Fibromyalgia (FM) is a chronic pain condition characterized by widespread pain and tenderness that afflicts 2%–4% of the population in industrialized countries ( ). It is the second most common rheumatologic disease after osteoarthritis. Although the underlying pathology, mediating the allodynia and hyperalgesia of FM remains poorly understood, a dysfunction in central neurobiologic structures is suspected. In addition to pain, FM patients often present with other syndromes such as irritable bowel syndrome, idiopathic low back pain, and temporomandibular disease syndrome, suggesting a common underlying pathology across these conditions ( ).
Although FM is defined by widespread tenderness, experimental data indicate that the enhanced pain sensitivity of FM is not limited to pressure stimuli alone. Individuals with FM also exhibit heightened pain sensitivity in response to multiple other stimuli, including heat, noise, and electricity ( ). These data, in conjunction with the finding that pain is not localized to a particular body region, suggest that this condition may be largely from the augmented central nervous system processing of pain.
The neurophysiology of pain processing has received increasing interest in recent years and data from different neuroimaging methods such as multiple positron emission tomography ( ), single photon emission computed tomography (SPECT) ( ), functional magnetic resonance imaging ( ), and more recently magnetic resonance (MR) spectroscopy consistently identify the brain structures that are activated during painful conditions in healthy controls ( ). These structures include the primary and secondary somatosensory cortices, the insula, the anterior cingulate, the thalamus, the dorsal lateral prefrontal cortex, and the basal ganglia ( ). Collectively, these regions have been termed the “pain matrix,” which is activated in response to painful stimulation. Interestingly, not all of the regions in the pain matrix serve the same functions in encoding pain ( ). Multiple studies have indicated that pain matrix exhibits abnormal activation patterns in FM, both at baseline and in response to painful stimuli ( ).
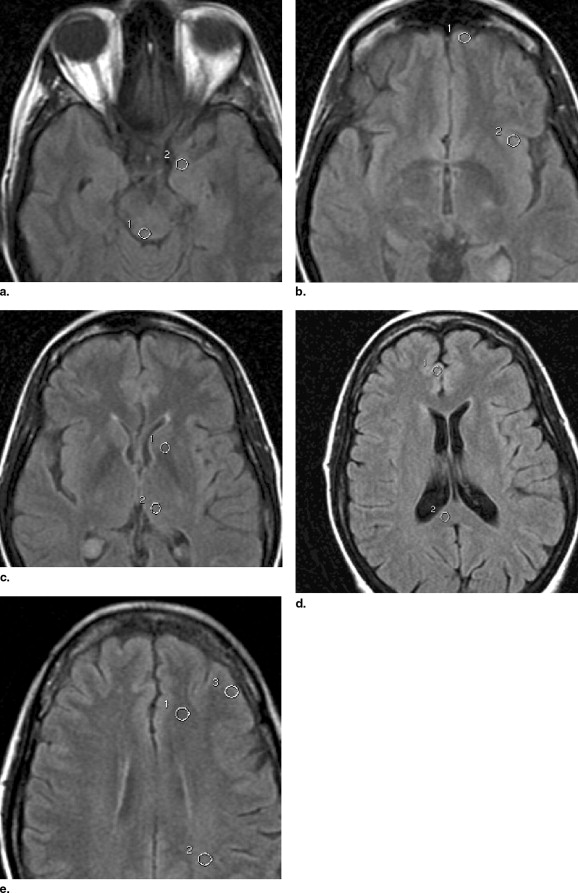
Diffusion-weighted imaging (DWI), which measures the diffusivity of water molecules, is a well-established MR imaging sequence commonly used in clinical practice to detection early ischemia ( ). Diffusion tensor imaging (DTI) yields quantitative measures for tissue water mobility as a function of the direction of water motion and is probed by application of diffusion-sensitization gradients in multiple directions ( ). Appropriate mathematical combination of the directional diffusion-weighted images provides quantitative measures of water diffusion for each voxel via the apparent diffusion coefficient (ADC), as well as the degree of diffusion directionality, or anisotropy ( ). DTI allows in vivo mapping of the anatomic connections in the human brain; previous studies have identified and confirmed the existence of an anatomic circuitry for the functionally characterized top-down influences on pain processing via brainstem structures in humans ( ).
Fractional anisotropy (FA) is a measure of the portion of the diffusion tensor from anisotropy.
The aim of the present study was to investigate whether DWI and DTI can depict cerebral abnormalities in fibromyalgia patients and if significant differences in measured ADC histograms between these patients and normal controls exist. We hypothesized that if there were differences between fibromyalgia patients and controls in any brain region, that these abnormalities should be most pronounced in individuals with more severe pain, a lower pain threshold, or cognitions that are known to be associated with a poor prognosis in pain patients.
Materials and methods
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Imaging
MR imaging
Get Radiology Tree app to read full this article<
DTI
Get Radiology Tree app to read full this article<
Imaging Postprocessing and Analysis
Conventional MR imaging
Get Radiology Tree app to read full this article<
DWI and whole-brain apparent diffusion coefficient histograms
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
DTI
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Pain Assessment
Clinical pain
Get Radiology Tree app to read full this article<
Experimental pain
Get Radiology Tree app to read full this article<
Questionnaires
Get Radiology Tree app to read full this article<
Statistical Analysis
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Results
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Table 1
ADC (Mean and SD) and FA (Mean, SD) and P Value in Right Thalamus in the Two Groups
FM Patients (19) HC (25)P Value ADC (mean [SD]) × 10 −6 mm 7.14 (0.30) 7.20 (0.28) NS FA (mean [SD]) 0.258 (0.022) 0.278 (0.035) .02
ADC: apparent diffusion coefficient; FA: fraction anisotropy; SD: standard deviation.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Table 2
Correlation of Clinical Outcomes With FA Values in Right Thalamus
Clinical Outcome R (correlation)P Value Tender point −0.47 NS VAS—clinical pain −0.50 <.05 Depression −0.23 NS Anxiety −0.07 NS BPCQ—powerful doctor −0.72 <.005 BPCQ—chance 0.36 NS BPCQ—internal 0.07 NS Pressure pain testing—low 0.12 NS Pressure pain testing—medium 0.14 NS Pressure pain testing—high 0.16 NS
FA: fraction anisotropy; VAS: visual analog scale; BPCQ: Beliefs about Pain Control Questionnaire.
Get Radiology Tree app to read full this article<
Discussion
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Acknowledgments
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
References
1. Wolfe F., Ross K., Anderson J., et. al.: The prevalence and characteristics of fibromyalgia in the general population. Arthr Rheum 1995; 38: pp. 19-28.
2. Clauw D.J., Chrousos G.P.: Chronic pain and fatigue syndromes: overlapping clinical and neuroendocrine features and potential pathogenic mechanisms. Neuroimmunomodulation 1997; 4: pp. 134-153.
3. Petzke F., Clauw D.J., Ambrose K., et. al.: Increased pain sensitivity in fibromyalgia: effects of stimulus type and mode of presentation. Pain 2003; 105: pp. 403-413.
4. Arroyo J.F., Cohen M.L.: Abnormal responses to electrocutaneous stimulation in fibromyalgia. J Rheumatol 1993; 20: pp. 1925-1931.
5. Lorenz J.: Hyperalgesia or hypervigilance?. Zeitschr Rheumatol 1998; 57: pp. 19-22.
6. Aziz Q., Thompson D.G., Ng V.W., et. al.: Cortical processing of human somatic and visceral sensation. J Neurosci 2000; 20: pp. 2657-2663.
7. Jones A.K., Brown W.D., Friston K.J., et. al.: Cortical and subcortical localization of response to pain in man using positron emission tomography. Proc R Soc Lond B Biol Sci 1991; 244: pp. 39-44.
8. Mountz J.M., Bradley L.A., Modell J.G., et. al.: Fibromyalgia in women. Arthr Rheum 1995; 38: pp. 926-938.
9. Kwiatek R., Barnden L., Tedman R., et. al.: Regional cerebral blood flow in fibromyalgia: single-photon-emission computed tomography evidence of reduction in the pontine tegmentum and thalami. Arthr Rheum 2000; 43: pp. 2823-2833.
10. Gracely R.H., Petzke F., Wolf J.M., et. al.: Functional magnetic resonance imaging evidence of augmented pain processing in fibromyalgia. Arthr Rheum 2002; 46: pp. 1333-1343.
11. Giesecke T., Gracely R.H., Grant M.A., et. al.: Evidence of augmented central pain processing in idiopathic chronic low back pain. Arthr Rheum 2004; 50: pp. 613-623.
12. Cook D.B., Lange G., Ciccone D.S., et. al.: Functional imaging of pain in patients with primary fibromyalgia. J Rheumatol 2004; 31: pp. 364-378.
13. Ross A.J., Sachdev P.S.: Magnetic resonance spectroscopy in cognitive research. Brain Res Brain Res Rev 2004; 44: pp. 83-102.
14. Grachev I.D., Fredrickson B.E., Apkarian A.V.: Abnormal brain chemistry in chronic back pain: an in vivo proton magnetic resonance spectroscopy study. Pain 2000; 89: pp. 7-18.
15. Brooks J., Tracey I.: From nociception to pain perception: imaging the spinal and supraspinal pathways. J Anat 2005; 207: pp. 19-33.
16. Singer T, Seymour B, O’Doherty J, et al. Empathy for pain involves the affective but not sensory components of pain. Science 2044; 303:1157–1162.
17. Critchley H.D., Wiens S., Rotshtein P., et. al.: Neural systems supporting interoceptive awareness. Nat Neurosci 2004; 7: pp. 189-195.
18. Craig A.D., Chen K., Bandy D., et. al.: Thermosensory activation of insular cortex. Nat Neurosci 2000; 3: pp. 184-190.
19. Mosely M., Cohen Y., Kucharczyk J., et. al.: Diffusion-weighted MR-imaging of anisotropic water diffusion in cat central nervous system. Radiology 1990; 176: pp. 439-445.
20. Basser P.J., Pierpaoli C.: Microstructural and physiological features of tissues elucidated by quantitative-diffusion-tensor MRI. J Magn Reson 1996; pp. 209-219. Series B 111
21. Sundgren P.C., Dong Q., Gomez-Hassan D., et. al.: Diffusion tensor imaging of the brain. Neuroradiology 2004; 46: pp. 339-350.
22. Hadjipavlou G., Dunckley P., Behrens T.E., et. al.: Determining anatomical connectivities between cortical and brainstem pain processing regions in humans: a diffusion tensor imaging study in healthy controls. J Pain 2006; 123: pp. 169-178.
23. Seghier M.L., Lazeyras F., Vuilleumier P., et. al.: Functional magnetic resonance imaging and diffusion tensor imaging in a case of central poststroke pain. J Pain 2005; 6: pp. 208-212.
24. Wolfe F., Smythe H.A., Yunus M.B., et. al.: The American College of Rheumatology 1990 criteria for the classification of fibromyalgia. Arthritis Rheum 1990; 33: pp. 160-172.
25. Welsh R.C., Rahbar H., Foerster B.: Brain diffusivity in patients with neuropsychiatric systemic lupus erythematosus with new acute neurological symptoms. J Magn Reson 2007; In press
26. Meyer C.R., Boes J.L., Kim B., et. al.: Demonstration of accuracy and clinical versatility of mutual information for automatic multimodality image fusion using affine and thin plate spline warped geometric deformations. Med Image Anal 1997; 1: pp. 195-206.
27. Petzke F., Khine A., Williams D., et. al.: Dolorimetry performed at 3 paired tender points highly predicts overall tenderness. J Rheumatol 2001; 28: pp. 2568-2569.
28. Petzke F., Harris R.E., Williams D.A., et. al.: Differences in unpleasantness induced by experimental pressure between patients with fibromyalgia and controls. Eur J Pain 2005; 9: pp. 325-335.
29. Gracely R.H., Lota L., Walter D.J., et. al.: A multiple random staircase method of psychophysical pain assessment. Pain 1988; 32: pp. 55-63.
30. Radloff L.S.: The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Measur 1977; 1: pp. 385-401.
31. Spielberger CD, Gorsuch RC, Lushene RE, et al. (1983). Manual for the State Trait Anxiety Inventory (Form Y): (“Self-evaluation questionnaire”). Palo Alto, Ca: Consulting Psychologists, 1983.
32. Skevington S.M.: A standardized scale to measure beliefs about controlling pain (BPCQ): a preliminary study. Psychol Health 1990; 4: pp. 221-232.
33. Levene H.: (1960)Olkin I. et. al.Contributions to probability and statistics: essays in honor of Harold Hotelling.1960.Stanford University PressStanford, Ct:pp. 278-292.
34. Petrou M., Foerster B., Fan X.: Two D-CSI MR spectroscopy in the evaluation of fibromyalgia patients: a prospective study comparing fibromyalgia patients with normal healthy controls.2005.pp. 78. European Society of Neuroradiology Annual Meeting
35. Petrou M., Foerster B., Fan X.: Metabolite abnormalities in potential pain processing brain regions of fibromyalgia patients using MR spectroscopy.2006.European Congress of Radiologypp. 313.
36. Foerster BR, Petrou M, Clauw DJ, et al. Cerebral perfusion differences in pain processing regions of fibromyalgia patients using MR perfusion techniques [abstract] To be presented at the European Congress of Radiology 2007, Vienna, Austria.