Rationale and Objectives
The purpose of this study was to critically appraise and compare the diagnostic performance of imaging modalities that are used for the diagnosis of upper and lower gastrointestinal (GI) tract obstruction in neonates and infants.
Methods
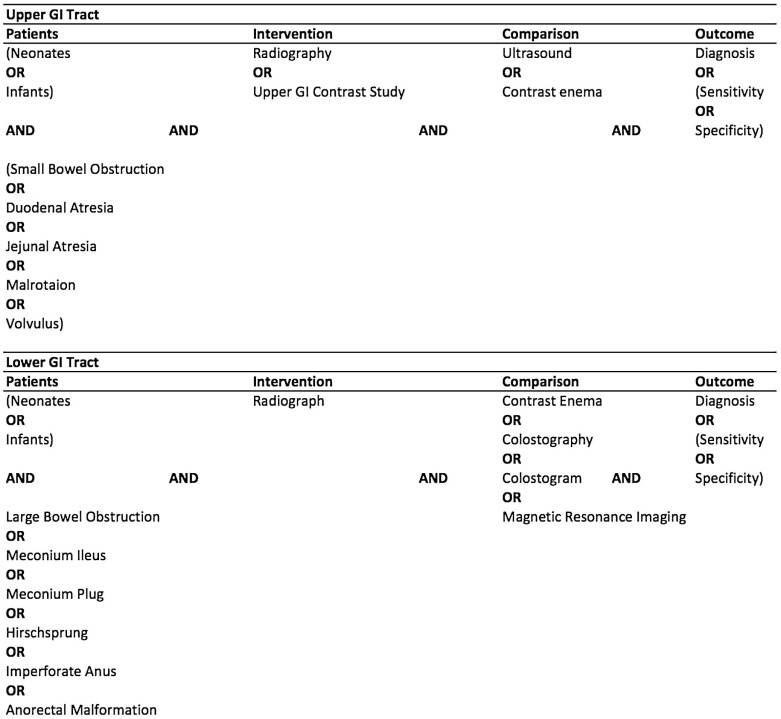
A focused clinical question was constructed and the literature was searched using the patient, intervention, comparison, outcome method comparing radiography, upper GI contrast study, and ultrasound in the detection of upper GI tract obstruction such as duodenal atresia and stenosis, jejunal and ileal atresia, and malrotation and volvulus. The same methods were used to compare radiography and contrast enema in the detection of lower GI tract obstruction such as meconium plug syndrome, meconium ileus, Hirschsprung disease, and imperforate anus. Retrieved articles were appraised and assigned a level of evidence based on the Oxford University Centre for Evidence-Based Medicine hierarchy of validity for diagnostic studies.
Results
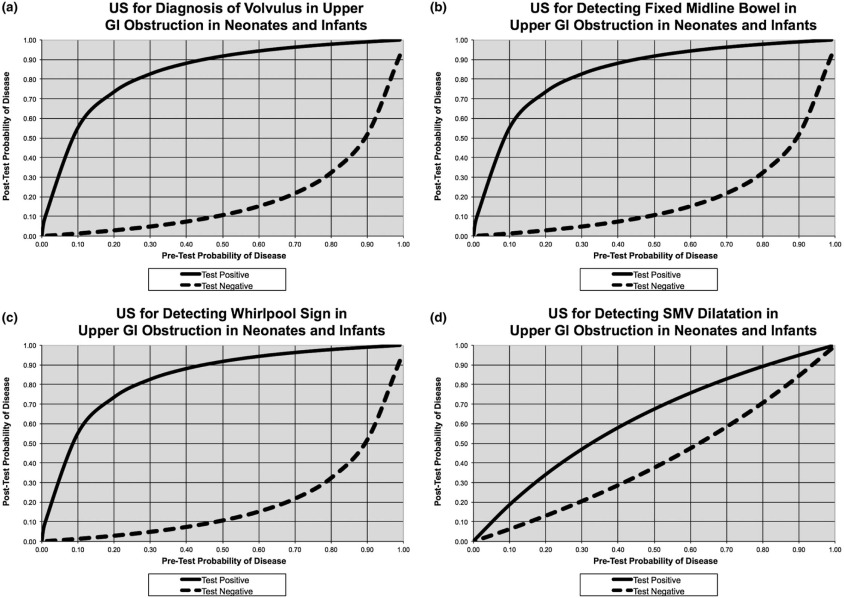
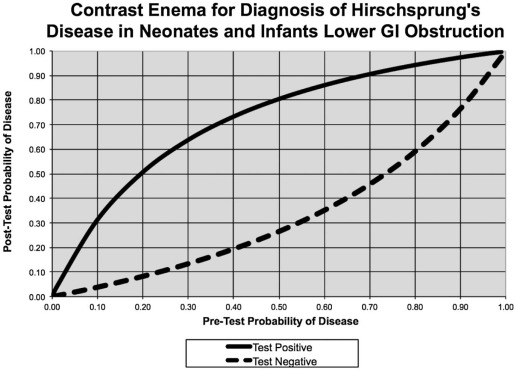
There were no sensitivities/specificities available for the imaging diagnosis of duodenal atresia or stenosis, jejunal or ileal atresias, meconium plug, and meconium ileus or for the use of cross-table lateral radiography for the diagnosis of rectal pouch distance from skin in imperforate anus. The retrieved sensitivity for the detection of malrotation on upper GI contrast study is 96%, and the sensitivity for the diagnosis of midgut volvulus on upper GI contrast study is 79%. The retrieved sensitivity and specificity for the detection of malrotation with volvulus on ultrasound were 89% and 92%, respectively. The retrieved sensitivity and specificity for the detection of Hirschsprung disease on contrast enema were 70% and 83%, respectively. The retrieved sensitivity of invertogram for the diagnosis of rectal pouch distance from skin in imperforate anus is 27%. The retrieved sensitivities of perineal ultrasound and colostography for the diagnosis of rectal pouch distance from skin in imperforate anus were 86% and 100%, respectively.
Conclusions
There is limited evidence for the imaging diagnosis of duodenal atresia and stenosis, jejunal and ileal atresias, meconium plug, meconium ileus, and imperforate anus, with recommended practice based mainly on low-quality evidence or expert opinion. The available evidence supports the use of upper GI contrast study for the diagnosis of malrotation and volvulus, with ultrasound as an adjunct to diagnosis. Contrast enema is useful in the investigation of suspected Hirschsprung disease, but a negative study does not outrule the condition. Colostography is the investigation of choice for the work-up of infants with complex anorectal malformations before definitive surgical repair.
Introduction
Duodenal atresia occurs in 1 in 5000–10,000 live births. In one-third of cases, it is an isolated anomaly. In one-third of cases, it is associated with Down syndrome. It can also be associated with other congenital abnormalities, especially cardiac and esophageal anomalies. It results from failure of the duodenum to recanalize during weeks 8–10 of gestation . Neonates typically present with bilious or nonbilious vomiting in the first 24 hours after birth.
Infants with less severe duodenal stenosis may have delayed presentation with frequent vomiting and failure to thrive. Duodenal stenosis is often due to the presence of a duodenal web or may be secondary to extrinsic compression from an annular pancreas, malrotation, or a preduodenal portal vein .
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Ask
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Search
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Appraise
Upper GI Tract
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Duodenal Atresia and Stenosis, Jejunal, and Ileal Atresia
Get Radiology Tree app to read full this article<
Radiography
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Upper GI contrast study
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Contrast enema
Get Radiology Tree app to read full this article<
Malrotation and Volvulus
Radiography
Get Radiology Tree app to read full this article<
Upper GI contrast study
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Contrast enema
Get Radiology Tree app to read full this article<
Ultrasound
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
TABLE 1
Test Performances for the Diagnosis of Upper and Lower GI Tract Obstruction in Neonates and Infants
Selected Study Upper Gastrointestinal (GI) Tract Lower GI Tract US Volvulus US with Fixed Midline Bowel US with Whirlpool Sign US with SMV Dilatation Contrast Enema for Hirschsprung Disease Sensitivity, % 89 89 89 56 70 Specificity, % 92 92 92 73 83 Accuracy 0.81 0.81 0.81 0.60 0.70
SMV, superior mesenteric vein; US, ultrasound.
Get Radiology Tree app to read full this article<
Lower GI Tract
Get Radiology Tree app to read full this article<
Meconium Plug Syndrome and MI
Get Radiology Tree app to read full this article<
Radiography
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Contrast enema
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Hirschsprung Disease
Contrast enema
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Imperforate Anus
Get Radiology Tree app to read full this article<
Radiography
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Ultrasound
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Colostography
Get Radiology Tree app to read full this article<
Magnetic Resonance Imaging (MRI)
Get Radiology Tree app to read full this article<
Apply
Upper GI Tract
Duodenal Atresia and Stenosis, Jejunal, and Ileal Atresia
Get Radiology Tree app to read full this article<
Malrotation and Volvulus
Get Radiology Tree app to read full this article<
Lower GI Tract
Meconium Plug Syndrome and MI
Get Radiology Tree app to read full this article<
Hirschsprung Disease
Get Radiology Tree app to read full this article<
Imperforate Anus
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Evaluate
Upper GI Tract
Duodenal Atresia and Stenosis, Jejunal, and Ileal Atresia
Get Radiology Tree app to read full this article<
Malrotation and Volvulus
Get Radiology Tree app to read full this article<
Lower GI Tract
Meconium Plug Syndrome and MI
Get Radiology Tree app to read full this article<
Hirschsprung Disease
Get Radiology Tree app to read full this article<
Imperforate Anus
Get Radiology Tree app to read full this article<
References
1. Wesson D.E.: Intestinal atresia.2014.Wolters Kluwer Up to date; Available at http://uptodate.com
2. Gomella T.C., Cunningham M., Eyal F.G.: Neonatology: management, procedures, on-call problems, diseases, and drugs.6th ed.2009.McGraw HillNew York
3. Best K.E., Tennant P.W., Addor M.C., et. al.: Epidemiology of small intestinal atresia in Europe: a register-based study. Arch Dis Child Fetal Neonatal Ed 2012; 97: pp. F353-F358.
4. Applegate K.E., Anderson J.M., Klatte E.C.: Intestinal malrotation in children: a problem-solving approach to the upper gastrointestinal series. Radiographics 2006; 26: pp. 1485-1500.
5. Millar A.J., Rode H., Cywes S.: Malrotation and volvulus in infancy and childhood. Semin Pediatr Surg 2003; 12: pp. 229-236.
6. Brandt M.L.: Intestinal malrotation.2015.Wolters Kluwer Up to date; Available at http://www.uptodate.com
7. Torres A.M., Ziegler M.M.: Malrotation of the intestine. World J Surg 1993; 17: pp. 326-331.
8. Filston H.C., Kirks D.R.: Malrotation—the ubiquitous anomaly. J Pediatr Surg 1981; 16: pp. 614-620.
9. Strouse P.J.: Disorders of intestinal rotation and fixation (“malrotation”). Pediatr Radiol 2004; 34: pp. 837-851.
10. Maxson R.T., Franklin P.A., Wagner C.W.: Malrotation in the older child: surgical management, treatment, and outcome. Am Surg 1995; 61: pp. 135-138.
11. Powell D.M., Othersen H.B., Smith C.D.: Malrotation of the intestines in children: the effect of age on presentation and therapy. J Pediatr Surg 1989; 24: pp. 777-780.
12. Spigland N., Brandt M.L., Yazbeck S.: Malrotation presenting beyond the neonatal period. J Pediatr Surg 1990; 25: pp. 1139-1142.
13. Burge D., Drewett M.: Meconium plug obstruction. Pediatr Surg Int 2004; 20: pp. 108-110.
14. Keckler S.J., St Peter S.D., Spilde T.L., et. al.: Current significance of meconium plug syndrome. J Pediatr Surg 2008; 43: pp. 896-898.
15. Sabharwal S., Borowitz D.: Cystic fibrosis: overview of gastrointestinal disease. Up to date2015.
16. Cuschieri A.: Anorectal anomalies associated with or as part of other anomalies. Am J Med Genet 2002; 110: pp. 122-130.
17. Haynes R.B.: Of studies, summaries, synopses, and systems: the “4S” evolution of services for finding current best evidence. Evid Based Ment Health 2001; 4: pp. 37-39.
18. Kerr J.M.: Small bowel imaging: CT enteroclysis or barium enteroclysis? Critically appraised topic. Abdom Imaging 2008; 33: pp. 31-33.
19. Daskalogiannaki M., Prassopoulos P., Katrinakis G., et. al.: Splenic involvement in lymphomas. Evaluation on serial CT examinations. Acta Radiol 2001; 42: pp. 326-332.
20. American College of Physicians Journal Club Web site : Available at http://www.acpjc.org Accessed February 7, 2012
21. Deignan R.W., Malone D.E., Taylor S., et. al.: Improving visualization of distal and terminal ileum during the small bowel meal: an evaluation of fluoroscopic manoeuvres. Clin Radiol 1995; 50: pp. 548-552.
22. Gourtsoyiannis N., Grammatikakis J., Prassopoulos P.: Role of conventional radiology in the diagnosis and staging of gastrointestinal tract neoplasms. Semin Surg Oncol 2001; 20: pp. 91-108.
23. Elsayes K.M., Al-Hawary M.M., Jagdish J., et. al.: CT enterography: principles, trends, and interpretation of findings. Radiographics 2010; 30: pp. 1955-1970.
24. Thipphavong S., Millward S.F., Elliott J.A.: Balloon angioplasty versus primary stenting of ostial atherosclerotic renal arterial stenoses: critically appraised topic. Can Assoc Radiol J 2004; 55: pp. 108-110.
25. Hajivassiliou C.A.: Intestinal obstruction in neonatal/pediatric surgery. Semin Pediatr Surg 2003; 12: pp. 241-253.
26. Virgone C., D’antonio F., Khalil A., et. al.: Accuracy of prenatal ultrasound in detecting jejunal and ileal atresia: systematic review and meta-analysis. Ultrasound Obstet Gynecol 2015; 45: pp. 523-529.
27. Brantberg A., Blaas H.G., Salvesen K.A., et. al.: Fetal duodenal obstructions: increased risk of prenatal sudden death. Ultrasound Obstet Gynecol 2002; 20: pp. 439-446.
28. Grosfeld J.L., Rescorla F.J.: Duodenal atresia and stenosis: reassessment of treatment and outcome based on antenatal diagnosis, pathologic variance, and long-term follow-up. World J Surg 1993; 17: pp. 301-309.
29. Ha H.K., Ko G.Y., Yu E.S., et. al.: Intestinal tuberculosis with abdominal complications: radiologic and pathologic features. Abdom Imaging 1999; 24: pp. 32-38.
30. Kadian Y.S., Rattan K.N.: Congenital pyloric atresia with distal duodenal atresia—role of CT scan. J Neonatal Surg 2014; 3: pp. 37.
31. Chen Q.J., Gao Z.G., Tou J.F., et. al.: Congenital duodenal obstruction in neonates: a decade’s experience from one center. World J Pediatr 2014; 10: pp. 238-244.
32. Sizemore A.W., Rabbani K.Z., Ladd A., et. al.: Diagnostic performance of the upper gastrointestinal series in the evaluation of children with clinically suspected malrotation. Pediatr Radiol 2008; 38: pp. 518-528.
33. Stringer D.A.: Pediatric gastrointestinal imaging.1st ed.1989.BC DeckerOntario
34. Chao H.C., Kong M.S., Chen J.Y., et. al.: Sonographic features related to volvulus in neonatal intestinal malrotation. J Ultrasound Med 2000; 19: pp. 371-376.
35. Dufour D., Delaet M.H., Dassonville M., et. al.: Midgut malrotation, the reliability of sonographic diagnosis. Pediatr Radiol 1992; 22: pp. 21-23.
36. Quail M.A.: Question 2. Is Doppler ultrasound superior to upper gastrointestinal contrast study for the diagnosis of malrotation?. Arch Dis Child 2011; 96: pp. 317-318.
37. Carlyle B.E., Borowitz D.S., Glick P.L.: A review of pathophysiology and management of fetuses and neonates with meconium ileus for the pediatric surgeon. J Pediatr Surg 2012; 47: pp. 772-781.
38. Noblett H.R.: Treatment of uncomplicated meconium ileus by Gastrografin enema: a preliminary report. J Pediatr Surg 1969; 4: pp. 190-197.
39. Copeland D.R., St Peter S.D., Sharp S.W., et. al.: Diminishing role of contrast enema in simple meconium ileus. J Pediatr Surg 2009; 44: pp. 2130-2132.
40. Cuenca A.G., Ali A.S., Kays D.W., et. al.: “Pulling the plug”—management of meconium plug syndrome in neonates. J Surg Res 2012; 175: pp. e43-e46.
41. Karimi A., Gorter R.R., Sleeboom C., et. al.: Issues in the management of simple and complex meconium ileus. Pediatr Surg Int 2011; 27: pp. 963-968.
42. Wagner J.P., Shekherdimian S.: Hirschsprung disease.2015. http://emedicine.medscape.com/article/178493-overview Accessed November 29, 2015
43. de Lorijn F., Kremer L.C., Reitsma J.B., et. al.: Diagnostic tests in Hirschsprung disease: a systematic review. J Pediatr Gastroenterol Nutr 2006; 42: pp. 496-505.
44. Noviello C., Cobellis G., Romano M., et. al.: Diagnosis of Hirschsprung’s disease: an age-related approach in children below or above one year. Colorectal Dis 2010; 12: pp. 1044-1048.
45. de Lorijn F., Reitsma J.B., Voskuijl W.P., et. al.: Diagnosis of Hirschsprung’s disease: a prospective, comparative accuracy study of common tests. J Pediatr 2005; 146: pp. 787-792.
46. Diamond I.R., Casadiego G., Traubici J., et. al.: The contrast enema for Hirschsprung disease: predictors of a false-positive result. J Pediatr Surg 2007; 42: pp. 792-795.
47. Levitt M., Pena A.: Pediatric imperforate anus surgery workup.2013. http://emedicine.medscape.com/article/933524-overview Accessed November 29, 2015
48. Narasimharao K.L., Prasad G.R., Katariya S., et. al.: Prone cross-table lateral view: an alternative to the invertogram in imperforate anus. AJR Am J Roentgenol 1983; 140: pp. 227-229.
49. Niedzielski J.K.: Invertography versus ultrasonography and distal colostography for the determination of bowel-skin distance in children with anorectal malformations. Eur J Pediatr Surg 2005; 15: pp. 262-267.
50. Wetherill C., Sutcliffe J.: Hirschsprung disease and anorectal malformation. Early Hum Dev 2014; 90: pp. 927-932.
51. Podberesky D.J., Towbin A.J., Eltomey M.A., et. al.: Magnetic resonance imaging of anorectal malformations. Magn Reson Imaging Clin N Am 2013; 21: pp. 791-812.
52. Farhataziz N., Engels J.E., Ramus R.M., et. al.: Fetal MRI of urine and meconium by gestational age for the diagnosis of genitourinary and gastrointestinal abnormalities. AJR Am J Roentgenol 2005; 184: pp. 1891-1897.
53. Applegate K.E.: Evidence-based diagnosis of malrotation and volvulus. Pediatr Radiol 2009; 39: pp. S161-S163.