Rationale and Objectives
To evaluate the relationship between intramammary arterial calcifications detected by screening mammography and concomitant coronary artery disease, detected by coronary angiography.
Materials and Methods
We retrospectively evaluated screening mammography and coronary angiography results of 131 consecutive patients, ages 42–81 years. Risk factors for coronary artery disease (hypertension, diabetes mellitus, dyslipidemia, smoking, and obesity) were obtained from medical records to identify possible simultaneous risk factors for coronary artery disease.
Results
Eighty-five women had coronary artery disease (41 with intramammary arterial calcifications and 44 without such calcifications) and 46 had normal coronary angiography (11 had intramammary arterial calcifications and 35 did not). A strong association between intramammary arterial calcifications and coronary artery disease was seen, with an OR of 2.96 and P = .006 in the raw model and OR of 4.6 in the adjusted one. The evaluated risk factors did not present as confounding variables. Most patients had only two risk factors or less. The most prevalent risk factor for coronary artery disease was hypertension, with significantly higher prevalence in the coronary artery disease group ( P < .01).
Conclusion
A strong association exists between intramammary arterial calcifications and coronary artery disease. Therefore a mammographic finding of intramammary arterial calcification should receive more of the radiologists’ attention and its presence should never be omitted from the final report.
Coronary artery disease (CAD) and cancer are the leading causes of female death ( ). Mammography is employed as a breast cancer screening method in the United States and several other Western countries in women older than 40 years of age ( ). Intramammary arterial calcifications (IMAC) detected in mammograms are frequently not included in final reports because this considered a benign finding that is not relevant to the diagnosis of breast cancer ( ). In the last 20 years, studies have correlated IMAC to risk factors for cardiovascular disease (CVD), therefore suggesting an indirect relationship between IMAC and CVD ( ). IMAC was also associated with increased CVD mortality ( ). The purpose of this study is to verify whether IMAC may represent a predictor of underlying CAD, using coronary angiography as a gold standard.
Materials and methods
A total of 131 consecutive female patients ages 42–81 years (mean, 61 years) who underwent coronary angiography between October 2001 and April 2005 and also underwent mammography within 1 year of the coronary angiography were included in the study. All patients were admitted to one institution and received coronary angiography for suspected heart disease, mostly ischemic heart disease. This study was approved by the Institutional Review Board, and informed consent was waived because of the study’s retrospective design. Patient confidentiality was preserved following institutional and national regulations. After retrieval of angiography and mammography reports, patients were divided into group A (abnormal coronary angiography) and B (normal angiography). Group A was subdivided into patients with mild, moderate, and severe CAD.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Results
Patient Features and Risk Factors for CAD
Get Radiology Tree app to read full this article<
Table 1
Clinical Profile of Patients who had Coronary Angiography
Risk Factors Total ( n = 131) Group A ( n = 85) Group B ( n = 46) Age 61.1 ± 9.08 61.9 ± 9.08 59.7 ± 8.99 NS Hypertension 116 80 (94.1%) 36 (78.2%)P < .01 Diabetes mellitus 38 29 (34.1%) 9 (19.5%)P = .07 Dyslipidemia 88 61 (71.7%) 27 (58.6%) NS Smoking 19 13 (15.2%) 6 (13.0%) NS Obesity 29 16 (18.8%) 13 (28.2%) NS Intramammary arterial calcifications 52 41 (48.2%) 11 (23.9%)P < .01
NS: not significant.
Group A: women with coronary artery disease.
Group B: women without coronary artery disease.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
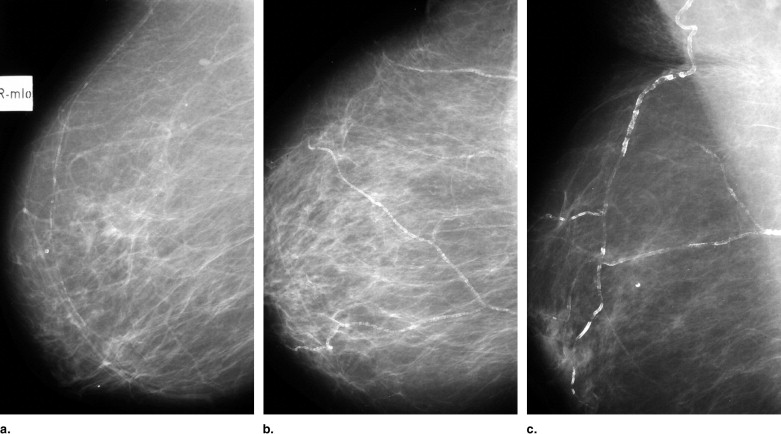
Mammography Results
Get Radiology Tree app to read full this article<
Table 2
Mammography Results
Coronary Artery Disease Intramammary Arterial Calcifications Present Absent Total Present 41 44 85 Absent 11 35 46 Total 52 79 131
P = .006
OR = 2.96 CI 95% (1.25–7.30)
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Table 3
Odds Ratio and Respective Confidence Interval (95%) for the Association Between IMAC and CAD
IMAC Absent OR ⁎ Present OR (CI 95%) ⁎ Model 1 † CAD 1.00 2.97 (1.33–6.60) Model 2 ‡ CAD 1.00 3.74 (1.50–9.30) Model 3 § CAD 1.00 4.02 (1.60–10.12) Model 4 ∥ CAD 1.00 4.60 (1.65–12.83)
CAD: coronary artery disease; IMAC: intramammary arterial calcifications.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Table 4
Prevalence of Risk Factors in Women With and Without IMAC
Risk factors Total ( n = 131) IMAC+ ( n = 52) IMAC– ( n = 79) Hypertension 116 46 (88.4%) 70 (88.6%) NS DM 36 18 (34.6%) 20 (25.3%) NS Dyslipidemia 88 32 (61.5%) 56 (70.8%) NS Smoking 19 1 (1.92%) 18 (22.7%)P < .001 Obesity 29 7 (13.4%) 22 (27.8%)P = .05 CAD 85 41 (78.8%) 44 (55.7%)P < .01
IMAC: intramammary arterial calcifications; DM: diabetes mellitus; CAD: coronary artery disease.
Get Radiology Tree app to read full this article<
Coronary Angiography Results
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
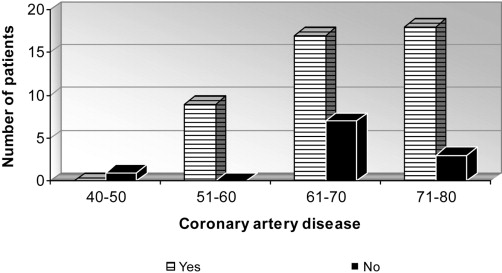
Table 5
Patient Distribution by Age
Age range IMAC Total Present Absent CAD+ CAD– CAD+ CAD– 40–50 y 0 1 10 (59%) 7 18 51–60 y 9 (100%) 0 19 (56%) 15 43 61–70 y 17 (71%) 7 15 (55%) 12 51 71–80 y 15 (83%) 3 0 1 19 Total 41 11 44 35 131
IMAC: intramammary arterial calcifications; DM: diabetes mellitus; CAD: coronary artery disease.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
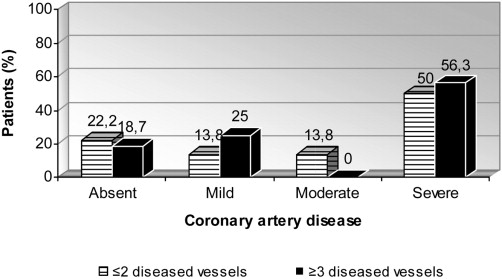
Table 6
Comparison Between IMAC Intensity and CAD Severity
CAD IMAC Absent Mild Moderate Intense Total Absent 35 4 6 1 46 Mild 10 3 5 1 19 Moderate 4 1 4 — 9 Severe 30 18 7 2 57 Total 79 26 22 4 131
IMAC: intramammary arterial calcifications; DM: diabetes mellitus; CAD: coronary artery disease.
Get Radiology Tree app to read full this article<
Discussion
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
References
1. American Heart Association: 2005.AHADallas, TX
2. Mosca L., Appel L.J., Benjamin E.J., et. al., American Heart Association; American College of Cardiology; American College of Nurse Practitioners; American College of Obstetricians and Gynecologists; American College of Physicians; American Medical Women’s Association; Association of Black Cardiologists; Centers for Disease Control and Prevention; National Heart, Lung and Blood Institute, National Institutes of Health; Office of Research on Women’s Health; Society of Thoracic Surgeons; World Heart Federation: Evidence-based guidelines for cardiovascular disease prevention in women. J Am Coll Cardiol 2004; 43: pp. 900-921.
3. Feig A.S., D’orsi C.J., Hendrick R.E., et. al.: American College of Radiology guidelines for breast cancer screening. Am J Roentgenol 1998; 171: pp. 29-33.
4. American College of Radiology (ACR) Breast imaging data and report system (BI- RADS).1995.American College of RadiologyReston, Va:
5. Crystal P., Crystal E., Leor J., et. al.: Breast arterial calcium on routine mammography as a potential marker for increased risk of cardiovascular disease. Am J Cardiol 2000; 86: pp. 216-217.
6. van Noord P.A., Beijerinck D., Kemmeren J.M., et. al.: Mammograms may convey more than breast cancer risk: breast arterial calcification and arterio-sclerotic related diseases in women of the DOM cohort. Eur J Cancer Prev 1996; 5: pp. 483-487.
7. Iribarren C., Go A.S., Tolstykh I., et. al.: Breast vascular calcification and risk of coronary heart disease, stroke, and heart failure. J Womens Health (Larchmt) 2004; 13: pp. 381-392.
8. Kemmeren J.M., van Noord P.A., Beijerinck D., et. al.: Arterial calcification found on breast cancer screening mammograms and cardiovascular mortality in women: the DOM Project. Am J Epidemiol 1998; 147: pp. 333-341.
9. National Heart Lung and Blood Institute Coronary Artery Surgery Study: A multicenter comparison of the effects of randomized medical and surgical treatment of mildly symptomatic patients with coronary artery disease, and a registry of consecutive patients undergoing coronary angiography. Circulation 1981; 63: pp. I13-I17.
10. Sickles E.A.: Breast calcifications: mammographic evaluation. Radiology 1986; 160: pp. 289-293.
11. Leinster S.J., Whitehouse G.H.: Factors which influence the occurrence of vascular calcification in the breast. Br J Radiol 1987; 60: pp. 457-458.
12. Pecchi A., Rossi R., Coppi F., et. al.: Association of breast arterial calcifications detected by mammography and coronary artery calcifications quantified by multislice CT in a population of post-menopausal women. Radiol Med (Torino) 2003; 106: pp. 305-312.
13. Maas A.H., van der Schouw Y.T., Mali W.P., et. al.: Prevalence and determinants of breast arterial calcium in women at high risk of cardiovascular disease. Am J Cardiol 2004; 94: pp. 655-659.
14. Baum J.K., Comstock C.H., Joseph L.: Intramammary arterial calcifications associated with diabetes. Radiology 1980; 136: pp. 61-62.
15. Moshyedi A.C., Puthawala A.H., Kurland R.J., et. al.: Breast arterial calcification: association with coronary artery disease. Radiology 1995; 194: pp. 181-183.
16. Kemmeren J.M., Beijerinck D., van Noord P.A., et. al.: Breast arterial calcifications: association with diabetes mellitus and cardiovascular mortality. Radiology 1996; 201: pp. 75-78.
17. Sickles E.A., Galvin H.B.: Breast arterial calcification in association with diabetes mellitus: too weak a correlation to have clinical utility. Radiology 1985; 155: pp. 577-579.
18. Schmitt E.L., Threatt B.A.: Mammographic intra-arterial calcifications. J Can Assoc Radiol 1984; 35: pp. 14-16.
19. Schmitt E.L., Threatt B.A.: Relationship of mammographic intra-arterial calcifications and diabetes. South Med J 1984; 77: pp. 988-989.
20. Schmitt E.L., Norbeck J.M., Threatt B.: Incidence of mammary intra-arterial calcification: an age-matched control study. South Med J 1985; 78: pp. 1440-1442.
21. Henkin Y., Abu-Ful A., Shai I., et. al.: Lack of association between breast artery calcification seen on mammography and coronary artery disease on angiography. J Med Screen 2003; 10: pp. 139-142.
22. Maas A.H., van der Schouw Y.T., Beijerinck D., et. al.: Arterial calcifications seen on mammograms: cardiovascular risk factors, pregnancy, and lactation. Radiology 2006; 240: pp. 33-38.
23. Kataoka M., Warren R., Luben R., et. al.: How predictive is breast arterial calcification of cardiovascular disease and risk factors when found at screening mammography?. AJR Am J Roentgenol 2006; 187: pp. 73-80.