Simulation is a promising method for improving clinician performance, enhancing team training, increasing patient safety, and preventing errors. Training scenarios to enrich medical student and resident education, and apply toward competency assessment, recertification, and credentialing are important applications of simulation in radiology. This review will describe simulation training for procedural skills, interpretive and noninterpretive skills, team-based training and crisis management, professionalism and communication skills, as well as hybrid and in situ applications of simulation training. A brief overview of current simulation equipment and software and the barriers and strategies for implementation are described. Finally, methods of measuring competency and assessment are described, so that the interested reader can successfully implement simulation training into their practice.
Medical education has traditionally revolved around the apprenticeship model outlined by Flexner and Cameron , in which skills are learned under the tutelage of physician mentors and perfected by trainees through extensive hands-on experience in the hospital setting. However, there have been many changes in the way health care is delivered, reimbursed, and perceived by society ( Fig 1 ). Recent cost-containment and quality and safety mandates at the national and local levels challenge this model of medical education. A decrease in hospital length of stay, restrictions on resident work hours, and decreased resident autonomy have led to fewer opportunities for hands-on experience with patients. Work hour regulations, productivity pressures, and patients’ awareness of trainees “practicing” on them has led to a decline in training opportunities . These changes translate to a truncated training experience, fewer direct patient encounters, and fewer opportunities to perform procedures, which complicates traditional models of medical education. Simulation represents an attractive supplement to these traditional training methods in radiology.
Figure 1
Reasons for increased use of simulation-based training in medical education. (Color version of figure is available online.)
Simulation training allows trainees to practice a procedure or clinical scenario in a simulated environment before treating actual patients. These training modules use different scenarios and equipment and vary in realism.
Simulation is used in many nonmedical settings to teach crisis management skills to professionals such as pilots, military personnel, firefighters, and nuclear power plant workers . Currently, simulation is being expanded in the medical field to enhance clinical training. For example, medical schools use simulated patients to help teach communication and professionalism skills to students, allowing for constructive feedback in a safe environment and at the same time students gain experience. In fact, simulation-based learning in medical school is proving to be superior to problem-based learning for the acquisition of critical assessment and management skills . Medical specialties spanning from general practice to surgical subspecialties use high-fidelity simulation as a promising method for enhancing team training, increasing patient safety, preventing errors, and improving clinician performance .
Computer-based simulations are also being used for enhancing medical training and assessment, such as Advanced Cardiac Life Support recertification through the American Heart Association, which incorporates multiple comprehensive patient scenarios to determine competency in certification. Similar assessment with objective structured clinical examinations for medical students and residents are being used for board certification. Objective structured clinical examinations offer formalized review of necessary clinical skills, including interviewing patients, physical examinations, ordering and interpreting diagnostic tests, performing procedures, peer to peer communication, and patient handover. This kind of training assesses a clinician’s decision-making process with multiple scenarios to test competency and can be both formative if offered mid-course, providing an opportunity for improvement based on feedback, or summative, for a final grade.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
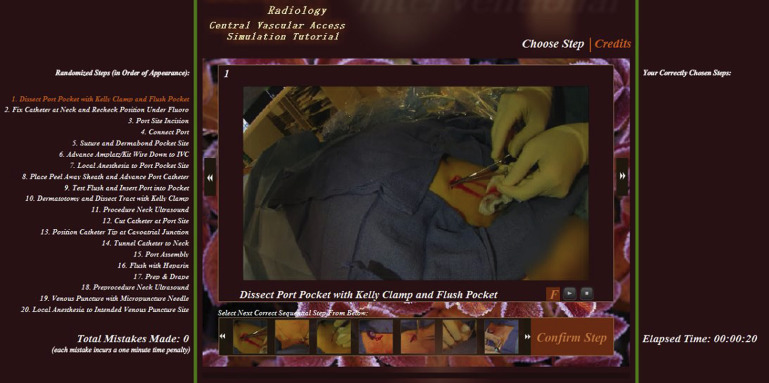
Figure 2
An example of a multifaceted radiology simulation scenario that incorporates procedural skill acquisition as well as professionalism and communication skills is shown. (Color version of figure is available online.)
Get Radiology Tree app to read full this article<
Simulation training of procedural skills in radiology
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Pediatrics
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Cross-Sectional Interventional Training of Percutaneous Image-Guided Procedures
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Vascular Interventional Training
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Neuroradiology
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Nuclear Medicine
Get Radiology Tree app to read full this article<
Thoracic Radiology
Get Radiology Tree app to read full this article<
Simulation training of nonprocedural skills in radiology
Get Radiology Tree app to read full this article<
Interpretive Skills
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Team-Based Training and Crisis Management: Contrast Reactions, Sedation Management
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Professionalism and Communication
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Hybrid Simulation
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
In Situ Simulation
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Current simulation equipment and software
Get Radiology Tree app to read full this article<
Part-task Trainers
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Computer-enhanced Mannequins
Get Radiology Tree app to read full this article<
Virtual Reality Simulators
Get Radiology Tree app to read full this article<
PACS Simulators
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Assessment methods and measuring competency
Assessment Methods
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Psychometric Tools for Interpersonal/Communications Skills
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Checklists for Procedural Skills
Get Radiology Tree app to read full this article<
Pretests and Posttests for Knowledge
Get Radiology Tree app to read full this article<
Measuring Competency
Get Radiology Tree app to read full this article<
Observational Assessment Tools
Get Radiology Tree app to read full this article<
Nonobservational Tools
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Barriers and Strategies for Implementation
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Access
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Cost
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Instructor Availability
Get Radiology Tree app to read full this article<
Educational Validity
Get Radiology Tree app to read full this article<
Assessment and Outcome Measurement
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Future Directions
Get Radiology Tree app to read full this article<
Improvements in Simulation Methods
Get Radiology Tree app to read full this article<
Simulation in Medical Curricula, Professional Credentialing, and Recertification Examinations
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Conclusions
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Acknowledgments
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
References
1. Flexner A.: Medical education in the United States and Canada: a report to the Carnegie Foundation for the Advancement of Teaching.1910.Carnegie Foundation for the Advancement of TeachingNew York City
2. Cameron J.L.: William Stewart Halsted. Our surgical heritage. Ann surgery 1997; 225: pp. 445-458.
3. Dawson S.: Procedural simulation: a primer. Radiology 2006; 241: pp. 17-25.
4. Okuda Y., Bryson E., DeMaria S., et. al.: The utility of simulation in medical education: what is the evidence?. Mt Sinai J Med 2009; 76: pp. 330-343.
5. Gaba D.M., Maxwell M., DeAnda A.: Anesthetic mishaps: breaking the chain of accident evolution. Anesthesiology 1987; 66: pp. 670-676.
6. Helmreich R.L., Chidester T., Gregorich S.: How effective is cockpit resource management training. Flight Saf Dig 1990; 9: pp. 1-17.
7. Steadman R.H., Coates W., Huang Y., et. al.: Simulation-based training is superior to problem-based learning for the acquisition of critical assessment and management skills. Crit Care Med 2006; 34: pp. 151-157.
8. Rosen M.A., Salas E., Wilson K., et. al.: Measuring team performance in simulation-based training: adopting best practices for healthcare. Simul Healthc 2008; 3: pp. 33-41.
9. Shapiro M., Morey J., Small S., et. al.: Simulation based teamwork training for emergency department staff: does it improve clinical team performance when added to an existing didactic teamwork curriculum?. Qual Saf Health Care 2004; 13: pp. 417-421.
10. Small S.D., Wuerz R., Simon R., et. al.: Demonstration of high-fidelity simulation team training for emergency medicine. Acad Emerg Med 1999; 6: pp. 312-323.
11. Merién A., van de ven J., Mol B., et. al.: Multidisciplinary team training in a simulation setting for acute obstetric emergencies: a systematic review. Obstet Gynecol 2010; 115: pp. 1021-1031.
12. Wayne D.B., Didwania A., Feinglass J., et. al.: Simulation-based education improves quality of care during cardiac arrest team responses at an academic teaching hospital: a case-control study. Chest 2008; 133: pp. 56-61.
13. Robertson B., Schumacher L., Gosman G., et. al.: Simulation-based crisis team training for multidisciplinary obstetric providers. Simul Healthc 2009; 4: pp. 77-83.
14. Salas E., Wilson K., Burke C., et. al.: Using simulation-based training to improve patient safety: what does it take?. Jt Comm J Qual Patient Saf 2005; 31: pp. 363-371.
15. Shanks D., Wong R., Roberts J., et. al.: Use of simulator-based medical procedural curriculum: the learner’s perspectives. BMC Med Educ 2010; 10: pp. 77.
16. Ogden P.E., Cobbs L., Howell M., et. al.: Clinical simulation: importance to the internal medicine educational mission. Am J Med 2007; 120: pp. 820-824.
17. Millington S.J., Wong R., Kassen B., et. al.: Improving internal medicine residents’ performance, knowledge, and confidence in central venous catheterization using simulators. J Hosp Med 2009; 4: pp. 410-416.
18. Woo M.Y., Frank J., Lee A., et. al.: Effectiveness of a novel training program for emergency medicine residents in ultrasound-guided insertion of central venous catheters. CJEM 2009; 11: pp. 343-348.
19. Velmahos G.C., Toutouzas K., Sillin L., et. al.: Cognitive task analysis for teaching technical skills in an inanimate surgical skills laboratory. Am J Surg 2004; 187: pp. 114-119.
20. Kneebone R., Nestel D., Yadollahi F., et. al.: Assessing procedural skills in context: exploring the feasibility of an Integrated Procedural Performance Instrument (IPPI). Med Educ 2006; 40: pp. 1105-1114.
21. Barry Issenberg S., McGaghie W., Petrusa E., et. al.: Features and uses of high-fidelity medical simulations that lead to effective learning: a BEME systematic review. Med Teach 2005; 27: pp. 10-28.
22. Ericsson K.A., Krampe R.T., Tesch-Römer C.: The role of deliberate practice in the acquisition of expert performance. Psychol Rev 1993; 100: pp. 363.
23. Mendiratta-Lala M., Williams T., de Quadros N., et. al.: The use of a simulation center to improve resident proficiency in performing ultrasound-guided procedures. Acad Radiol 2010; 17: pp. 535-540.
24. Rowe R., Cohen R.A.: An evaluation of a virtual reality airway simulator. Anesth Analg 2002; 95: pp. 62-66.
25. Hassard M.K., McCurdy L., Williams J., et. al.: Training module to teach ultrasound-guided breast biopsy skills to residents improves accuracy. Can Assoc Radiol J 2003; 54: pp. 155-159.
26. Barsuk J.H., McGaghie W., Cohen E., et. al.: Use of simulation-based mastery learning to improve the quality of central venous catheter placement in a medical intensive care unit. J Hosp Med 2009; 4: pp. 397-403.
27. Ericsson K.A.: Deliberate practice and the acquisition and maintenance of expert performance in medicine and related domains. Acad Med 2004; 79: pp. S70-S81.
28. Robertson H.J., Paige J.T., Bok L.: Simulation in radiology.2012.Oxford University PressNew York, NY
29. Ahmed K., Keeling A., Fakhry M., et. al.: Role of virtual reality simulation in teaching and assessing technical skills in endovascular intervention. J Vasc Interv Radiol 2010; 21: pp. 55-66.
30. Seymour N.E., Gallagher A., Roman S., et. al.: Virtual reality training improves operating room performance: results of a randomized, double-blinded study. Ann Surg 2002; 236: pp. 458-463.
31. Matveevskii A.S., Gravenstein N.: Role of simulators, educational programs, and nontechnical skills in anesthesia resident selection, education, and competency assessment. J Crit Care 2008; 23: pp. 167-172.
32. Korndorffer J.R., Dunne J., Sierra R., et. al.: Simulator training for laparoscopic suturing using performance goals translates to the operating room. J Am Coll Surg 2005; 201: pp. 23-29.
33. Sedlack R.E., Kolars J.C.: Computer simulator training enhances the competency of gastroenterology fellows at colonoscopy: results of a pilot study. Am J Gastroenterol 2004; 99: pp. 33-37.
34. Bakker N.H., Tanase D., Reekers J., et. al.: Evaluation of vascular and interventional procedures with time–action analysis: a pilot study. J Vasc Interv Radiol 2002; 13: pp. 483-488.
35. Stein-Wexler R., Sanchez T., Roper G., et. al.: An interactive teaching device simulating intussusception reduction. Pediatr Radiol 2010; 40: pp. 1810-1815.
36. Gaca A.M., Frush D., Hohenhaus S., et. al.: Enhancing pediatric safety: using simulation to assess radiology resident preparedness for anaphylaxis from intravenous contrast media. Radiology 2007; 245: pp. 236-244.
37. Lerner C., Gaca A., Frush D., et. al.: Enhancing pediatric safety: assessing and improving resident competency in life-threatening events with a computer-based interactive resuscitation tool. Pediatr Radiol 2009; 39: pp. 703-709.
38. Magee D., Zhu Y., Ratnalingam R., et. al.: An augmented reality simulator for ultrasound guided needle placement training. Med Biol Eng Comput 2007; 45: pp. 957-967.
39. Andreatta P., Chen Y., Marsh M., et. al.: Simulation-based training improves applied clinical placement of ultrasound-guided PICCs. Support Care Cancer 2011; 19: pp. 539-543.
40. Mendiratta-Lala M., Williams T., Mendiratta V., et. al.: Simulation center training as a means to improve resident performance in percutaneous noncontinuous ct-guided fluoroscopic procedures with dose reduction. AJR Am J Roentgenol 2015; 204: pp. W376-W383.
41. Sarwani N., Tappouni R., Flemming D.: Use of a simulation laboratory to train radiology residents in the management of acute radiologic emergencies. AJR Am J Roentgenol 2012; 199: pp. 244-251.
42. Chaer R.A., DeRubertis B., Lin S., et. al.: Simulation improves resident performance in catheter-based intervention: results of a randomized, controlled study. Ann Surg 2006; 244: pp. 343-352.
43. Kerber C., Flaherty L.: A teaching and research simulator for therapeutic embolization. AJNR Am J Neuroradiol 1980; 1: pp. 167-169.
44. Anderson J.H., Raghavan R.: A vascular catheterization simulator for training and treatment planning. J Digit Imaging 1998; 11: pp. 120-123.
45. Hahn J.K., Kaufman R., Winick A., et. al.: Training environment for inferior vena caval filter placement. Stud Health Technol Inform 1998; 50: pp. 291-297.
46. Luboz V., Zhang Y., Johnson S., et. al.: ImaGiNe Seldinger: first simulator for Seldinger technique and angiography training. Comput Methods Programs Biomed 2013; 111: pp. 419-434.
47. Chong C., How R., Black R., et. al.: Development of a simulator for endovascular repair of abdominal aortic aneurysms. Ann Biomed Eng 1998; 26: pp. 798-802.
48. Lonn L., Edmond J., Marco J., et. al.: Virtual reality simulation training in a high-fidelity procedure suite: operator appraisal. J Vasc Interv Radiol 2012; 23: pp. 1361-1366.e2.
49. Dawson D.L., Meyer J., Lee E., et. al.: Training with simulation improves residents’ endovascular procedure skills. J Vasc Surg 2007; 45: pp. 149-154.
50. Klass D., Tam M., Cockburn J., et. al.: Training on a vascular interventional simulator: an observational study. Eur Radiol 2008; 18: pp. 2874-2878.
51. Dankelman J., Wentink M., Grimbergen C., et. al.: Does virtual reality training make sense in interventional radiology? Training skill-, rule-and knowledge-based behavior. Cardiovasc Interv Radiol 2004; 27: pp. 417-421.
52. Gould D., Kessel D., Healey A., et. al.: Simulators in catheter-based interventional radiology: training or computer games?. Clin Radiol 2006; 61: pp. 556-561.
53. Gould D.: Training on simulators: limitations and relevance. Eur J Vasc Endovasc Surg 2007; 33: pp. 533-535.
54. Kaye A.D., K. V., Hymel B.J.: Simulation in spinal pain management.Simulation in radiology.2012.Oxford University PressNew York, NY:pp. 180.
55. Abdala N., Oliveira R., Junior A., et. al.: Manikin-type training simulator model for transpedicular puncture in percutaneous vertebroplasty. Radiol Bras 2007; 40: pp. 231-234.
56. Ferreira F., Peixoto J., Maciel M., et. al.: Development of a simulator with thyroid nodules for nuclear medicine. Sci Plena 2009; 5:
57. Mosman E.A., Peterson L., Hung J., et. al.: Practical methods for reducing radioactive contamination incidents in the nuclear cardiology laboratory. J Nucl Med Technol 1999; 27: pp. 287-289.
58. Keshtgar M., Chicken D., Waddington W., et. al.: A training simulator for sentinel node biopsy in breast cancer: a new standard. Eur J Surg Oncol 2005; 31: pp. 134-140.
59. Groen J., Van der Vleuten P., Greuter M., et. al.: Comparison of MRI, 64-slice MDCT and DSCT in assessing functional cardiac parameters of a moving heart phantom. Eur Radiol 2009; 19: pp. 577-583.
60. Towbin A.J., Paterson B.E., Chang P.J.: Computer-based simulator for radiology: an educational tool. Radiographics 2008; 28: pp. 309-316.
61. Ganguli S., Pedrosa I., Yam C., et. al.: Part I: preparing first-year radiology residents and assessing their readiness for on-call responsibilities. Acad Radiol 2006; 13: pp. 764-769.
62. Rojas C.A., Jawad H., Chung J.H.: The new era of radiology teaching files. AJR Am J Roentgenol 2012; 198: pp. 773-776.
63. Wiggins R.H., Davidson H., Harnsberger H., et. al.: Image file formats: past, present, and future. Radiographics 2001; 21: pp. 789-798.
64. Schlorhaufer C., Behrends M., Diekhaus G., et. al.: Implementation of a web-based, interactive polytrauma tutorial in computed tomography for radiology residents: how we do it. Eur J Radiol 2012; 81: pp. 3942-3946.
65. Tran T.H.D., Roach N., O’Kane P., et. al.: Creating a digital radiographic teaching file and database using a PC and common software. AJR Am J Roentgenol 2000; 175: pp. 325-327.
66. Talanow R.: Radiology teacher: a free, internet-based radiology teaching file server. J Am Coll Radiol 2009; 6: pp. 871-875.
67. Williams J., Sato T.S., Policeni B.: Pulmonary embolism teaching file: a simple pilot study for rapidly increasing pulmonary embolism recognition among new residents using interactive cross-sectional imaging. Acad Radiol 2013; 20: pp. 1048-1051.
68. Monsky W.L., Levine D., Mehta T., et. al.: Using a sonographic simulator to assess residents before overnight call. AJR Am J Roentgenol 2002; 178: pp. 35-39.
69. Becker G.J.: Simulation and the coming transformation of medical education and training. Radiology 2007; 245: pp. 7-9.
70. Wang C.L., Schopp J., Kani K., et. al.: Prospective randomized study of contrast reaction management curricula: computer-based interactive simulation versus high-fidelity hands-on simulation. Eur J Radiol 2013; 82: pp. 2247-2252.
71. Petscavage J.M., Paladin A., Wang C., et. al.: Current status of residency training of allergic-like adverse events to contrast media. Acad Radiol 2012; 19: pp. 252-255.
72. May W., Park J.H., Lee J.P.: A ten-year review of the literature on the use of standardized patients in teaching and learning: 1996-2005. Med Teach 2009; 31: pp. 487-492.
73. Medina L.S., Racadio J.M., Schwid H.A.: Computers in radiology. The sedation, analgesia, and contrast media computerized simulator: a new approach to train and evaluate radiologists’ responses to critical incidents. Pediatr Radiol 2000; 30: pp. 299-305.
74. Shavit I., Keidan I., Hoffmann Y., et. al.: Enhancing patient safety during pediatric sedation: the impact of simulation-based training of nonanesthesiologists. Arch Pediatr Adolesc Med 2007; 161: pp. 740-743.
75. February 2, 2015. Available at: http://acgme.org/acgmeweb/Portals/0/PDFs/Milestones/DiagnosticRadiologyMilestones.pdf
76. Ju M., Berman A., Hwang W., et. al.: Assessing interpersonal and communication skills in radiation oncology residents: a Pilot Standardized Patient Program. Int J Radiat Oncol Biol Phys 2014; 88: pp. 1129-1135.
77. Sasson J.P., Zand T., Lown B.A.: Communication in the diagnostic mammography suite: implications for practice and training. Acad Radiol 2008; 15: pp. 417-424.
78. Adler D.D., Riba M.B., Eggly S.: Breaking bad news in the breast imaging setting. Acad Radiol 2009; 16: pp. 130-135.
79. Harvey J.A., Cohen M., Brenin D., et. al.: Breaking bad news: a primer for radiologists in breast imaging. J Am Coll Radiol 2007; 4: pp. 800-808.
80. Brem R.F., Sanchez J.L., Rapelyea J.A.: Breaking bad news in breast imaging: a critical component of patient care. Acad Radiol 2009; 16: pp. 121-122.
81. Hammond I., Franche R., Black D., et. al.: The radiologist and the patient: breaking bad news. Can Assoc Radiol J 1999; 50: pp. 233-234.
82. Fallowfield L., Jenkins V., Farewell V., et. al.: Efficacy of a Cancer Research UK communication skills training model for oncologists: a randomised controlled trial. Lancet 2002; 359: pp. 650-656.
83. Jenkins V., Fallowfield L.: Can communication skills training alter physicians’ beliefs and behavior in clinics?. J Clin Oncol 2002; 20: pp. 765-769.
84. Fallowfield L., Jenkins V., Farewell V., et. al.: Enduring impact of communication skills training: results of a 12-month follow-up. Br J Cancer 2003; 89: pp. 1445-1449.
85. December 9, 2014. Available at: https://www.acgme.org/acgmeweb/tabid/148/ProgramandInstitutionalAccreditation/Hospital-BasedSpecialties/DiagnosticRadiology.aspx
86. Brydges R., Carnahan H., Rose D., et. al.: Coordinating progressive levels of simulation fidelity to maximize educational benefit. Acad Med 2010; 85: pp. 806-812.
87. Kneebone R., Kidd J., Nestel D., et. al.: An innovative model for teaching and learning clinical procedures. Med Educ 2002; 36: pp. 628-634.
88. Patterson MD, Blike GT, Nadkarni VM. In situ simulation: challenges and results. In: Henriksen K, Battles JB, Keyes MA, et al., eds. Advances in patient safety: new directions and alternative approaches. Vol. 3: Performance and Tools. Rockville, MD: Agency for Healthcare Research and Quality, US; 2008.
89. CAE Healthcare. HPS human patient simulator. Available at: http://www.caehealthcare.com/patient-simulators/hps-human-patient-simulator . Accessed July 31, 2015.
90. Holmboe E.S., Hawkins R.E.: Practical guide to the evaluation of clinical competence.2008.Mosby/Elsevier PhiladelphiaPA
91. Mentice. Available at: http://www.mentice.com/simulators-and-procedures#simulators . Accessed July 31, 2015.
92. Towbin A.J., Paterson B., Chang P.J.: A computer-based radiology simulator as a learning tool to help prepare first-year residents for being on call. Acad Radiol 2007; 14: pp. 1271-1283.
93. Ganguli S., Camacho M., Yam C., et. al.: Preparing first-year radiology residents and assessing their readiness for on-call responsibilities: results over 5 years. AJR Am J Roentgenol 2009; 192: pp. 539-544.
94. Glavin R.J., Gaba D.M.: Challenges and opportunities in simulation and assessment. Simul Healthc 2008; 3: pp. 69-71.
95. Matos F.M., Raemer D.B.: Mixed-realism simulation of adverse event disclosure: an educational methodology and assessment instrument. Simul Healthc 2013; 8: pp. 84-90.
96. Wood J., Collins J., Burnside E., et. al.: Patient, faculty, and self-assessment of radiology resident performance: a 360-degree method of measuring professionalism and interpersonal/communication skills11 1Funded by a grant from the Association of Program Directors in Radiology. Acad Radiol 2004; 11: pp. 931-939.
97. Joyce B.L., Steenbergh T., Scher E.: Use of the Kalamazoo Essential Elements Communication Checklist (Adapted) in an institutional interpersonal and communication skills curriculum. J Grad Med Educ 2010; 2: pp. 165-169.
98. Tubbs R.J., Murphy B., Mainiero M., et. al.: High-fidelity medical simulation as an assessment tool for radiology residents’ acute contrast reaction management skills. J Am Coll Radiol 2009; 6: pp. 582-587.
99. Glaiberman C.B., Jacobs B., Street M., et. al.: Simulation in training: one-year experience using an efficiency index to assess interventional radiology fellow training status. J Vasc Interv Radiol 2008; 19: pp. 1366-1371.
100. Berry M., Lystig T., Reznick R., et. al.: Assessment of a virtual interventional simulator trainer. J Endovasc Ther 2006; 13: pp. 237-243.
101. Iobst W.F., Sherbino J., Cate O., et. al.: Competency-based medical education in postgraduate medical education. Med Teach 2010; 32: pp. 651-656.
102. Warf B.C., Donnelly M., Schwartz R., et. al.: Interpreting the judgment of surgical faculty regarding resident competence. J Surg Res 1999; 86: pp. 29-35.
103. Reznick R., MacRae H.: Teaching surgical skills—changes in the wind. N Engl J Med 2006; 355: pp. 2664-2669.
104. Martin J., Regehr G., Reznick R., et. al.: Objective structured assessment of technical skill (OSATS) for surgical residents. Br J Surg 1997; 84: pp. 273-278.
105. Joice P., Hanna G., Cuschieri A.: Errors enacted during endoscopic surgery—a human reliability analysis. Appl Ergon 1998; 29: pp. 409-414.
106. Szalay D., Keeling A., Fakhry M., et. al.: Using operative outcome to assess technical skill. Am J Surg 2000; 180: pp. 234-237.
107. Krupinski E.A., Patel B., Berger W., et. al.: Assessing radiology resident preparedness to manage IV contrast media reactions using simulation technology. Stud Health Technol Inform 2009; 142: pp. 139-141.
108. Sekhar A., Sun M.R., Siewert B.: A Tissue Phantom Model for training residents in ultrasound-guided liver biopsy. Acad Radiol 2014; 21: pp. 902-908.
109. Strickland C.D., Lowry P., Petersen B., et. al.: Introduction of a virtual workstation into radiology medical student education. AJR Am J Roentgenol 2015; 204: pp. W289-W292.
110. Petscavage J.M., Wang C., Schopp J., et. al.: Cost analysis and feasibility of high-fidelity simulation based radiology contrast reaction curriculum. Acad Radiol 2011; 18: pp. 107-112.
111. Schmidt E., Goldhaber-Fiebert S., Ho L., et. al.: Simulation exercises as a patient safety strategy: a systematic review. Ann Intern Med 2013; 158: pp. 426-432.
112. Boet S., Bould M., Sharma B., et. al.: Within-team debriefing versus instructor-led debriefing for simulation-based education: a randomized controlled trial. Ann Surg 2013; 258: pp. 53-58.
113. Gould D., Patel A., Becker G., et. al.: SIR/RSNA/CIRSE joint medical simulation task force strategic plan: executive summary. Cardiovasc Interv Radiol 2007; 30: pp. 551-554.
114. Desser T.S.: Simulation-based training: the next revolution in radiology education?. J Am Coll Radiol 2007; 4: pp. 816-824.
115. Patel A.A., Glaiberman C., Gould D.A.: Procedural simulation. Anesthesiol Clin 2007; 25: pp. 349-359.