Rationale and Objectives
The cervical spine is a high-risk area for percutaneous biopsy compared to the thoracic and lumbar regions. Biopsy of the cervical spine is less commonly undertaken, and previously published series on diagnostic yield and safety of cervical spine biopsy have been limited to 12 patients or less. The purpose of our study is to further define the diagnostic yield of computed tomography (CT)-guided biopsy for bony lesions identified in the cervical spine, by combining data from two large tertiary care referral centers.
Methods
A retrospective review of an imaging database was performed to identify all percutaneous CT-guided biopsies of the cervical spine performed at two tertiary care hospitals from 2010 to 2015. Core biopsies were obtained whenever possible and supplemented with fine-needle aspiration in some cases. Histopathologic results of the biopsy were recorded, as were changes in subsequent management, need for repeat biopsy, and complications.
Results
Forty-three patients underwent CT-guided biopsy of the cervical spine. Sufficient tissue for histopathologic analysis was obtained in 41 out of 43 cases, for a yield of 95%. One case was false-negative and one was deemed insufficient by the pathologist for diagnostic purposes; in both of these cases, only a fine-needle aspiration was obtained. There were no immediate or delayed complications.
Conclusions
Percutaneous biopsy of the cervical spine is a safe and high-yield method of obtaining a tissue diagnosis when performed under image guidance with CT.
Background
The cervical spine is a relatively high-risk area of the spine to biopsy compared to the lumbar or thoracic regions. The cervical vertebral bodies are smaller, the spinal cord is more tightly packed in the cervical spinal canal compared to other levels, and there is less surrounding cerebrospinal fluid (CSF). The vertebral arteries travel in the C6 to C1 foramen transversaria, in proximity to the vertebral bodies. More anteriorly, other critical structures like the carotid arteries, esophagus, and cranial nerves can be found in the cervical region of the spine. Image guidance with computed tomography (CT) is usually performed for safe tissue sampling of bony lesions in the cervical spine.
Data on diagnostic yield and safety of cervical spine biopsies are sparse compared to other regions of the spine , and the sample sizes of the largest published studies consist of 12 patients or less. In 2004, Lis et al. studied the diagnostic yield of CT-guided spine biopsies in 410 lesions, of which nine were in the cervical spine (2% of the sample). They reported a yield of 100% for the nine cervical spine lesions sampled. A study performed 4 years later by Rimondi et al. in 10 cervical spine lesions reported an accuracy of 70%. The differences in yield may be owing to the small sample size of the cervical spine lesions. Brugieres and colleagues published a series on CT-guided cervical bone biopsy in 12 patients and reported recurrent laryngeal nerve dysfunction in three patients (25%) related to the biopsy, which resolved on follow-up . No permanent deficits or serious adverse events were reported.
Get Radiology Tree app to read full this article<
Methods
Patient Selection
Get Radiology Tree app to read full this article<
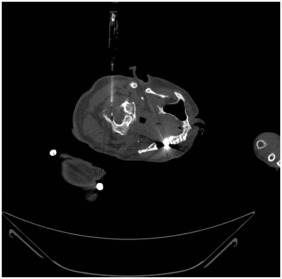
Technique
Get Radiology Tree app to read full this article<
Sample Preparation
Get Radiology Tree app to read full this article<
Results
Patient Characteristics
Get Radiology Tree app to read full this article<
Lesion Characteristics
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Table 1
Histopathologic Results of Cervical Spine Biopsy
Malignant ( n = 13 cases) Myeloma 6 Metastasis 5 Chondrosarcoma 1 Chordoma 1
Benign ( n = 30 cases) Normal 9 Infection 8 Reactive changes 6 Schwannoma 1 Eosinophilic granuloma 1 Hemangioblastoma 1 Bone cyst 1 Pseudomeningocele 1 False negative (proven osteomyelitis on open biopsy) 1 Inadequate sample 1
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Discussion
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Conclusion
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Acknowledgment
Get Radiology Tree app to read full this article<
References
1. Kattapuram S., Rosenthal D.: Percutaneous biopsy of the cervical spine using CT guidance. Am J Roentgen 1987; 149: pp. 539-541.
2. Rimondi E., Staals E., Errani C., et. al.: Percutaneous CT-guided biopsy of the spine: results of 430 biopsies. Eur Spine J 2008; 17: pp. 975-981.
3. Lis E., Bisky M., Pisinski L., et. al.: Percutaneous CT-guided biopsy of osseous lesion of the spine in patients with known or suspected malignancy. AJNR Am J Neuroradiol 2004; 25: pp. 1583-1588.
4. Brugieres P., Gaston A., Voisin M.C., et. al.: CT-guided percutaneous biopsy of the cervical spine: a series of 12 cases. Neuroradiology 1992; 34: pp. 358-360.
5. Deak P., Smal Y., Kalender W.: Multisection CT protocols: sex- and age-specific conversion factors used to determine effective dose from dose-length product. Radiology 2010; 257: pp. 158-166.
6. Hau M., Kim J., Kattapuram S., et. al.: Accuracy of CT-guided biopsy in 359 patients with musculoskeletal lesions. Skeletal Radiol 2002; 31: pp. 349-353.
7. Fraser-Hill M., Renfrew D., Hilsenrath P.: Percutaneous needle biopsy of musculoskeletal lesions. 2. Cost-effectiveness. Am J Roentgen 1992; 158: pp. 813-818.