Rationale and Objectives
The purpose of this study was to critically appraise and compare the diagnostic performance of imaging modalities that are used for the diagnosis of intussusception and methods used in the treatment of ileocolic intussusception.
Methods
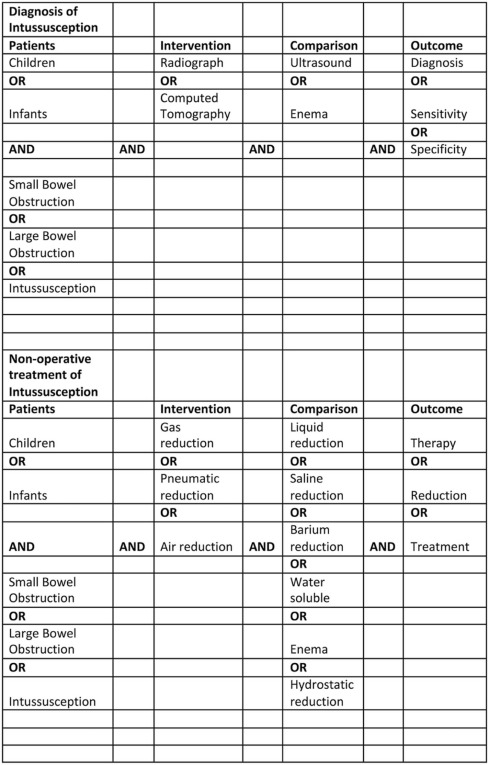
A focused clinical question was constructed and the literature was searched using the patient, intervention, comparison, outcome (PICO) method comparing radiography, ultrasound, and computed tomography in the detection of intussusception. The same methods were used to compare pneumatic (gas) reduction and hydrostatic (liquid) reduction using saline, water-soluble contrast, and barium. Retrieved articles were appraised and assigned a level of evidence based on the Oxford University Centre for Evidence-Based Medicine hierarchy of validity for diagnostic studies.
Results
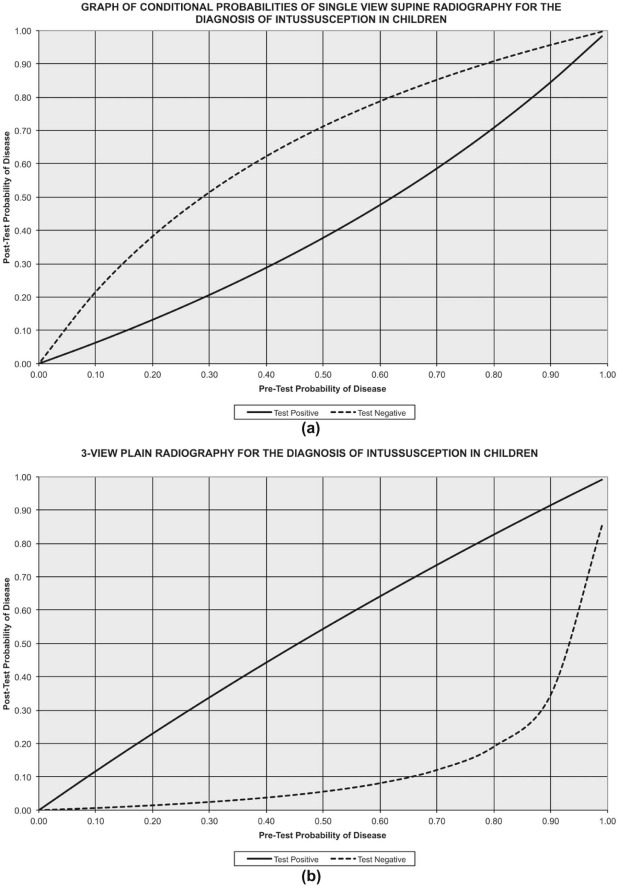
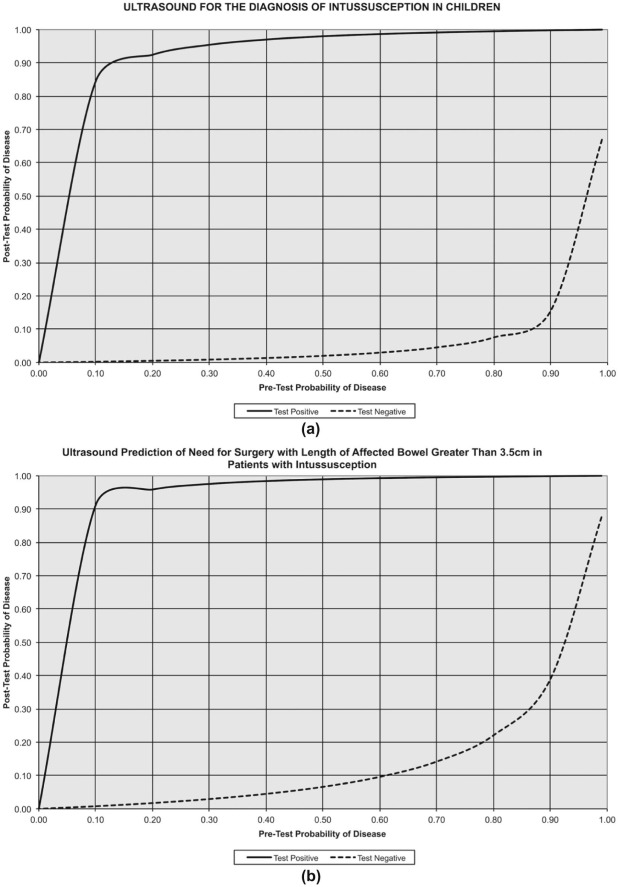
The retrieved sensitivity for the diagnosis of intussusception using plain radiography is 48% (95% confidence interval [CI], 44%–52%), with a specificity of 21% (95% CI, 18%–24%). The retrieved sensitivity for the diagnosis of intussusception using ultrasound is 97.9% (95% CI, 95%–100%), with a specificity of 97.8% (95% CI, 97%–99%). Based on a good quality meta-analysis, the combined success rate of gas enema reduction was shown to be 82.7% (95% CI, 79.9%–85.6%) compared to a combined success rate of 69.6% (95% CI, 65.0%–74.1%) for liquid enema reduction.
Conclusions
The best available evidence recommends ultrasound as the diagnostic modality of choice for the diagnosis of ileocolic intussusception in children. In stable children without signs of peritonism, nonoperative reduction is the treatment of choice. Pneumatic (gas) reduction enema has been shown to be superior to hydrostatic (liquid) enema reduction.
Introduction
Intussusception is an invagination of the bowel into itself, usually involving both small and large bowel. The more proximal bowel that herniates into the more distal bowel is called the intussusceptum, and the bowel that contains it is called the intussuscipiens . As the intussusceptum and its mesentery telescope into the intussuscipiens, there is impairment of venous and lymphatic return, which leads to bowel wall edema. If untreated, this will progress to bowel ischemia, necrosis, and perforation. Intussusception can occur in large or small bowel, but is most commonly ileocecal .
Children with intussusception may have variable presentations, making the diagnosis often a challenging one. The classic triad of vomiting, colicky abdominal pain, and bloody (so called “red currant jelly”) stools is seen in less than 50% of patients . Indeed, the presence of bloody stool is often a late sign signifying delayed presentation and ischemic bowel.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Research Questions
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Literature Search
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Appraisal
Diagnosis of Intussusception
Radiography
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Table 1
Test Performances for Diagnosis of Intussusception in Children
Diagnosis of Intussusception in Children Radiography
(Single View) 3-View Radiography
(Supine, Prone, and Left Lateral Decubitus) Ultrasound Ultrasound to Predict Need for Surgery Selected study Morrison et al. Roskind et al. Hryhorczuk and Strouse Munden et al. Sensitivity, % 48% (95% CI, 44%–52%) 100% (95% CI, 79.1%–100%) 97.9% (95% CI, 95%–100%) 93% (95% CI, 79%–100%) Specificity, % 21% (95% CI, 18%–24%) 17.4% (95% CI, 11.1%–26.1%) 97.8% (95% CI, 97%–99%) 100% (95% CI, 100%) Likelihood ratio + test 0.6 1.2 49.0 93.0 Likelihood ratio − test 2.4 0 0.02 0.07
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Ultrasound
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Computed Tomography
Get Radiology Tree app to read full this article<
Treatment of Intussusception
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
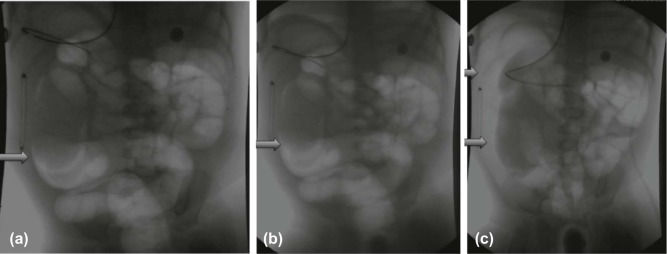
Pneumatic (Gas) Reduction
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Table 2
Test Performances (Benefits and Harms) in the Treatment of Intussusception in Children
Nonoperative Treatment of Intussusception in Children Gas Reduction Enema Liquid Reduction Enema_P_ Value Meta-analysis Sadigh et al. Sadigh et al. Combined success rate 82.7% (95% CI, 79.9%–85.6%) 69.6% (95% CI, 65.0%–74.1%) <.001 Pooled perforation rate 0.39% (95% CI, 0.23%–0.55%) 0.43% (95% CI, 0.24%–0.62%) .73 Early recurrence rate (within 48 h) 3.1% (95% CI, 1.1%–5.1%) 3.2% (85% CI, 1.9%–4.5%) .93
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Hydrostatic/Liquid Reduction (Saline or Water-soluble Contrast Media)
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Barium Reduction
Get Radiology Tree app to read full this article<
Delayed Repeat Enema
Get Radiology Tree app to read full this article<
Applicability to Practice
Diagnosis of Intussusception
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Treatment of Intussusception
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Evaluation of the Evidence
Diagnosis of Intussusception
Get Radiology Tree app to read full this article<
Treatment of Intussusception
Get Radiology Tree app to read full this article<
References
1. Applegate K.E.: Intussusception in children: evidence-based diagnosis and treatment. Pediatr Radiol 2009; 39: pp. S140-S143.
2. Kitagawa S., Miqdady M.: Intussusception in children.2016. UpToDate. Topic 5898
3. Blanch A.J., Perel S.B., Acworth J.P.: Paediatric intussusception: epidemiology and outcome. Emerg Med Australas 2007; 19: pp. 45-50.
4. Samad L., Marven S., El Bashir H., et. al.: Prospective surveillance study of the management of intussusception in UK and Irish infants. Br J Surg 2012; 99: pp. 411-415.
5. Parashar U.D., Holman R.C., Cummings K.C., et. al.: Trends in intussusception-associated hospitalizations and deaths among US infants. Pediatrics 2000; 106: pp. 1413-1421.
6. Navarro O., Daneman A.: Intussusception. Part 3: diagnosis and management of those with an identifiable or predisposing cause and those that reduce spontaneously. Pediatr Radiol 2004; 34: pp. 305-312. quiz 369
7. Haynes R.B.: Of studies, summaries, synopses, and systems: the “4S” evolution of services for finding current best evidence. Evid Based Ment Health 2001; 4: pp. 37-39.
8. Morrison J., Lucas N., Gravel J.: The role of abdominal radiography in the diagnosis of intussusception when interpreted by pediatric emergency physicians. J Pediatr 2009; 155: pp. 556-559.
9. Roskind C.G., Kamdar G., Ruzal-Shapiro C.B., et. al.: Accuracy of plain radiographs to exclude the diagnosis of intussusception. Pediatr Emerg Care 2012; 28: pp. 855-858.
10. Hryhorczuk A.L., Strouse P.J.: Validation of US as a first-line diagnostic test for assessment of pediatric ileocolic intussusception. Pediatr Radiol 2009; 39: pp. 1075-1079.
11. Munden M.M., Bruzzi J.F., Coley B.D., et. al.: Sonography of pediatric small-bowel intussusception: differentiating surgical from nonsurgical cases. AJR Am J Roentgenol 2007; 188: pp. 275-279.
12. West K.W., Stephens B., Vane D.W., et. al.: Intussusception: current management in infants and children. Surgery 1987; 102: pp. 704-710.
13. Howick J., Chalmers I., Glasziou P., et. al.: Oxford Centre for Evidence-Based Medicine. The 2011 Oxford CEBM Evidence Levels of Evidence (Introductory Document) http://www.cebm.net/index.aspx?o=5653
14. Navarro O., Dugougeat F., Kornecki A., et. al.: The impact of imaging in the management of intussusception owing to pathologic lead points in children. A review of 43 cases. Pediatr Radiol 2000; 30: pp. 594-603.
15. Sadigh G., Zou K.H., Razavi S.A., et. al.: Meta-analysis of air versus liquid enema for intussusception reduction in children. AJR Am J Roentgenol 2015; 205: pp. W542-W549.
16. Gray M.P., Li S.H., Hoffmann R.G., et. al.: Recurrence rates after intussusception enema reduction: a meta-analysis. Pediatrics 2014; 134: pp. 110-119.
17. Gorenstein A., Raucher A., Serour F., et. al.: Intussusception in children: reduction with repeated, delayed air enema. Radiology 1998; 206: pp. 721-724.
18. Navarro O.M., Daneman A., Chae A.: Intussusception: the use of delayed, repeated reduction attempts and the management of intussusceptions due to pathologic lead points in pediatric patients. AJR Am J Roentgenol 2004; 182: pp. 1169-1176.
19. Beres A.L., Baird R.: An institutional analysis and systematic review with meta-analysis of pneumatic versus hydrostatic reduction for pediatric intussusception. Surgery 2013; 154: pp. 328-334.
20. Shiels W.E., Kirks D.R., Keller G.L., et. al.: John Caffey Award. Colonic perforation by air and liquid enemas: comparison study in young pigs. AJR Am J Roentgenol 1993; 160: pp. 931-935.
21. Fallon S.C., Kim E.S., Naik-Mathuria B.J., et. al.: Needle decompression to avoid tension pneumoperitoneum and hemodynamic compromise after pneumatic reduction of pediatric intussusception. Pediatr Radiol 2013; 43: pp. 662-667.
22. Kaiser A.D., Applegate K.E., Ladd A.P.: Current success in the treatment of intussusception in children. Surgery 2007; 142: pp. 469-475. discussion 475-7
23. Flaum V., Schneider A., Gomes Ferreira C., et. al.: Twenty years’ experience for reduction of ileocolic intussusceptions by saline enema under sonography control. J Pediatr Surg 2016; 51: pp. 179-182.
24. Nayak D., Jagdish S.: Ultrasound guided hydrostatic reduction of intussusception in children by saline enema: our experience. Indian J Surg 2008; 70: pp. 8-13.
25. Sanchez T.R., Doskocil B., Stein-Wexler R.: Nonsurgical management of childhood intussusception: retrospective comparison between sonographic and fluoroscopic guidance. J Ultrasound Med 2015; 34: pp. 59-63.
26. Ito Y., Kusakawa I., Murata Y., et. al.: Japanese guidelines for the management of intussusception in children, 2011. Pediatr Int 2012; 54: pp. 948-958.
27. Daneman A., Navarro O.: Intussusception. Part 2: an update on the evolution of management. Pediatr Radiol 2004; 34: pp. 97-108. quiz 187
28. Pazo A., Hill J., Losek J.D.: Delayed repeat enema in the management of intussusception. Pediatr Emerg Care 2010; 26: pp. 640-645.
29. Lautz T.B., Thurm C.W., Rothstein D.H.: Delayed repeat enemas are safe and cost-effective in the management of pediatric intussusception. J Pediatr Surg 2015; 50: pp. 423-427.