Rationale and Objectives
We sought to investigate the value of diffusion-weighted MR imaging in evaluating focal hepatic nodules in an experimental hepatocellular carcinoma (HCC) rat model.
Materials and Methods
Forty rats with chemically induced primary hepatic nodules ranging pathologically from regenerative nodules (RNs) to dysplastic nodules (DNs) to HCC were examined with diffusion-weighted imaging. The apparent diffusion coefficient (ADC) values of hepatic nodular lesions were calculated. Tukey’s HSD post hoc test was used to compare the difference in ADC values between different hepatic nodular lesions.
Results
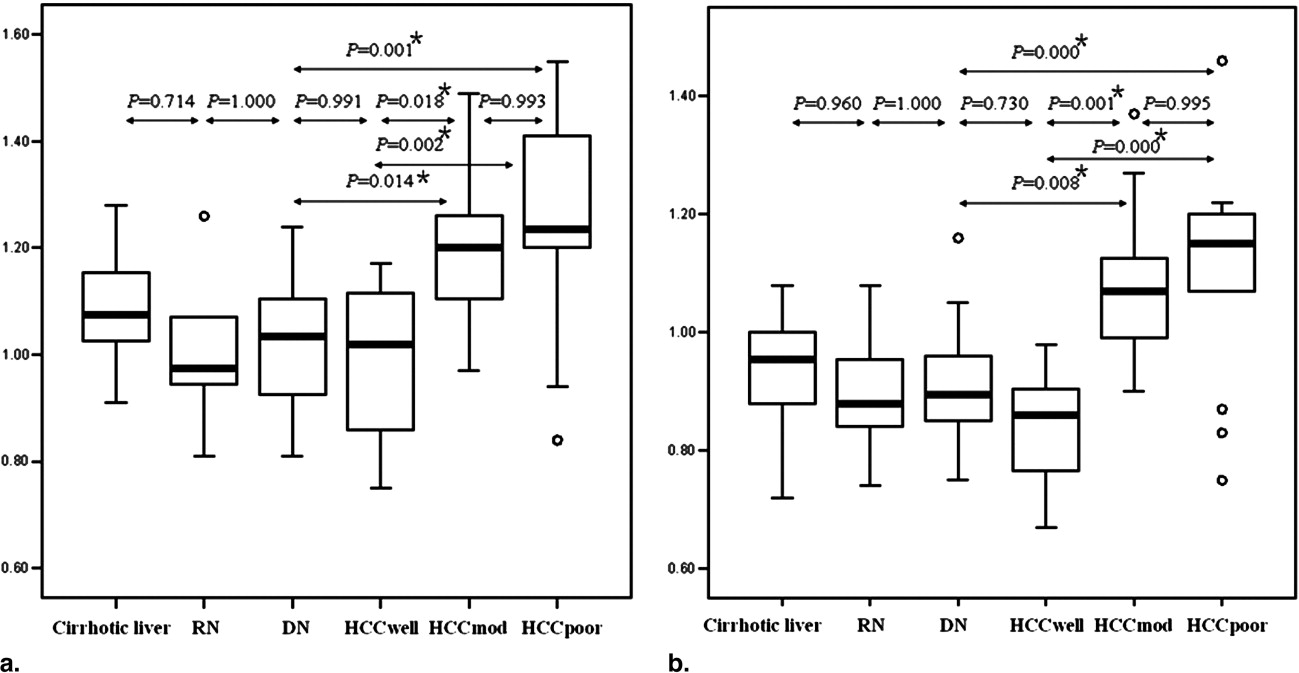
Eight RNs, 16 DNs, 7 well-differentiated HCCs (HCC well ), 11 moderately differentiated HCCs (HCC mod ), and 14 poorly differentiated HCCs (HCC poor ) were evaluated. There was no significant difference between RNs and DNs ( P > 0.05). Although the ADC values of HCC well were slightly lower than those of DNs, there was no significant difference between them ( P > 0.05). The ADC values of HCC mod and HCC poor were significantly higher ( P < 0.05) than those of other nodules, and no significant difference was seen between HCC mod and HCC poor ( P > 0.05).
Conclusion
Diffusion-weighted magnetic resonance imaging can be useful in characterizing focal hepatic nodular lesions, but ADC values cannot be used efficiently to distinguish HCC well from DNs.
Hepatocellular carcinoma (HCC) is the most common primary malignant tumor of the liver, with highest incidences occurring in Africa, Southeast Asia, and China ( ). A cirrhotic liver is often the background from which HCC arises. One pathway to the development of HCC in patients with cirrhosis is a multistep carcinogenesis process from benign regenerative nodule (RN) to dysplastic nodule (DN) to a dysplastic nodule with microscopic foci of HCC, which may enlarge and replace the nodule giving rise to a small HCC, and finally to the overt HCC ( ). DNs are considered precancerous lesions of HCC ( ). Therefore, it is clinically important to detect DNs and HCC at an early stage for prompt surgical resection, transplantation, or local ablation therapy to ensure a better chance of survival.
Diffusion-weighted (DW) MRI is an imaging technique used to show microscopic motion in biologic tissues ( ). The apparent diffusion coefficient (ADC), a quantity calculated from the DW MR images, combines the effects of capillary perfusion and water diffusion in the extracellular extravascular space ( ). Thus, DW MRI is currently the only imaging method for assessing in vivo perfusion and diffusion simultaneously within the same organ ( ).
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Materials and methods
Animal Model
Get Radiology Tree app to read full this article<
MR Imaging
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Histology
Get Radiology Tree app to read full this article<
Image Analysis
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Statistical Analysis
Get Radiology Tree app to read full this article<
Results
Get Radiology Tree app to read full this article<
Table 1
ADC values of liver lesions calculated with various sets of b values
Liver lesions No. ADC (×10 −3 mm 2 /sec) of liver lesions calculated with various sets of b values Low b values ( b = 0, 600 sec/mm 2 ) High b values ( b = 0, 1,000 sec/mm 2 ) Cirrhotic liver 32 1.08 ± 0.09 0.94 ± 0.09 RNs 8 1.01 ± 0.13 0.90 ± 0.10 DNs 16 1.02 ± 0.11 0.91 ± 0.11 HCC well 7 0.98 ± 0.17 0.84 ± 0.12 HCC mod 11 1.21 ± 0.17 1.08 ± 0.14 HCC poor 14 1.24 ± 0.21 1.11 ± 0.18
Data are expressed as mean ± SD. RN, regenerative nodule; DN, dysplastic nodule; HCC well , well-differentiated HCC; HCC mod , moderately differentiated HCC; HCC poor , poorly differentiated HCC.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Discussion
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Acknowledgments
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
References
1. Unoura M., Kaneko S., Matsushita E., et. al.: High-risk groups and screening strategies for early detection of hepatocellular carcinoma in patients with chronic liver disease. Hepatogastroenterology 1993; 40: pp. 305-310.
2. Parkin D.M.: Global cancer statistics in the year 2000. Lancet Oncol 2001; 2: pp. 533-543.
3. Bosch F.X., Ribes J., Borras J.: Epidemiology of primary liver cancer. Semin Liver Dis 1999; 19: pp. 271-285.
4. International Working Party: Terminology of nodular hepatocellular lesions. Hepatology 1995; 22: pp. 983-993.
5. Kobayashi M., Ikeda K., Hosaka T., et. al.: Dysplastic nodules frequently develop into hepatocellular carcinoma in patients with chronic viral hepatitis and cirrhosis. Cancer 2006; 106: pp. 636-647.
6. Efremidis S.C., Hytiroglou P.: The multistep process of hepatocarcinogenesis in cirrhosis with imaging correlation. Eur Radiol 2002; 12: pp. 753-764.
7. Taguchi K., Aishima S., Matsuura S., et. al.: Significance of the relationship between irregular regeneration and two hepatocarcinogenic pathways: “De novo” and so-called “dysplastic nodule-hepatocellular carcinoma” sequence. J Surg Oncol 2005; 92: pp. 100-103.
8. Kojiro M.: Focus on dysplastic nodules and early hepatocellular carcinoma: An Eastern point of view. Liver Transpl 2004; 10: pp. S3-S8.
9. Hayashi M., Matsui O., Ueda K., Kawamori Y., Gabata T., Kadoya M.: Progression to hypervascular hepatocellular carcinoma: Correlation with intranodular blood supply evaluated with CT during intraarterial injection of contrast material. Radiology 2002; 225: pp. 143-149.
10. Le Bihan D., Breton E., Lallemand D., Aubin M.L., Vignaud J., Laval-Jeantet M.: Separation of diffusion and perfusion in intravoxel incoherent motion MR imaging. Radiology 1988; 168: pp. 497-505.
11. Le Bihan D., Breton E., Lallemand D., Grenier P., Cabanis E., Laval-Jeantet M.: MR imaging of intravoxel incoherent motions: Application to diffusion and perfusion in neurologic disorders. Radiology 1986; 161: pp. 401-407.
12. Turner R., Le Bihan D., Maier J., Vavrek R., Hedges L.K., Pekar J.: Echo-planar imaging of intravoxel incoherent motion. Radiology 1990; 177: pp. 407-414.
13. Namimoto T., Yamashita Y., Sumi S., Tang Y., Takahashi M.: Focal liver masses: Characterization with diffusion-weighted echo-planar MR imaging. Radiology 1997; 204: pp. 739-744.
14. Ichikawa T., Haradome H., Hachiya J., Nitatori T., Araki T.: Diffusion-weighted MR imaging with a single-shot echoplanar sequence: Detection and characterization of focal hepatic lesions. AJR Am J Roentgenol 1998; 170: pp. 397-402.
15. Kim T., Murakami T., Takahashi S., Hori M., Tsuda K., Nakamura H.: Diffusion-weighted single-shot echoplanar MR imaging for liver disease. AJR Am J Roentgenol 1999; 173: pp. 393-398.
16. Taouli B., Vilgrain V., Dumont E., Daire J.L., Fan B., Menu Y.: Evaluation of liver diffusion isotropy and characterization of focal hepatic lesions with two single-shot echo-planar MR imaging sequences: Prospective study in 66 patients. Radiology 2003; 226: pp. 71-78.
17. Ha W.S., Kim C.K., Song S.H., Kang C.B.: Study on mechanism of multistep hepatotumorigenesis in rat: Development of hepatotumorigenesis. J Vet Sci 2001; 2: pp. 53-58.
18. Fournier L.S., Cuenod C.A., de Bazelaire C., et. al.: Early modifications of hepatic perfusion measured by functional CT in a rat model of hepatocellular carcinoma using a blood pool contrast agent. Eur Radiol 2004; 14: pp. 2125-2133.
19. Tsuda N., Kato N., Murayama C., Narazaki M., Yokawa T.: Potential for differential diagnosis with gadolinium-ethoxybenzyl-diethylenetriamine pentaacetic acid-enhanced magnetic resonance imaging in experimental hepatic tumors. Invest Radiol 2004; 39: pp. 80-88.
20. Kojiro M., Roskams T.: Early hepatocellular carcinoma and dysplastic nodules. Semin Liver Dis 2005; 25: pp. 133-142.
21. Matsui O., Kadoya M., Kameyama T., et. al.: Benign and malignant nodules in cirrhotic livers: Distinction based on blood supply. Radiology 1991; 178: pp. 493-497.
22. Guan S., Zhao W.D., Zhou K.R., et. al.: Sequential hemodynamic changes in precancerous lesions of hepatocellular carcinoma: Experimental study with MR perfusion. Chin J Radiol 2006; 40: pp. 231-234.
23. Geschwind J.F., Artemov D., Abraham S., et. al.: Chemoembolization of liver tumor in a rabbit model: Assessment of tumor cell death with diffusion-weighted MR imaging and histologic analysis. J Vasc Interv Radiol 2000; 11: pp. 1245-1255.
24. Kim Y.J., Chang K.H., Song I.C., et. al.: Brain abscess and necrotic or cystic brain tumor: Discrimination with signal intensity on diffusion-weighted MR imaging. AJR Am J Roentgenol 1998; 171: pp. 1487-1490.
25. Chan J.H., Tsui E.Y., Luk S.H., et. al.: Diffusion-weighted MR imaging of the liver: Distinguishing hepatic abscess from cystic or necrotic tumor. Abdom Imaging 2001; 26: pp. 161-165.
26. Lang P., Wendland M.F., Saeed M., et. al.: Osteogenic sarcoma: Noninvasive in vivo assessment of tumor necrosis with diffusion-weighted MR imaging. Radiology 1998; 206: pp. 227-235.
27. Deng J., Rhee T.K., Sato K.T., et. al.: In vivo diffusion-weighted imaging of liver tumor necrosis in the VX2 rabbit model at 1.5 Tesla. Invest Radiol 2006; 41: pp. 410-414.
28. Maier C.F., Paran Y., Bendel P., Rutt B.K., Degani H.: Quantitative diffusion imaging in implanted human breast tumors. Magn Reson Med 1997; 37: pp. 576-581.
29. Galons J.P., Altbach M.I., Paine-Murrieta G.D., Taylor C.W., Gillies R.J.: Early increases in breast tumor xenograft water mobility in response to paclitaxel therapy detected by non-invasive diffusion magnetic resonance imaging. Neoplasia 1999; 1: pp. 113-117.