Rationale and Objectives
The aim of this study was to assess the effects of radiation dose reduction on the assessment of the tracheal lumen on expiratory multidetector computed tomographic (MDCT) images of pediatric patients referred for evaluation for tracheomalacia (TM).
Materials and Methods
The hospital information system was used to retrospectively identify 20 standard-dose and 20 reduced-dose paired inspiratory and expiratory MDCT studies performed for the evaluation of suspected TM in pediatric patients (aged ≤ 18 years). The reduced-dose technique used a 50% reduction of the tube current for the expiratory portion of the study compared to the standard-dose technique. Two experienced pediatric radiologists, who were blinded to the tube current of the study, reported their levels of confidence for measuring the tracheal lumen using a four-point scale ranging from zero (no confidence) to three (highest level of confidence). The difference in confidence level between the two groups of studies was analyzed using the Mann-Whitney U test. The percentage of radiation dose reduction using the reduced-dose technique in comparison to the standard-dose technique was estimated using anthropomorphic thorax phantoms. The presence or absence of TM (≥50% expiratory reduction in tracheal cross-sectional luminal area) on MDCT imaging was compared to bronchoscopic results for the subset of 32 patients who underwent both procedures.
Results
A high level of confidence was reported for measuring the tracheal lumen on MDCT imaging for both standard-dose (median, 3.0) and reduced-dose (median, 3.0) expiratory sequences ( P = .80). The total radiation dose of the paired inspiratory-expiratory computed tomographic (CT) exam was decreased by 23% with the reduced-dose technique. TM was diagnosed by CT imaging in seven patients who underwent standard-dose and six patients who underwent reduced-dose paired inspiratory and expiratory MDCT studies. CT results for the presence or absence of TM were concordant with the results of bronchoscopy in all 32 patients who underwent both procedures.
Conclusion
The radiation dose of paired inspiratory-expiratory CT imaging can be reduced by 23% while maintaining similar diagnostic confidence for assessment of the tracheal lumen compared to a standard-dose technique in pediatric patients. Thus, a reduced-dose technique is recommended for evaluating TM in children.
Tracheomalacia (TM), a condition characterized by excessive expiratory collapse due to weakening of the tracheal wall and supporting cartilage, is the most common congenital anomaly of the central airways and a cause of potentially significant morbidity . Recently, paired inspiratory and expiratory multidetector computed tomographic (MDCT) imaging has been shown to be highly accurate in diagnosing TM in both children and adults . However, a potential disadvantage of this technique is that dual-phase (ie, inspiratory and expiratory phases) computed tomographic (CT) imaging is associated with up to twice as much radiation exposure as a single-phase CT acquisition. Such exposure is particularly concerning for pediatric patients, who are more susceptible than adults to the potentially harmful effects of ionizing radiation .
A previous study in adult patients showed that tube current can be reduced for the expiratory phase of MDCT studies while maintaining a high level of confidence in assessing the tracheal lumen for TM . However, to our knowledge, there is no published information regarding the use of a reduced-dose MDCT technique for the evaluation of TM in children. Because pediatric CT parameters are already routinely adjusted by patient age or weight, as well as by the use of automated tube current modulation, it is uncertain whether further dose reduction is possible while maintaining diagnostic confidence. Therefore, the purpose of this study was to evaluate the influence of a reduced-dose technique on the confidence levels of radiologists in assessing the tracheal lumen on paired inspiratory and expiratory MDCT exams of pediatric patients with clinically suspected TM.
Materials and methods
Patient Population
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
MDCT Imaging Technique
Patient Preparation
Sedation and intubation
Get Radiology Tree app to read full this article<
Intravenous contrast material
Get Radiology Tree app to read full this article<
MDCT Technical Factors
Type of MDCT scanner
Get Radiology Tree app to read full this article<
MDCT parameters
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Table 1
Tube Voltage and Tube Current by Patient Weight
Weight (lb) Tube Voltage (kVp) Standard/Reduced Tube Current (mA) 10–19 80 60/30 20–39 90 70/35 40–59 100 80/40 60–79 100 100/50 80–99 120 120/60 100–150 120 140/70 >150 120 170/85
Table 2
Tube Voltage and Tube Current by Patient Age
Age (y) Tube Voltage (kVp) Standard/Reduced Tube Current (mA) Newborn to 1 80 60/30 1–3 100 80/40 3–6 120 80/40 >6 120 200/100
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
CT Image Review and Evaluation
CT Image Review
Get Radiology Tree app to read full this article<
CT Image Evaluation
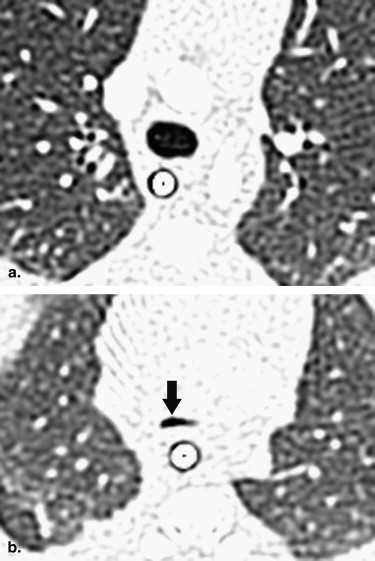
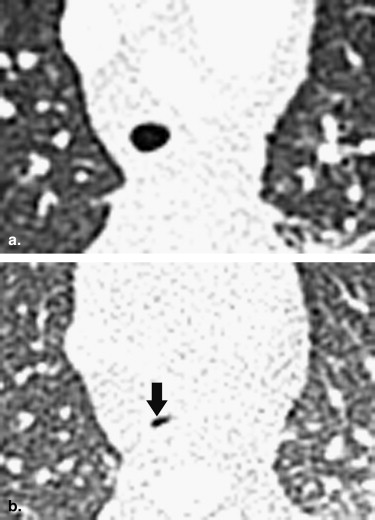
Quantitative measurement of tracheal luminal area
Get Radiology Tree app to read full this article<
Degree of confidence in measuring the tracheal luminal area
Get Radiology Tree app to read full this article<
Bronchoscopic Evaluation
Get Radiology Tree app to read full this article<
Radiation Dose
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Statistical Analysis
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Results
Get Radiology Tree app to read full this article<
Table 3
Patient Characteristics and Confidence Levels for Measurement of the Tracheal Lumen with Standard Versus Reduced Radiation Dose
Patient Characteristics Confidence Level Patient Age (mo) Gender Clinical Symptom Inspiration Expiration Standard radiation dose 1 1.5 M Stridor 3 3 2 52.3 F Stridor 3 3 3 141.6 M Cough 3 3 4 49.3 M Recurrent infection 3 3 5 5.8 M Stridor 3 3 6 6.5 M Cough 3 3 7 5.1 M Stridor 3 3 8 3.4 F Desaturation 3 3 9 5.4 M Desaturation 3 3 10 6.3 M Stridor 2 2 11 189.1 M Shortness of breath 3 3 12 15.3 M Stridor 2 3 13 73.1 F Recurrent infection 3 3 14 1.5 F Stridor 2 2 15 3.2 M Cough 2 3 16 3.9 M Stridor 2 2 17 7.9 M Recurrent infection 3 3 18 43.0 M Recurrent infection 3 3 19 0.9 M Stridor 3 3 20 4.4 M Stridor 3 3 Reduced radiation dose 1 2.5 M Cough 2 3 2 3.7 M Stridor 2 2 3 14.7 F Stridor 3 3 4 4.1 F Stridor 3 3 5 5.8 M Stridor 3 3 6 38.0 M Stridor 3 3 7 8.3 M Stridor 3 3 8 14.2 M Cough 3 3 9 50.8 M Cough 3 3 10 3.6 M Desaturation 3 3 11 143.7 M Cough 3 3 12 16.3 F Desaturation 3 3 13 6.9 F Stridor 3 3 14 2.0 F Desaturation 3 3 15 97.0 M Cough 2 2 16 45.2 M Stridor 3 3 17 58.0 F Recurrent infection 2 2 18 0.6 M Stridor 3 3 19 23.7 M Recurrent infection 3 3 20 25.5 M Shortness of breath 3 3
Get Radiology Tree app to read full this article<
Patient Characteristics
Get Radiology Tree app to read full this article<
MDCT Imaging Findings
Degree of Confidence in Measuring the Tracheal Luminal Area
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
CT Diagnosis of TM
Get Radiology Tree app to read full this article<
Comparison Between CT Imaging and Bronchoscopy
Get Radiology Tree app to read full this article<
Radiation Doses
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Discussion
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
References
1. Holinger L.D.: Etiology of stridor in the neonate, infant, and child. Ann Otol Rhinol Laryngol 1980; 89: pp. 397-400.
2. Paston F., Bye M.: Tracheomalacia. Pediatr Rev 1996; 17: pp. 328.
3. Wright C.D.: Tracheomalacia. Chest. Surg Clin N Am 2003; 13: pp. 349-357.
4. Carden K.A., Boiselle P.M., Waltz D.A., et. al.: Tracheomalacia and tracheobronchomalacia in children and adults: an in-depth review. Chest 2005; 127: pp. 984-1005.
5. Boiselle P.M., Feller-Kopman D., Ashiku S., et. al.: Tracheobronchomalacia: evolving role of dynamic multislice helical CT. Radiol Clin North Am 2003; 41: pp. 627-636.
6. Fraser R.S., Colman N., Muller N.L., et. al.: Upper airway obstruction.Fraser R.S.Colman N.Muller N.L.Pare P.D.Synopsis of diseases of the chest.2005.SaundersPhiladelphia:pp. 631-634.
7. Lee E.Y., Mason K.P., Zurakowski D., et. al.: MDCT assessment of tracheomalacia in symptomatic infants with mediastinal aortic vascular anomalies: preliminary technical experience. Pediatr Radiol 2008; 38: pp. 82-88.
8. Lee E.Y., Zurakowski D., Waltz D.A., et. al.: MDCT evaluation of the prevalence of tracheomalacia in children with mediastinal aortic vascular anomalies. J Thorac Imaging 2008; 23: pp. 258-265.
9. Lee E.Y., Litmanovich D., Boiselle P.M.: Multidetector CT evaluation of tracheomalacia. Radiol Clin North Am 2009; 47: pp. 261-269.
10. Baroni R.H., Ashiku S., Boiselle P.M.: Dynamic CT evaluation of the central airways in patients undergoing tracheoplasty for tracheobronchomalacia. AJR Am J Roentgenol 2005; 184: pp. 1444-1449.
11. Lee K.S., Sun M.R., Ernst A., et. al.: Comparison of dynamic expiratory CT with bronchoscopy for diagnosing airway malacia: a pilot evaluation. Chest 2007; 131: pp. 758-764.
12. Baroni R.H., Feller-Kopman D., Nishino M., et. al.: Tracheobronchomalacia: comparison between end-expiratory and dynamic expiratory CT for evaluation of central airway collapse. Radiology 2005; 235: pp. 635-641.
13. Ferretti G.R., Jankowski A., Perrin M.A., et. al.: Multi-detector CT evaluation in patients suspected of tracheobronchomalacia: comparison of end-expiratory with dynamic expiratory volumetric acquisitions. Eur J Radiol 2008; 68: pp. 340-346.
14. Frush D.P., Donnelly L.F., Rosen N.S.: Computed tomography and radiation risks: what pediatric health care providers should know. Pediatrics 2003; 112: pp. 951-957.
15. Brody A.S., Frush D.P., Huda W., et. al.: Radiation risk to children from computed tomography. Pediatrics 2007; 120: pp. 677-682.
16. Huda W.: Radiation doses and risks in chest computed tomography examinations. Proc Am Thorac Soc 2007; 4: pp. 316-320.
17. Zhang J., Hasegawa I., Feller-Kopman D., et. al.: 2003 AUR Memorial Award. Dynamic expiratory volumetric CT imaging of the central airways: comparison of standard-dose and low-dose techniques. Acad Radiol 2003; 10: pp. 719-724.
18. Boiselle P.M., Dippolito G., Copeland J., et. al.: Multiplanar and 3D imaging of the central airways: comparison of image quality and radiation dose of single-detector row CT and multi-detector row CT at differing tube currents in dogs. Radiology 2003; 228: pp. 107-111.
19. Lee E.Y., Boiselle P.M.: Tracheobronchomalacia in infants and children: multidetector CT evaluation. Radiology 2009; 252: pp. 7-22.
20. European Commission Study Group: European guidelines on quality criteria for computed tomography. Publication No EUR16262 EN.2000.Office for Official Publications of European CommunitiesBrussels, Belgium
21. Jessen K.A., Shrimpton P.C., Geleijns J., et. al.: Dosimetry for optimization of patient protection in computed tomography. Appl Radiat Isot 1999; 50: pp. 165-172.
22. Khursheed A., Hillier M.C., Shrimpton P.C., et. al.: Influence of patient age on normalized effective doses calculated for CT examination. Br J Radiol 2002; 75: pp. 819-830.
23. Petrie A., Sabin C.: Medical statistics at a glance.2nd ed2005.BlackwellMalden, MA 52–53
24. Browner W.S., Newman T.B., Cummings S.R., et. al.: Estimating sample size and power.Hulley S.B.Cummings S.R.Browner W.S.Grady D.Hearst N.Newman T.B.Designing clinical research.2001.Lippincott, Williams & WilkinsPhiladelphia:pp. 65-91. the nitty-gritty
25. Goo H.W., Suh D.S.: Tube current reduction in pediatric non-ECG-gated heart CT by combined tube current modulation. Pediatr Radiol 2006; 36: pp. 344-351.
26. Herzog C., Mulvihill D.M., Nguyen S.A., et. al.: Pediatric cardiovascular CT angiography: radiation dose reduction using automatic anatomic tube current modulation. AJR Am J Roentgenol 2008; 190: pp. 1232-1240.
27. Singh S., Kalra M.K., Moore M.A., et. al.: Dose reduction and compliance with pediatric CT protocols adapted to patient size, clinical indication, and number of prior studies. Radiology 2009; 252: pp. 200-208.