Rationale and Objectives
In conventional projection radiography, cartilage and other soft tissues do not produce enough radiographic contrast to be distinguishable from each other. Diffraction-enhanced imaging (DEI) uses a monochromatic x-ray beam and a silicon crystal analyzer to produce images in which attenuation contrast is greatly enhanced and x-ray refraction at tissue boundaries can be detected. The aim of this study was to test the efficacy of conventional x-ray tube–based DEI for the detection of soft tissues in experimental samples.
Materials and Methods
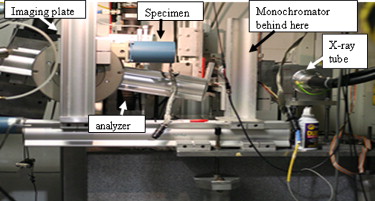
Cadaveric human tali (normal and degenerated) and a knee and thumb were imaged with DEI using a conventional x-ray tube and DEI setup that included a double–silicon crystal monochromator and a silicon crystal analyzer positioned between the imaged object and the detector.
Results
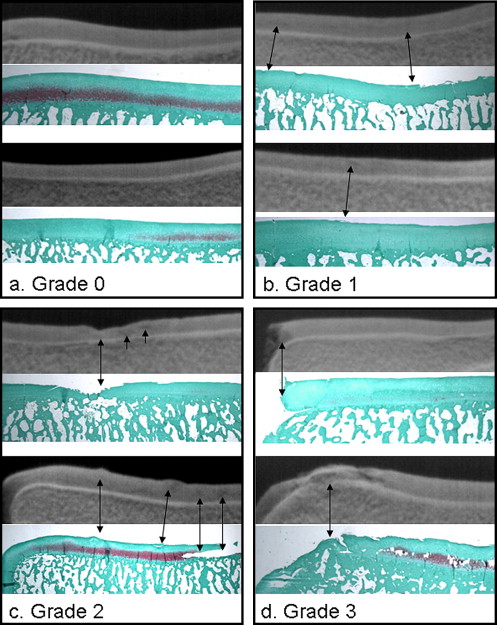
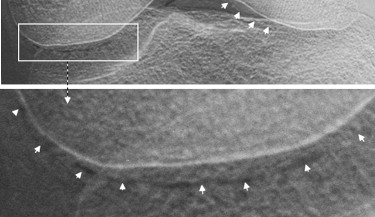
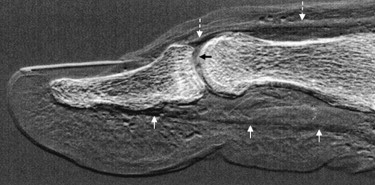
Diffraction-enhanced images of the cadaveric tali allowed the visualization of cartilage and its specific level of degeneration for each specimen. There was a significant correlation between the grade of cartilage integrity as assessed on the tube diffraction-enhanced images and on their respective histologic sections ( r = 0.97, P = .01). Images of the intact knee showed the articular cartilage edge of the femoral condyle, even when superimposed by the tibia. In the thumb image, it was possible to visualize articular cartilage, tendons, and other soft tissues.
Conclusion
DEI based on a conventional x-ray tube allows the visualization of skeletal and soft tissues simultaneously. Although more in-depth testing and optimization of the DEI setup must be carried out, these data demonstrate a proof of principle for further development of the technology for future clinical imaging.
Phase contrast imaging techniques are based on the use of information arising from the modification of the amplitude and phase of x-rays as they traverse an object. This allows for the detection of subject contrast due to tissue properties such as refraction. This contrast does not depend on x-ray attenuation, as is the case with contrast in conventional radiography. Thus, tissue contrast that is difficult to detect through x-ray attenuation, particularly at high energies, at which radiation dose is comparatively reduced, may be detected with phase contrast techniques. This includes soft tissues that do not have the composition to provide the necessary attenuation of x-rays and require techniques that exploit x-ray refraction at tissue boundaries to be visualized. One such technique is based on a system in which an analyzer crystal is positioned between the object and the detector. This allows only those x-rays satisfying the Bragg condition to be diffracted to the detector. Changes in x-ray reflection angle are converted to changes in x-ray intensity, through an intensity versus reflection angle curve (measured in microradians), described as the “rocking curve.” By altering the angle of the analyzer, it is possible to record different refraction angles and thus extract both refraction and absorption characteristics ( ).
What renders this technology pertinent to the study of joint disease is that soft tissues, including articular cartilage, menisci, tendons, and ligaments, are detected with reasonable clarity and contrast. Furthermore, it has been used to detect pathologic changes within these tissues, even at early stages of disease. The drawback has been that DEI has, until now, been used exclusively with synchrotron sources of x-rays, rendering it impractical for routine clinical use. This led to the development of a system that could use DEI technology but with a compact x-ray source, such as a commercially available tungsten tube (tube DEI).
Get Radiology Tree app to read full this article<
Materials and methods
Specimens
Get Radiology Tree app to read full this article<
Imaging Setup
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Imaging
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Histology
Get Radiology Tree app to read full this article<
Image Grading and Statistical Analysis
Get Radiology Tree app to read full this article<
Results
Tali
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Knee and Thumb
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Discussion
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
References
1. Chapman D., Thomlinson W., Johnston R.E., et. al.: Diffraction enhanced x-ray imaging. Phys Med Biol 1997; 42: pp. 2015-2025.
2. Muehleman C., Chapman L.D., Kuettner K.E., et. al.: Radiography of rabbit articular cartilage with diffraction enhanced imaging. Anat Rec A Discov Mol Cell Evol Biol 2003; 272: pp. 392-397.
3. Muehleman C., Majumdar S., Arfelli F., et. al.: Radiographic detection of structural orientation in articular cartilage. Osteoarthritis Cartilage 2004; 12: pp. 97-105.
4. Muehleman C., Li J., Wernick M., et. al.: Yes you can see cartilage with x-rays: diffraction enhanced imaging of cartilage and bone. J Musculoskelet Neuronal Interact 2004; 4: pp. 369-370.
5. Muehleman C., Li J., Zhong Z., et. al.: Multiple-image radiography human soft tissue. J Anat 2006; 208: pp. 115-124.
6. Muehleman C., Li J., Zhong Z.: Preliminary study on diffraction enhanced imaging for a canine model of cartilage damage. Osteoarthritis Cartilage 2006; 14: pp. 882-888.
7. Lewis R.A.: Medical phase contrast x-ray imaging: current status and future prospects. Phys Med Biol 2004; 49: pp. 3573-3583.
8. Mollenhauer J.A., Aurich M.E., Zhong A., et. al.: Diffraction enhanced x-ray imaging of articular cartilage. Osteoarthritis Cartilage 2002; 10: pp. 163-171.
9. Abreu M., Johnson K., Chung C.B., et. al.: Calcification in calcium pyrophosphate dihydrate (CPPD) crystalline deposits in the knee: anatomic, radiographic, MRI, and histologic study in cadavers. Skeletal Radiol 2004; 33: pp. 392-398.
10. Muehleman C., Bareither D., Huch K., et. al.: Prevalence of degenerative morphological changes in the joints of the lower extremity. Osteoarthritis Cartilage 1997; 5: pp. 23-37.
11. Parham CA, Zhong A, Connor D, Chapman D, Pisano ED. Design and implementation of a compact low-dose diffraction enhanced medical imaging system. Acad Radiol. In press.
12. Rosenberg L.: Chemical basis for the histologic use of Safranin O in the study of articular cartilage. J Bone Joint Surg Am 1971; 53: pp. 69-82.
13. Burstein D., Gray M.L.: Is MRI fulfilling its promise for molecular imaging of cartilage in arthritis?. Osteoarthritis Cartilage 2006; 14: pp. 1087-1090.
14. Li J., Williams J.M., Zhong Z., et. al.: Reliability of diffraction enhanced imaging for assessment of cartilage lesions, ex vivo. Osteoarthritis Cartilage 2005; 13: pp. 187-197.
15. Li J., Zhong Z., Lidtke R., et. al.: Radiography of soft tissue of the foot and ankle with diffraction enhanced imaging. J Anat 2003; 202: pp. 463-470.