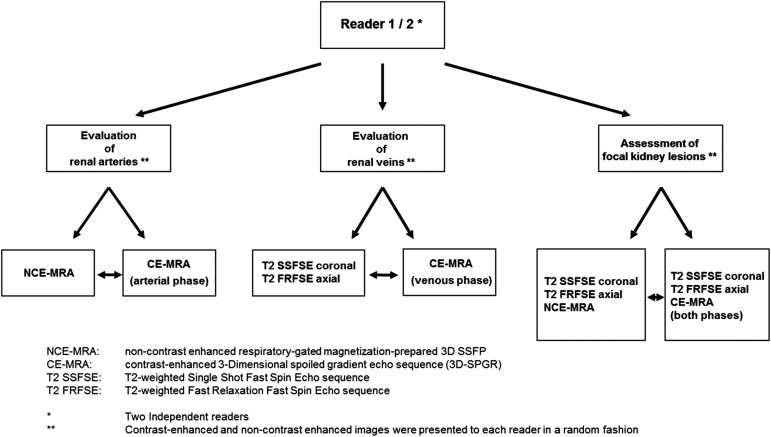
Rationale and Objectives
The objective of the study was to evaluate the performance of a non–contrast-enhanced magnetic resonance (MR) imaging protocol for preoperative screening of living related kidney donors.
Materials and Methods
Forty consecutive subjects (mean age 52.2 ± 11.3 years, range 29–73 years) underwent MR imaging with T2-weighted sequences (coronal and axial plane), with a non–contrast-enhanced respiratory-gated three-dimensional steady state free precession MR angiography (NCE-MRA) sequence and with contrast-enhanced magnetic resonance MR angiography (CE-MRA) sequences in the arterial and venous phases. Two blinded readers independently assessed arterial and venous anatomy and potential kidney lesions. Results of non–contrast-enhanced images were compared to CE-MRA and in a subgroup of 21 subjects to surgery as standard of reference.
Results
Regarding arterial anatomy, NCE-MRA yielded sensitivity, specificity, and accuracy of 100%, 89%, and 91% compared to CE-MRA. Three kidneys were found to have more accessory renal arteries at NCE-MRA than at CE-MRA. In the subgroup of 21 subjects, 1 surgically proven accessory artery was depicted with NCE-MRA but not with CE-MRA. Accuracy of T2-weighted images regarding accessory veins or variant venous course was 99%, with one missed circumaortic vein on T2-weighted images. Two simple cysts were missed on T2-weighted and NCE-MRA but not on CE-MRA images.
Conclusion
A non–contrast-enhanced MR imaging protocol including NCE-MRA and T2-weighted images allows for the accurate screening of living related kidney donors and may serve as an alternative to CE-MRA.
Renal transplantation is considered the therapy of choice for end-stage renal failure. Living related kidney donation offers a possibility to overcome the constant shortage of renal allografts. Compared with cadaveric grafts, grafts from living donors are associated with better long-term results, including longer graft survival .
Harvesting of donor kidneys via a laparoscopic approach has become the procedure of choice with the advantages of a lower overall complication rate, less postoperative pain, shorter hospital stay, and faster return to work compared to open donor nephrectomy . Before nephrectomy, the current guidelines recommend the assessment for potential donors including a complete clinical history, physical examination, laboratory testing, urine analysis, and imaging with a mandatory renal angiogram . In particular, laparoscopic harvesting procedures require accurate preoperative imaging, which should provide detailed information on the vascular road map and rule out the presence of focal or diffuse renal lesions and urinary tract dilatation.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Materials and methods
Get Radiology Tree app to read full this article<
Study Subjects
Get Radiology Tree app to read full this article<
Table 1
Demographics of Potential Living Related Kidney Donors
Study Population ( N = 40) Age (y) ∗ 52.2 ± 11.3 (29–73) Sex Men 15 Women 25 BMI (kg/m 2 ) ∗ 25.3 ± 3.0 (19.8–33.9) Creatinine clearance (mL/min) † 102 ± 22 (62–145) Obesity ‡ 3 Smoking § 5 Hypertension ¶ 11 Elevated serum cholesterol ∗∗ 7 Diabetes mellitus 2 Positive family history 1
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
MR Imaging
Get Radiology Tree app to read full this article<
Table 2
Detailed Overview of the Magnetic Resonance Imaging Protocol
Nr Sequence Contrast Agent ∗ Image Plane TR (ms) TE (ms) TI (ms) Flip Angle (°) Receiver Bandwith (kHz) NEX Slice Thickness (mm) Spacing (mm) Field of View (cm) Matrix 1 T2 SSFSE − Coronal 1132 92.4 – 90 ±62.5 0.54 4 1 46 × 41 384 × 224 2 T2 FRFSE − Axial 6316 85.3 – 90 ±50 2 4 1 36 × 36 256 × 160 3 NCE-MRA − Axial 4.5 2.3 200 90 ±125 0.79 2 −1 36 × 28 256 × 256 4 Test bolus + Sagittal 4.9 1.3 – 60 ±31.3 2 10 0 38 × 28 256 × 192 5 CE-MRA + Coronal 3.6 1.2 – 25 ±62.5 0.75 1.8 0 46 × 36 256 × 160
TR, repetition time in milliseconds; TE, echo time in milliseconds; TI, inversion time in milliseconds; NEX, number of excitations; T2 SSFSE, T2-weighted single shot fast spin echo sequence; T2 FRFSE, T2-weighted fast relaxation fast spin echo sequence; NCE-MRA, non–contrast-enhanced respiratory-gated magnetization-prepared three-dimensional SSFP (steady state free precession) with inversion recovery and fat saturation; Test bolus, spoiled gradient echo sequence (SPGR); CE-MRA, contrast-enhanced three-dimensional spoiled gradient echo sequence (3D-SPGR) acquisition in arterial and venous phase.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Image Analysis
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Surgical Report of Kidney Donors
Get Radiology Tree app to read full this article<
Statistical Analyses
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Results
Get Radiology Tree app to read full this article<
CE-MRA
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
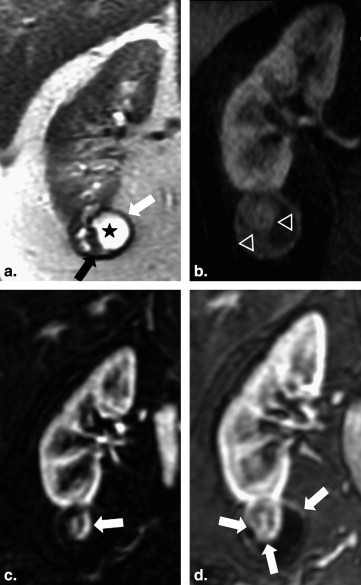
NCE-MRA and T2-weighted Images
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Surgery
Get Radiology Tree app to read full this article<
Performance of NCE-MRA for Vessel Anatomy Screening
Get Radiology Tree app to read full this article<
Table 3
Overview of the Performance of NCE-MRA for Vessel Anatomy Screening
Standard of Reference Test Sensitivity (95% CI) Specificity (95% CI) Accuracy (95% CI) Accessory renal arteries_n_ = 80 CE-MRA NCE-MRA 100% (82–100%) 89% (78–95%) 91% (82–96%)n = 21 Surgery CE-MRA 67% (9–99%) 100% (81–100%) 95% (76–100%)n = 21 Surgery NCE-MRA 100% (29–100%) 100% (81–100%) 100% (84–100%) Accessory renal veins_n_ = 80 CE-MRA T2 67% (9–99%) 100% (95–100%) 99% (93–100%) Variant renal veins_n_ = 80 CE-MRA T2 80% (28–99%) 100% (95–100%) 99% (93–100%)
CI, confidence interval; CE-MRA, contrast-enhanced magnetic resonance angiography; NCE-MRA, non–contrast-enhanced magnetic resonance angiography; T2, T2-weighted imaging.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
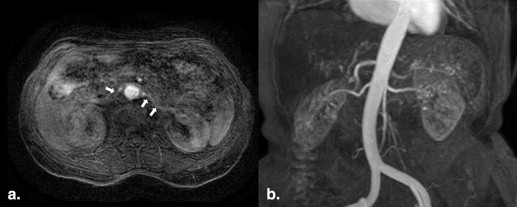
Assessment of Focal Kidney Lesions and Urinary Tract Obstruction
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Discussion
Get Radiology Tree app to read full this article<
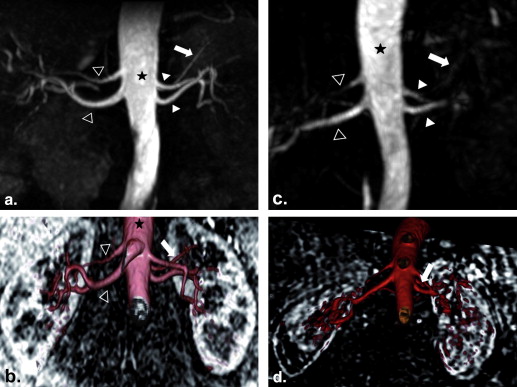
Assessment of Renal Arteries
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
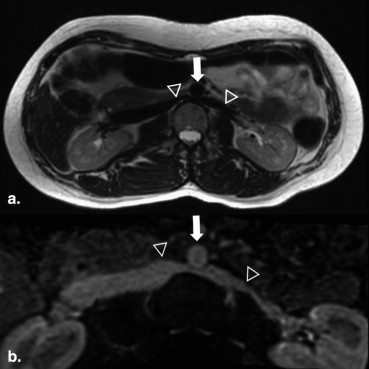
Assessment of Renal Veins
Get Radiology Tree app to read full this article<
Focal Kidney Lesions
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Limitations
Get Radiology Tree app to read full this article<
Conclusion
Get Radiology Tree app to read full this article<
References
1. Hariharan S., Johnson C.P., Bresnahan B.A., et. al.: Improved graft survival after renal transplantation in the United States, 1988 to 1996. N Engl J Med 2000; 342: pp. 605-612.
2. Nanidis T.G., Antcliffe D., Kokkinos C., et. al.: Laparoscopic versus open live donor nephrectomy in renal transplantation: a meta-analysis. Ann Surg 2008; 247: pp. 58-70.
3. Kalble T., Lucan M., Nicita G., et. al.: EAU guidelines on renal transplantation. Eur Urol 2005; 47: pp. 156-166.
4. Kuhlemann J., Blondin D., Grotemeyer D., et. al.: Gadofosveset-enhanced MR imaging for the preoperative evaluation of potential living kidney donors: correlation with intraoperative findings. Rofo 2010; 182: pp. 1001-1009.
5. Rankin S.C., Jan W., Koffman C.G.: Noninvasive imaging of living related kidney donors: evaluation with CT angiography and gadolinium-enhanced MR angiography. AJR Am J Roentgenol 2001; 177: pp. 349-355.
6. Liefeldt L., Kluner C., Glander P., et. al.: Non-invasive imaging of living kidney donors: intraindividual comparison of multislice computed tomography angiography with magnetic resonance angiography. Clin Transplant 2012; 26: pp. E412-E417.
7. Miyazaki M., Lee V.S.: Nonenhanced MR angiography. Radiology 2008; 248: pp. 20-43.
8. Glockner J.F., Takahashi N., Kawashima A., et. al.: Non-contrast renal artery MRA using an inflow inversion recovery steady state free precession technique (Inhance): comparison with 3D contrast-enhanced MRA. J Magn Reson Imaging 2010; 31: pp. 1411-1418.
9. Laurence I., Ariff B., Quest R.A., et. al.: Is there a role for free breathing non-contrast steady-state free precession renal MRA imaging for assessing live donors? A preliminary study. Br J Radiol 2012; 85: pp. e448-e454.
10. Khoo M.M., Deeab D., Gedroyc W.M., et. al.: Renal artery stenosis: comparative assessment by unenhanced renal artery MRA versus contrast-enhanced MRA. Eur Radiol 2011; 21: pp. 1470-1476.
11. Landis J.R., Koch G.G.: The measurement of observer agreement for categorical data. Biometrics 1977; 33: pp. 159-174.
12. Kok N.F., Dols L.F., Hunink M.G., et. al.: Complex vascular anatomy in live kidney donation: imaging and consequences for clinical outcome. Transplantation 2008; 85: pp. 1760-1765.
13. Nikken J.J., Krestin G.P.: MRI of the kidney: state of the art. Eur Radiol 2007; 17: pp. 2780-2793.
14. Andrews P.A., Burnapp L., Manas D., et. al.: Summary of the British Transplantation Society/Renal Association U.K. guidelines for living donor kidney transplantation. Transplantation 2012; 93: pp. 666-673.