MRI Lesion Features on Fup MRI BI-RADs on Fup MRI MRI-guided Bx Pathology Result 1 1.0 Mass 3 4b 5.6 1.0 Mass 3 Lesion revisualized, new calcs on mammo 4b DCIS with microinvasion 2 0.7 Mass 1 4a 38.9 0.8 Mass 1 Increased in size 4a FCC 3 \* 2.5 NME 1 3 24.2 2.5 NME 1 Lesion revisualized, stable 3 FCC 4 1.5 NME 2 4a 21.2 3.5 NME 2 Increased in size 4a FCC 5 1.3 NME 1 4a 26.9 1.3 NME 1 Lesion revisualized, stable 4a FCC 6 2.5 NME 1 4a 12.1 2.5 NME 1 Lesion revisualized, stable 4a FCC
BI-RADS, Breast Imaging Reporting and Data System; Bx, biopsy; calcs, calcifications; DCIS, ductal carcinoma in situ; FCC, fibrocystic change; Fup, follow-up; mammo, mammogram; MRI, magnetic resonance imaging; NME, nonmass enhancement.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
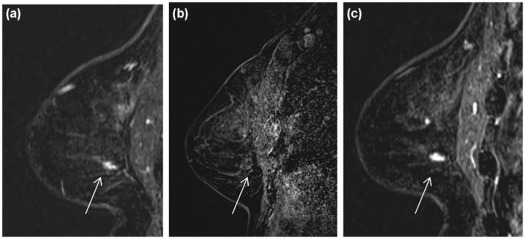
Follow-up—Malignancy
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Discussion
Get Radiology Tree app to read full this article<
TABLE 3
Frequency of Malignancy After Canceled MRI-guided Biopsy
Study/Year Number of Lesions Recommended for MRI-guided Biopsy Number (%) of Lesions Canceled Because of Nonvisualization Number of Lesions with Fup Imaging Number of Lesions with Pathology Fup Reported Median Fup Times Number (%) of Malignancies in Ipsilateral Quadrant Malignant Pathology Perlet et al. (2002) 413 46 (10) 46 0 1–4 d 0 (0) Hefler et al. (2003) 291 37 (13) 29 0 4–24 h 3 (10) One IDC and one ILC on short-term follow-up without compression; one IDC after biopsy on the day of the scheduled biopsy, despite the lack of contrast enhancement Liberman et al. (2005) 112 14 (13) 13 0 5 mo 0 (0) Viehweg et al. (2006) 83 10 (10) 10 0 6 mo 0 (0) Han et al. (2008) 172 22 (13) 18 0 Not reported 0 (0) Brennan et al. (2011) 911 74 (8) 58 3 12 mo 1 (2) One DCIS after mastectomy Johnson et al. (2013) 117 15 (13) 11 3 19.5 mo 0 (0) Niell et al. (2014) 445 56 (13) 41 8 154 d 5 (10) One IDC and one DCIS after mastectomy, one IDC after excisional biopsy, and one IDC and one DCIS on follow-up at 6 wk and 6 mo This study (2017) 1403 89 (6) 54 0 21.9 mo 1 (2) One DCIS on follow-up at 6 mo
DCIS, ductal carcinoma in situ; Fup, follow-up; IDC, invasive ductal carcinoma; ILC, invasive lobular carcinoma; MRI, magnetic resonance imaging.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
References
1. Morris E.A., Liberman L., Ballon D.J., et. al.: MRI of occult breast carcinoma in a high-risk population. AJR Am J Roentgenol 2003; 181: pp. 619-626.
2. Berg W.A., Gutierrez L., NessAiver M.S., et. al.: Diagnostic accuracy of mammography, clinical examination, US, and MR imaging in preoperative assessment of breast cancer. Radiology 2004; 233: pp. 830-849.
3. Lord S.J., Lei W., Craft P., et. al.: A systematic review of the effectiveness of magnetic resonance imaging (MRI) as an addition to mammography and ultrasound in screening young women at high risk of breast cancer. Eur J Cancer 2007; 43: pp. 1905-1917.
4. Hagen A.I., Kvistad K.A., Maehle L., et. al.: Sensitivity of MRI versus conventional screening in the diagnosis of BRCA-associated breast cancer in a national prospective series. Breast 2007; 16: pp. 367-374.
5. Kriege M., Brekelmans C.T., Boetes C., et. al.: Efficacy of MRI and mammography for breast-cancer screening in women with a familial or genetic predisposition. N Engl J Med 2004; 351: pp. 427-437.
6. Kuhl C.K., Schrading S., Leutner C.C., et. al.: Mammography, breast ultrasound, and magnetic resonance imaging for surveillance of women at high familial risk for breast cancer. J Clin Oncol 2005; 23: pp. 8469-8476.
7. Leach M.O., Boggis C.R., Dixon A.K., et. al.: Screening with magnetic resonance imaging and mammography of a UK population at high familial risk of breast cancer: a prospective multicentre cohort study (MARIBS). Lancet 2005; 365: pp. 1769-1778.
8. Lehman C.D., Blume J.D., Weatherall P., et. al.: Screening women at high risk for breast cancer with mammography and magnetic resonance imaging. Cancer 2005; 103: pp. 1898-1905.
9. Lehman C.D., Isaacs C., Schnall M.D., et. al.: Cancer yield of mammography, MR, and US in high-risk women: prospective multi-institution breast cancer screening study. Radiology 2007; 244: pp. 381-388.
10. Warner E., Messersmith H., Causer P., et. al.: Systematic review: using magnetic resonance imaging to screen women at high risk for breast cancer. Ann Intern Med 2008; 148: pp. 671-679.
11. American College of Radiology : ACR practice parameter for the performance of magnetic resonance imaging-guided breast interventional procedures. Available at: https://www.acr.org/-/media/ACR/Files/Practice-Parameters/MR-Guided-Breast.pdf
12. Kuhl C.K., Morakkabati N., Leutner C.C., et. al.: MR imaging- guided large-core (14-gauge) needle biopsy of small lesions visible at breast MR imaging alone. Radiology 2001; 220: pp. 31-39.
13. Chen X., Lehman C.D., Dee K.E.: MRI-guided breast biopsy: clinical experience with 14-gauge stainless steel core biopsy needle. AJR Am J Roentgenol 2004; 182: pp. 1075-1080.
14. Hauth E.A., Jaeger H.J., Lubnau J., et. al.: MR-guided vacuum-assisted breast biopsy with a handheld biopsy system: clinical experience and results in postinterventional MR mammography after 24 h. Eur Radiol 2008; 18: pp. 168-176.
15. Liberman L., Bracero N., Morris E., et. al.: MRI-guided 9-gauge vacuum-assisted breast biopsy: initial clinical experience. AJR Am J Roentgenol 2005; 185: pp. 183-193.
16. Niell B.L., Lee J.M., Johansen C., et. al.: Patient outcomes in canceled MRI-guided breast biopsies. AJR Am J Roentgenol 2014; 202: pp. 223-228.
17. Hefler L., Casselman J., Amaya B., et. al.: Follow-up of breast lesions detected by MRI not biopsied due to absent enhancement of contrast medium. Eur Radiol 2003; 13: pp. 344-346.
18. Brennan S.B., Sung J.S., Dershaw D.D., et. al.: Cancellation of MR imaging-guided breast biopsy due to lesion nonvisualization: frequency and follow-up. Radiology 2011; 261: pp. 92-99.
19. Perlet C., Heinig A., Prat X., et. al.: Multicenter study for the evaluation of a dedicated biopsy device for MR-guided vacuum biopsy of the breast. Eur Radiol 2002; 12: pp. 1463-1470.
20. Viehweg P., Bernerth T., Kiechle M., et. al.: MR-guided intervention in women with a family history of breast cancer. Eur J Radiol 2006; 57: pp. 81-89.
21. Johnson K.S., Baker J.A., Lee S.S., et. al.: Cancelation of MRI guided breast biopsies for suspicious breast lesions identified at 3.0 T MRI: reasons, rates, and outcomes. Acad Radiol 2013; 20: pp. 569-575.
22. Han B.K., Schnall M.D., Orel S.G., et. al.: Outcome of MRI-guided breast biopsy. AJR Am J Roentgenol 2008; 191: pp. 1798-1804.
23. American College of Radiology (ACR) : ACR BI-RADS atlas: Breast Imaging Reporting and Data System; mammography U, magnetic resonance imaging, follow-up and outcome monitoring, data dictionary.5th ed.2013.American College of RadiologyReston (VA)
24. Kuhl C.K., Bieling H.B., Gieseke J., et. al.: Healthy premenopausal breast parenchyma in dynamic contrast-enhanced MR imaging of the breast: normal contrast medium enhancement and cyclical phase dependency. Radiology 1997; 203: pp. 137-144.
25. El Khouli R.H., Macura K.J., Kamel I.R., et. al.: The effects of applying breast compression in dynamic contrast material-enhanced MR imaging. Radiology 2014; 272: pp. 79-90.
26. Li J., Dershaw D.D., Lee C.H., et. al.: MRI follow-up after concordant, histologically benign diagnosis of breast lesions sampled by MRI-guided biopsy. AJR Am J Roentgenol 2009; 193: pp. 850-855.
27. Sung J.S., Lee C.H., Morris E.A., et. al.: Patient follow-up after concordant histologically benign imaging-guided biopsy of MRI-detected lesions. AJR Am J Roentgenol 2012; 198: pp. 1464-1469.
28. Shaylor S.D., Heller S.L., Melsaether A.N., et. al.: Short interval follow-up after a benign concordant MR-guided vacuum assisted breast biopsy—is it worthwhile?. Eur Radiol 2014; 24: pp. 1176-1185.
29. Goodman K.A., Birdwell R.L., Ikeda D.M.: Compliance with recommended follow-up after percutaneous breast core biopsy. AJR Am J Roentgenol 1998; 170: pp. 89-92.
30. Hayward J.H., Ray K.M., Wisner D.J., et. al.: Follow-up outcomes after Benign concordant MRI-guided breast biopsy. Clin Imaging 2016; 40: pp. 1034-1039.