Rationale and Objectives
We investigated if 16-slice multidetector row computed tomography (MDCT) allows correct classification of coronary plaques into calcified or noncalcified and further subclassification of noncalcified plaques into either lipid-rich with a necrotic core or fibrous.
Materials and Methods
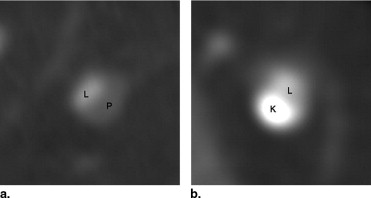
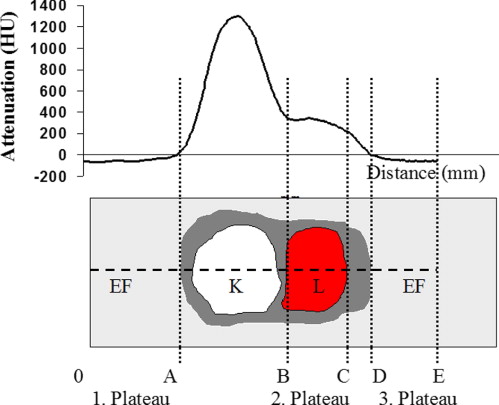
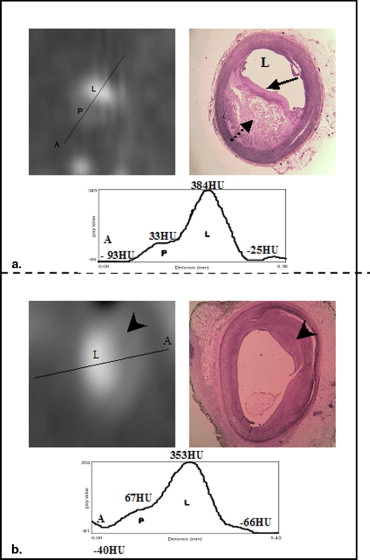
Coronary arteries of 30 isolated hearts were filled postmortem with a contrast medium and scanned with a 16-slice MDCT imager (Light Speed 16 pro, GEMS, Milwaukee, WI). Imaging parameters: collimation 16 × 0.625 mm, pitch 0.325, tube voltage 120 kV, tube current 250 mA, and gantry rotation time 500 milliseconds. The images were reformatted perpendicular to the axis of the coronary arteries (AW 4.2 software, GEMS) and analyzed by establishing attenuation profiles of the coronary cross sections (ImageJ 1.33n software, NIH, Bethesda, MD). Results were compared with the correlating histopathologic sections of the arteries.
Results
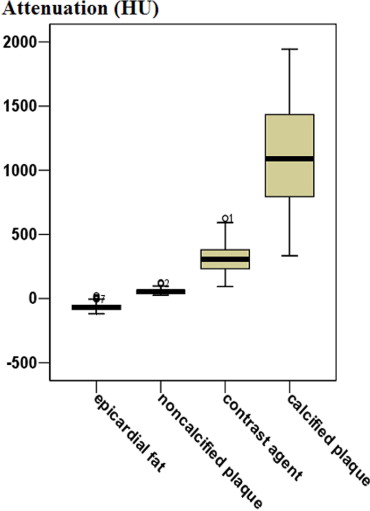
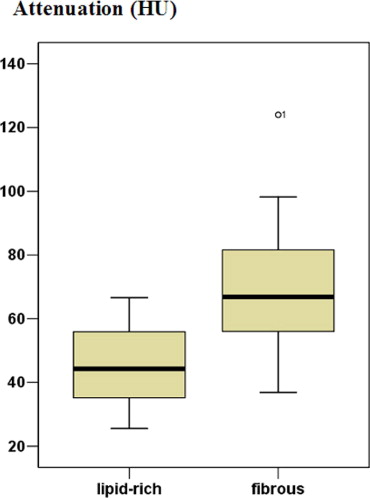
Analysis of 195 CT cross-sections showed a sensitivity and specificity for the correct classification of calcified plaques of 100% and 97.3% and for noncalcified plaques of 80.8% and 95.1%, respectively. The attenuation of epicardial fat ranged from –119 Hounsfield units (HU) to 23 HU (median –71 HU), and from 93 HU to 625 HU (308 HU) for the contrast medium. Calcified plaques showed an attenuation between 333 HU and 1944 HU (1,089 HU), noncalcified plaques between 26 HU and 124 HU (52 HU). Further subclassification of noncalcified plaques showed attenuation values between 26 HU and 67 HU (median 44 HU) for lipid-rich plaques with a necrotic core and from 37 HU to 124 HU (median 67 HU) for fibrous plaques.
Conclusions
Coronary atherosclerotic plaques can be reliably identified and classified as either calcified or noncalcified by 16-slice MDCT in postmortem studies. Further differentiation of noncalcified plaques in either lipid-rich or fibrous is not reliably feasible because of substantial overlap of the attenuation.
The pathologic mechanism that triggers acute coronary syndromes is in most cases (60%–75%) the rupture of a coronary plaque and as a consequence the formation of thrombus ( ). Plaques that are prone to rupture are called vulnerable plaques. Recent studies show that the major precursor lesion of acute coronary syndromes is the “thin-cap fibroatheroma,” a noncalcified plaque with a lipid-rich, necrotic core that is separated from the arterial lumen by a thin fibrous cap with a thickness below 65 μm ( ). Therefore the structure and composition of atherosclerotic plaques seem to be more important factors in the pathogenesis of acute coronary syndromes than the degree of stenosis caused by the lesion. To gain further information about morphologic features of arterial vessel wall lesions in patients with coronary heart disease, new imaging modalities need to be developed and established in clinical practice. One of these modalities could be multidetector row computed tomography (MDCT). Rumberger and colleagues conducted one of the first studies characterizing plaques by CT. The results of this histopathologic study showed a close relation between whole heart, coronary artery, and segmental coronary atherosclerotic plaque area and electron beam CT coronary calcium area ( ). The potential of MDCT to detect calcified and noncalcified coronary plaques has been shown in various other studies ( ). By defining certain attenuation values for the components of coronary plaques, characterization of different types of plaques, and thus detection of vulnerable plaques could be possible ( ). Kunimasa et al showed in a clinical study that 16-slice MDCT can detect noncalcified plaques in remote arteries of patients with acute coronary syndrome and that those have lower attenuation values than patients without acute coronary syndrome ( ). The search for the vulnerable plaque is supported by the results of the courage trial ( ). The latter showed medical treatment to be equal to angioplasty in stable angina. Treating only the vulnerable plaques is likely to improve the results of coronary stenting.
We therefore investigated if 16-slice MDCT allows reliable classification of coronary plaques into either calcified or noncalcified and further classification of noncalcified plaques into either lipid-rich with a necrotic core or fibrous.
Materials and methods
Material
Get Radiology Tree app to read full this article<
Computed Tomography
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Attenuation Profile Analysis
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Histopathology
Get Radiology Tree app to read full this article<
Statistical Analysis
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Results
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Table 1
Type-by-Type Analysis for Plaque Types IV–VIII
Minimum (HU) Maximum (HU) Median (HU) Type IV ( n = 4) 33 59 50 Type V ( n = 24) 26 63 44 Type VI ( n = 5) 36 67 40 Type VII ( n = 82) 333 1,944 1,089 Type VIII ( n = 21) 37 124 67
HU: Hounsfield unit.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Table 2
Cross Table Calcified Plaques
Histology Calcification+ Calcification− Total Computed tomography Calcification+ 82 3 85 Calcification− 0 110 110 Total 82 113 195
Table 3
Cross Table Noncalcified Plaques
Histology NCP+ NCP− Total Compute tomography NCP+ 59 6 65 NCP− 14 116 130 Total 73 122 195
NCP: noncalcified plaque.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Table 4
Attenuation Values of the Examined Components
Attenuation (HU) Epicardial Fat Lipid-rich NCP Fibrous NCP Contrast Agent Calcified Plaque X ⁎ <24.5 300/300 (100%) 0 0 0 0 24.5< X ⁎ <59.1 0 30/33 (90.9%) 6/21 (28.6%) 0 0 59.1< X ⁎ <101.5 0 3/33 (9.1%) 14/21 (66.7%) 2/182 (1.1%) 0 101.5< X ⁎ <494.5 0 0 1/21 (4.8%) 174/182 (95.6%) 4/82 (4.8%) 494.5< X ⁎ 0 0 0 6/182 (3.3%) 78/82 (95.1%)
NCP: noncalcified plaque.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Discussion
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Attenuation Profile Analysis
Get Radiology Tree app to read full this article<
Limitations of CT
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
References
1. Davies M.J.: Coronary disease: the pathophysiology of acute coronary syndromes. Heart 2000; 83: pp. 361-366.
2. Kolodgie F.D., Virmani R., Burke A.P., et. al.: Pathologic assessment of the vulnerable human coronary plaque. Heart 2004; 90: pp. 1385-1391.
3. Virmani R., Burke A.P., Kolodgie F.D., et. al.: Pathology of the thin-cap fibroatheroma. J Interven Cardiol 2003; 16: pp. 267-272.
4. Rumberger J.A., Simons D.B., Fitzpatrick L.A., et. al.: Coronary artery calcium area by electron-beam computed tomography and coronary atherosclerotic plaque area. Circulation 1995; 92: pp. 2157-2162.
5. Achenbach S., Moselewski F., Ropers D., et. al.: Detection of calcified and noncalcified coronary atherosclerotic plaque by contrast-enhanced, submillimeter multidetector spiral computed tomography. Circulation 2004; 109: pp. 14-17.
6. Komatsu S., Hirayama A., Omori Y., et. al.: Detection of coronary plaque by computed tomography with a novel plaque analysis system, ‘Plaque Map’, and comparison with intravascular ultrasound and angioscopy. Circ J 2005; 69: pp. 72-77.
7. Leber A., Knez A., Becker A., et. al.: Accuray of multidetector spiral computed tomography in identifying and differentiating the composition of coronary atherosclerotic plaques. J Am Coll Cardiol 2004; 43: pp. 1241-1247.
8. Nikolaou K., Becker C.R., Muders M., et. al.: Multidetector-row computed tomography and magnetic resonance imaging of atherosclerotic lesions in human ex vivo coronary arteries. Atherosclerosis 2004; 174: pp. 243-252.
9. Schroeder S., Kuettner A., Leitritz M., et. al.: Reliability of differentiating human coronary plaque morphology using contrast-enhanced multislice spiral computed tomography. J Comput Assist Tomogr 2004; 28: pp. 449-454.
10. Kunimasa T., Sato Y., Sugi K., et. al.: Evaluation by multislice computed tomography of atherosclerotic coronary artery plaques in non-culprit, remote coronary arteries of patients with acute coronary syndrome. Circ J 2005; 69: pp. 1346-1351.
11. Boden W.E., O’Rourke R.A., Teo K.K., et. al., COURAGE Trial Research Group: Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med 2007; 356: pp. 1503-1516.
12. Austen W.G., Edwards J.E., Frye R.L., et. al.: A reporting system on patients evaluated for coronary artery disease: report of the Ad Hoc Committee for Grading of Coronary Artery Disease, Council in Cardiovascular Surgery, American Heart Association. Circulation 1975; 51: pp. 5-40.
13. Stary H.C., Chandler A.B., Dinsmore R.E., et. al.: A definition of advanced types of atherosclerotic lesions and a histological classification of atherosclerosis: a report from the committee on vascular lesions of the council of arteriosclerosis, American Heart Association. ArteriosclerThromb Vasc Biol 1995; 15: pp. 1512-1531.
14. Stary H.C.: Natural history and histological classification of atherosclerotic lesions. Arterioscler Thromb Vasc Biol 2000; 20: pp. 1177-1178.
15. Virmani R., Kolodgie F., Burke A.P., et. al.: Lessons from sudden coronary death. Arterioscler Thromb Vasc Biol 2000; 20: pp. 1262-1275.
16. Kolodgie F.D., Burke A.P., Farb A., et. al.: The thin-cap fibroatheroma: a type of vulnerable plaque: the major precursor lesion to acute coronary syndromes. Curr Opin Cardiol 2001; 16: pp. 285-292.
17. Schroeder S., Kopp A., Baumbach A., et. al.: Noninvasive detection and evaluation of atherosclerotic coronary plaques with multislice computed tomography. J Am Coll Cardiol 2001; 37: pp. 1430-1435.
18. Becker C.R., Nikolaou K., Muders M., et. al.: Ex vivo coronary atherosclerotic plaque characterization with multi-detector row CT. Eur Radiol 2003; 13: pp. 2094-2098.
19. Viles-Gonzalez J.F., Poon M., Sanz J., et. al.: In vivo 16-slice, multidetector-row computed tomography for the assessment of experimental atherosclerosis. Circulation 2004; 110: pp. 1467-1472.
20. Hamoir X.L., Flohr T., Hamoir V., et. al.: Coronary arteries: assessment of image quality and optimal reconstruction window in retrospective ECG-gated multislice CT at 375-ms gantry rotation. Eur Radiol 2005; 15: pp. 296-304.
21. Hong C., Becker C.R., Hubert A., et. al.: ECG-gated, retrospectively reconstructed multidetector-row CT coronary angiography: effect of varying trigger delay on image quality. Radiology 2001; 220: pp. 712-717.
22. Mao S., Budoff M.J., Bin L., et. al.: Optimal ECG trigger point in electron-beam CT studies: three methods for minimizing motion artifacts. Acad Radiol 2001; 8: pp. 1107-1115.
23. Achenbach S., Ropers D., Kuettner A., et. al.: Contrast-enhanced coronary artery visualization by dual-source computed tomography-initial experience. Eur J Radiol 2006; 57: pp. 331-335.
24. Schroeder S., Kopp A., Ohnesorge B., et. al.: Accuracy and reliability of quantitative measurements in coronary arteries by multi-slice computed tomography: experimental and initial clinical results. Clin Radiol 2001; 56: pp. 466-474.
25. Cademartiri F., La Grutta L., Runza G., et. al.: Influence of convolution filtering on coronary plaque attenuation values: observations in an ex vivo model of multislice computed tomography coronary angiography. Eur Radiol 2007; 17: pp. 1842-1849.
26. Cademartiri F., Mollet N.R., Runza G., et. al.: Influence of intracoronary attenuation on coronary plaque measurements using multislice computed tomography: observations in an ex vivo model of coronary computed tomography angiography. Eur Radiol 2005; 15: pp. 1426-1431.
27. Schroeder S., Kuettner A., Wojak T., et. al.: Non-invasive evaluation of atherosclerosis with contrast enhanced 16 slice spiral computed tomography: results of ex vivo investigations. Heart 2004; 90: pp. 1471-1475.
28. Nikolaou K., Knez A., Sagmeister S., et. al.: Assessment of myocardial infarctions using multidetector-row computed tomography. Am J Roentgenol 2004; 28: pp. 286-292.
29. Ferencik M., Chan R.C., Achenbach S., et. al.: Arterial wall imaging: evaluation with 16-Section multidetector CT in blood vessel phantoms and ex vivo coronary arteries. Radiology 2006; 240: pp. 708-716.
30. Maseri A., Fuster V.: Is there a vulnerable plaque?. Circulation 2003; 107: pp. 2068-2071.