Rational and Objectives
The objective of this study was to compare the stationary digital breast tomosynthesis (s-DBT) system to a conventional mammography system in a study of breast specimens. Radiologist evaluation of image quality was assessed in a reader study. This study represents the first human tissue imaging with the novel carbon nanotube–based s-DBT device.
Materials and Methods
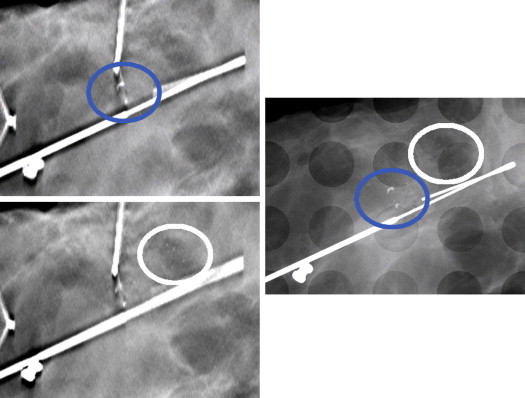
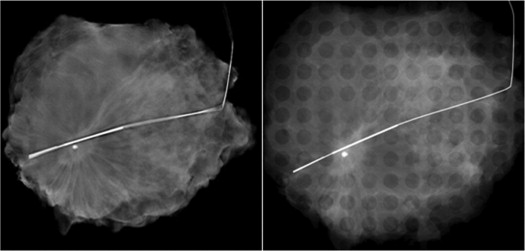
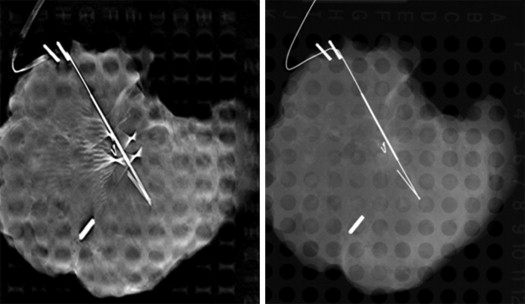
Thirty-nine patients, with known breast lesions (Breast Imaging Reporting and Data System 4 or 5) by conventional mammography and scheduled for needle localization biopsy, were recruited under an institutional review board–approved protocol. Specimen images were obtained using a two-dimensional (2D) mammography system with a ×1.8 magnification factor and an s-DBT system without a high magnification factor. A reader study was performed with four breast fellowship-trained radiologists over two separate sessions. Malignancy scores were recorded for both masses and microcalcifications (MCs). Reader preference between the two modalities for MCs, masses, and surgical margins was recorded.
Results
The s-DBT system was found to be comparable to magnified 2D mammography for malignancy diagnosis. Readers preferred magnified 2D mammography for MC visualization ( P < .05). However, readers trended toward a preference for s-DBT with respect to masses and surgical margin assessment.
Conclusions
Here, we report on the first human data acquired using a stationary digital breast tomosynthesis system. The novel s-DBT system was found to be comparable to magnified 2D mammography imaging for malignancy diagnosis. Given the trend of preference for s-DBT over 2D mammography for both mass visibility and margin assessment, s-DBT could be a viable alternative to magnified 2D mammography for imaging breast specimens.
Malignant lesions in the breast can be difficult to visualize using full-field digital mammography (FFDM) when significant tissue overlap is present. Tissue overlap is most apparent in breast tissue that is thick and radiographically dense. Digital breast tomosynthesis (DBT) uses a small number of angular projections to reconstruct a pseudo–three-dimensional (3D)volume. Recent studies have shown an increase in the area under the curve (AUC) when using a combination of DBT and FFDM compared to FFDM alone . Recall rates for benign cases significantly decrease when using a combination of DBT and FFDM . However, for cases with microcalcifications (MCs), the use of DBT along with an FFDM image has shown no significant improvement in the AUC .
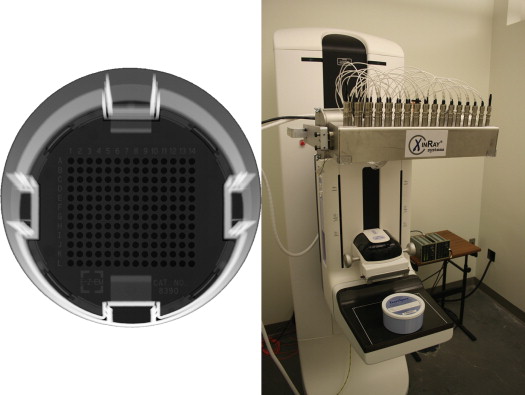
Current DBT systems use a single X-ray source which is translated over an angular span that typically covers between 15° and 50° . Larger angular spans sample more of the Fourier domain which reduces out-of-plane reconstruction artifacts. Translating a source over a larger angular span requires longer acquisition times, which leads to patient motion artifacts . These single-source systems also suffer from poor spatial resolution because of focal spot blurring from the tube motion . We have developed a stationary digital breast tomosynthesis (s-DBT) technology that uses a novel multiple focal-spot X-ray source array with carbon nanotubes (CNTs) as the field emission electron source . This stationary approach can increase acquisition speed and eliminate the focal spot motion. It has been shown that the s-DBT device offers significant improvement in image quality, including improved modulation transfer function (MTF) and lesion conspicuity in breast phantom studies .
Get Radiology Tree app to read full this article<
Materials and methods
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Results
Get Radiology Tree app to read full this article<
Table 1
Calculated Sensitivity and Specificity Values by Modality and Reader
Reader Sensitivity Specificity FFDM s-DBT FFDM s-DBT 1 24/24 (1.00) 23/25 (0.92) 4/14 (0.29) 2/13 (0.15) 2 21/25 (0.84) 19/25 (0.76) 5/14 (0.36) 7/14 (0.50) 3 24/25 (0.96) 25/25 (1.00) 0/13 (0.00) 0/13 (0.00) 4 23/25 (0.92) 25/25 (1.00) 4/14 (0.29) 2/14 (0.14)
FFDM, full-field digital mammography modality; s-DBT, stationary digital breast tomosynthesis.
Values were calculated from malignancy scores. Malignancy scores from 3 to 5 were considered positive for disease.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Table 2
Results of McNemar Test for Discordance Between the Two Modalities for All Four Readers
Modality = FFDM Modality = s-DBT Negative Positive Subtotal Reader 1 ( P = .5637) Negative 1 1 2 Positive 2 32 34 Subtotal 3 33 36 Reader 2 ( P = .2482) Negative 5 4 9 Positive 8 22 30 Subtotal 13 26 39 Reader 3 ( P = NA) Negative 0 0 0 Positive 0 35 35 Subtotal 0 35 35 Reader 4 ( P = .0455) Negative 2 4 6 Positive 0 33 33 Subtotal 2 37 39
FFDM, full-field digital mammography modality; s-DBT, stationary digital breast tomosynthesis.
Insignificant discordance was found between the two modalities for readers 1, 2, and 3. In the case of reader 4, diagnostics based on two modalities are likely to be different.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Table 3
Average Reader Preference for the Shape/Morphology of Masses, Microcalcification Assessment, and Margin Assessment
Reader Masses Microcalcifications Margins Mean SD_P_ Value Mean SD_P_ Value Mean SD_P_ Value 1 −1.02 1.40 <.05 −1.80 1.01 <.05 −0.44 1.35 <.05 2 0.18 1.20 .4094 −0.54 0.70 <.05 0.19 1.14 .2984 3 0.75 1.35 <.05 −0.20 0.98 .259 0.70 1.35 <.05 4 0.08 0.86 .5800 −0.62 0.52 <.05 0.21 0.72 .0743 Overall 0.07 1.34 — −0.70 0.95 — 0.16 1.22 —
SD, standard deviation.
Positive values represent a preference for stationary digital breast tomosynthesis compared to two-dimensional mammography.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Table 4
Results of the Secondary Analysis Performed on the Preference Portion of the Reader Study
Grand Mean Estimate Standard Error Two-Sided P Value Shape/morphology 0.0598 0.1416 .6751 Microcalcifications −0.6718 0.1030 <.05 Margins 0.1586 0.1422 .2718
It was tested whether the mean preference was larger than zero using a linear mixed model with a random intercept effect and Wald test. Positive values represent a preference for stationary digital breast tomosynthesis compared to two-dimensional mammography.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Discussion
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Acknowledgments
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
References
1. Rafferty E.A., Park J.M., Philpotts L.E., et. al.: Assessing radiologist performance using combined digital mammography and breast tomosynthesis compared with digital mammography alone: results of a multicenter, multireader trial. Radiology 2013; 266: pp. 104-113.
2. Michell M., Iqbal A., Wasan R., et. al.: A comparison of the accuracy of film-screen mammography, full-field digital mammography, and digital breast tomosynthesis. Clinical Radiology 2012; 67: pp. 976-981.
3. Bernardi D., Ciatto S., Pellegrini M., et. al.: Prospective study of breast tomosynthesis as a triage to assessment in screening. Breast Cancer Research and Treatment 2012; 133: pp. 267-271.
4. Poplack S.P., Tosteson T.D., Kogel C.A., et. al.: Digital breast tomosynthesis: initial experience in 98 women with abnormal digital screening mammography. AJR American Journal of Roentgenology 2007; 189: pp. 616-623.
5. Bissonnette M., Hansroul M., Masson E., et. al.: Digital breast tomosynthesis using an amorphous selenium flat panel detector. Proc SPIE 2005; 5745: pp. 529-540.
6. Maidment A., Albert M., Thunberg S., et. al.: Evaluation of a photon-counting breast tomosynthesis imaging system. Proc SPIE 2005; 5745:
7. Ren B., Ruth C., Stein J., et. al.: Design and performance of the prototype full field breast tomosynthesis system with selenium based flat panel detector. Proc SPIE 2005; 5745: pp. 550-561.
8. Ren B., Ruth C., Wu T., et. al.: A new generation FFDM/tomosynthesis fusion system with selenium detector. Proc SPIE 2010; 7622: pp. 76220B.
9. Wu T., Stewart A., Stanton M., et. al.: Tomographic mammography using a limited number of low-dose cone-beam projection images. Med Phys 2003; 30: pp. 365.
10. Acciavatti R.J., Maidment A.D.: Optimization of continuous tube motion and step-and-shoot motion in digital breast tomosynthesis systems with patient motion. Proc SPIE 2012; 8313: pp. 1-12. 831306
11. Qian X., Tucker A., Gidcumb E., et. al.: High resolution stationary digital breast tomosynthesis using distributed carbon nanotube x-ray source array. Med Phys 2012; 39: pp. 2090.
12. Qian X., Rajaram R., Calderon-Colon X., et. al.: Design and characterization of a spatially distributed multibeam field emission x-ray source for stationary digital breast tomosynthesis. Med Phys 2009; 36: pp. 4389-4399.
13. Tucker A.W., Lu J., Zhou O.: Dependency of image quality on system configuration parameters in a stationary digital breast tomosynthesis system. Med Phys 2013; 40: pp. 031917. -10
14. Kuo J., Ringer P.A., Fallows S.G., et. al.: Dynamic reconstruction and rendering of 3D tomosynthesis images. Proc SPIE 2011; 7961: 796116