Rationale and Objectives
Thyroid nodules are common in the population, although the rate of malignancy is relatively low (5%–15%). The purpose of this study was to determine if introducing a modified standardized reporting format and management algorithm (Thyroid Imaging Reporting and Data System [TI-RADS]) affects radiologist reporting adherence, number of thyroid biopsies, and other measurable outcomes.
Materials and Methods
All thyroid biopsies performed over two 6-month periods were evaluated at a tertiary care hospital with Research Ethics Board approval. The first period was before implementation of TI-RADS and the second was several months after implementation of TI-RADS (using a modified version made through a multidisciplinary collaboration). The number of biopsies performed was determined in each of the two periods as well as the percent of positive malignancy, wait times, and rates of non-diagnostic/unsatisfactory and inconclusive biopsies, which included atypia of undetermined significance (AUS) and follicular lesion of undetermined significance (FLUS).
Results
The average number of biopsies performed prior to implementing modified Kwak’s TI-RADS was 74 thyroid biopsies per month and the average number of diagnostic ultrasounds was 271. After the introduction of modified Kwak’s TI-RADS, the average number of thyroid biopsies decreased to 60 per month (an 18.9% reduction, P < .05), and the number of diagnostic ultrasound increased to 287 per month (a 5.9% increase from 2016 to 2017). The average wait time for a thyroid biopsy decreased from 5 to 3 weeks ( P < .05). There was a slight increase in the rate of positive malignancy results (from 15% to 18%), although it was not statistically significant. The rate of non-diagnostic/unsatisfactory and inconclusive results (including AUS and FLUS) remained unchanged (18% AUS/FLUS/15% non-diagnostic/unsatisfactory before and 17% AUS/FLUS/15% non-diagnostic/unsatisfactory after TI-RADS introduction, P > .05).
Conclusions
Introduction of a multidisciplinary-approved standardized reporting system with evidence-based management recommendations led to no statistically significant change in the number of diagnostic ultrasounds but a statistically significant reduction in the number of monthly thyroid biopsies and associated reduction in wait times.
Introduction
Studies have estimated that up to 67% of North Americans have thyroid nodules but that of these nodules only 5%–15% will be malignant . There has been a 2.4-fold increase in the incidence of thyroid cancer in the past 30 years; this increase in diagnosis is commonly considered to result from better technology and more frequent use of cross-sectional imaging . Despite an increase in overall thyroid diagnosis, the 5-year mortality rate for thyroid cancer has been stable at a relatively low 5%–7% since 2005 . Some studies estimate that up to 50% of thyroid cancers will remain indolent over a patient’s life time .
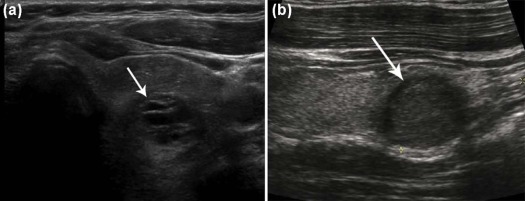
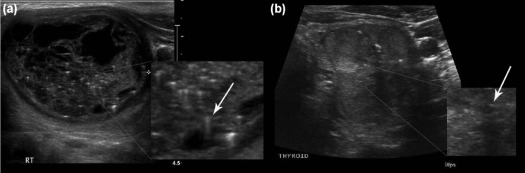
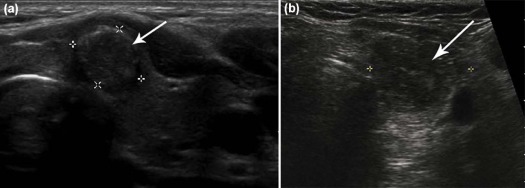
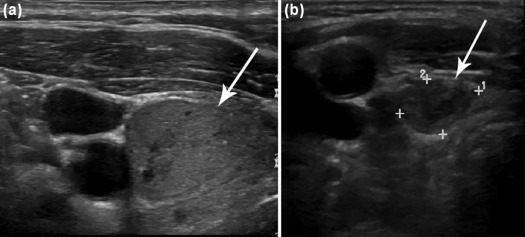
With more thyroid nodules being detected, emphasis should be placed on consistent imaging technique, template reporting use, and standardized management recommendations by radiologists. One of the main challenges in this sequence of events is determining which nodules require biopsy and which ones are better left alone ( Fig 1 ). A further concern is discerning which part of heterogenous nodules requires biopsy ( Fig 1 ).
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Methods
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
TABLE 1
Modified Version of TI-RADS Used in Our Institution Entitled “COP-modified TI-RADS”
COP, Community of Practice; TI-RADS, Thyroid Imaging Reporting and Data System; TOH, The Ottawa Hospital.
TABLE 2
Comparison of “COP-modified TI-RADS” to ATA Guidelines
COP-modified TI-RADS Definition COP-modified TI-RADS Management ATA Comparator Definition ATA Guideline Recommendation TR-1
NO ABNORMALITY IDENTIFIED No biopsy
No follow-up No specific category None TR-2
0% risk of malignancy BENIGN:
Spongiform
Colloid
Cyst
Giraffe hide pattern No biopsy
No follow-up BENIGN 0%
Purely cystic nodules (no solid component) No biopsy TR-3
<2% risk of malignancy
PROBABLY BENIGN:
Mixed composition
No suspicious US features No biopsy
No follow-up VERY LOW SUSPICION <3% risk of malignancy
Partially cystic nodules without any of the sonographic features described in low, intermediate or high suspicion patterns or Spongiform Consider biopsy at >20 mm (weak recommendation, low-quality evidence) TR-4F: New Thyroid COP designation*
DEFINITIONS
a) <10 mm and >1 “suspicious” features
b) Equivocal case (radiologist has low confidence in images provided)
c) Known prior cancer = (hemithyroidectomy) Yearly follow-up (indefinitely until category changes or until better evidence medicine published in literature) No specific guidelines exists as a direct comparison in ATA None as a direct equivalent to COP-modified TIRADS 4F does not exist in ATA TR-4A:
2%–10% risk of malignancy
LOW SUSPICION OF MALIGNANCY:
One suspicious US feature; eg, solid composition Follow-up at 12 months
Or
Biopsy at 15 mm if positive clinical factors (as per requesting physician) LOW Suspicion
5%–10% risk of malignancy
Isoechoic or hyperechoic solid nodule
Or
Partially cystic nodule with eccentric hypoechoic solid areas. NO microcalcification, irregular margin or extrathyroidal extension, or taller than wide shape Biopsy at 15 mm (weak recommendation, low-quality evidence) TR-4B*:
10%–20% risk of malignancy
INTERMEDIATE SUSPICION OF MALIGNANCY:
Solid AND hypoechoic to thyroid parenchyma Biopsy at 15 mm INTERMEDIATE Suspicion 10–20% risk of malignancy
Hypoechoic to thyroid
and > 95% solid nodule
With smooth margins Without microcalcifications, extrathyroidal extension, or taller than wide shape Recommend Biopsy at 1.5 cm (strong recommendation, low-quality evidence) TR-4B:
10%–50% risk of malignancy
INTERMEDIATE SUSPICION OF MALIGNANCY
Any TWO high suspicious features Biopsy at 10 mm HIGH Suspicion >70%–90%
Solid hypoechoic nodule or solid hypoechoic component of a partially cystic nodule with one or more of the following features: irregular margins (infiltrative, microlobulated), microcalcifications, taller than wide shape, rim calcifications with small extrusive soft tissue component, evidence of extrathyroidal extension Biopsy at 10 mm (strong recommendation, moderate-quality evidence) TR-4C:
50%–95% risk of malignancy
MODERATE CONCERN,
but not classic for malignancy:
(three or four suspicious US features) Biopsy at 10 mm Same as directly above Biopsy at 10 mm (strong recommendation, moderate-quality evidence) TR-5:
95% risk of malignancy
HIGHLY SUGGESTIVE OF MALIGNANCY:
Five suspicious US features from: solid composition, microcalcifications, taller than wide, hypoechoic, very hypoechoic, and irregular borders Biopsy at 10 mm Same as directly above Biopsy at 10 mm (strong recommendation, moderate-quality evidence)
ATA, American Thyroid Association; COP, Community of Practice; TI-RADS, Thyroid Imaging Reporting and Data System.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Results
Adherence
Get Radiology Tree app to read full this article<
TABLE 3
Adherence Rate of Radiologist at the Beginning, Middle, and End of the Study Period
Get Radiology Tree app to read full this article<
Number of Biopsies
Get Radiology Tree app to read full this article<
TABLE 4
Average Number of Biopsies per Month Before and After the Introduction of TI-RADS
Get Radiology Tree app to read full this article<
Wait times
Get Radiology Tree app to read full this article<
TABLE 5
Average Wait Time for Thyroid Biopsies Across Our Institution Before and After TI-RADS Implementation ( P < .05)
Get Radiology Tree app to read full this article<
Malignancy Rates
Get Radiology Tree app to read full this article<
TABLE 6
Average Malignancy Rate of Confirmed Biopsies per Month Before and After TI-RADS Implementation ( P > .05)
Get Radiology Tree app to read full this article<
Insufficient/Inconclusive Rates
Get Radiology Tree app to read full this article<
Discussion
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
PDSA/Adherence
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Number of Diagnostic Imaging Cases, Biopsies, and Wait Times
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Malignancy Rates
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Non-diagnostic/Unsatisfactory and AUS/FLUS Results
Get Radiology Tree app to read full this article<
Study Limitations
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Conclusion
Get Radiology Tree app to read full this article<
Acknowledgments
Get Radiology Tree app to read full this article<
References
1. Haugen B.R., Alexander E.K., Bible K.C., et. al.: 2015 American Thyroid Association Management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association guidelines task force on thyroid nodules and differentiated thyroid cancer, thyroid. Off J Am Thyroid Assoc 2016; 26: pp. 1-133.
2. Rahib L., Smith B.D., Aizenberg R., et. al.: Projecting cancer incidence and deaths to 2030: the unexpected burden of thyroid, liver, and pancreas cancers in the United States. Cancer Res 2014; 74: pp. 2913-2921.
3. Brito J.P., Morris J.C., Montori V.M.: Thyroid cancer: zealous imaging has increased detection and treatment of low risk tumours. BMJ 2013; 347: pp. f4706.
4. SEER : Cancer of the thyroid—SEER stat fact sheets. n.d.; Available at: http://seer.cancer.gov/statfacts/html/thyro.html
5. Vollmer R.T.: Revisiting overdiagnosis and fatality in thyroid cancer. Am J Clin Pathol 2014; 141: pp. 128-132.
6. O’Grady T.J., Gates M.A., Boscoe F.P.: Thyroid cancer incidence attributable to overdiagnosis in the United States 1981–2011. Int J Cancer 2015; 137: pp. 2664-2673.
7. Reiner B.I.: The challenges, opportunities, and imperative of structured reporting in medical imaging. J Digit Imaging 2009; 22: pp. 562-568.
8. Balleyguier C., Ayadi S., Nguyen K.V., et. al.: BIRADSTM classification in mammography. Eur J Radiol 2007; 61: pp. 192-194.
9. Tessler F.N., Middleton W.D., Grant E.G., et. al.: ACR Thyroid Imaging, Reporting and Data System (TI-RADS): white paper of the ACR TI-RADS committee. J Am Coll Radiol 2017; 14: pp. 587-595.
10. Kwak J.Y., Han K.H., Yoon J.H., et. al.: Thyroid imaging reporting and data system for US features of nodules: a step in establishing better stratification of cancer risk. Radiology 2011; 260: pp. 892-899.
11. Cibas E.S., Ali S.Z.: The Bethesda system for reporting thyroid cytopathology. Am J Clin Pathol 2009; 132: pp. 658-665.
12. Chandramohan A., Khurana A., Pushpa B.T., et. al.: Is TI-RADS a practical and accurate system for use in daily clinical practice?. Ind J Radiol Imaging 2016; 26: pp. 145-152.
13. Xu T., Gu J.-Y., Ye X.-H., et. al.: Thyroid nodule sizes influence the diagnostic performance of TI-RADS and ultrasound patterns of 2015 ATA guidelines: a multicenter retrospective study. Sci Rep 2017; 7: pp. 43183.
14. Wei X., Li Y., Zhang S., et. al.: Thyroid imaging reporting and data system (TI-RADS) in the diagnostic value of thyroid nodules: a systematic review. Tumor Biol 2014; 35: pp. 6769-6776.
15. Horvath E., Majlis S., Rossi R., et. al.: An ultrasonogram reporting system for thyroid nodules stratifying cancer risk for clinical management. J Clin Endocrinol Metab 2009; 94: pp. 1748-1751.
16. Russ G., Royer B., Bigorgne C., et. al.: Prospective evaluation of thyroid imaging reporting and data system on 4550 nodules with and without elastography. Eur J Endocrinol 2013; 168: pp. 649-655.
17. Yoon J.H., Lee H.S., Kim E.-K., et. al.: Malignancy risk stratification of thyroid nodules: comparison between the thyroid imaging reporting and data system and the 2014 American Thyroid Association Management Guidelines. Radiology 2016; 278: pp. 917-924.
18. Misiakos E.P., Margari N., Meristoudis C., et. al.: Cytopathologic diagnosis of fine needle aspiration biopsies of thyroid nodules. World J Clin Cases 2016; 4: pp. 38-48.
19. Ko S.Y., Lee H.S., Kim E.-K., et. al.: Application of the thyroid imaging reporting and data system in thyroid ultrasonography interpretation by less experienced physicians. Ultrasonography 2014; 33: pp. 49-57.
20. Cheng S.-P., Lee J.-J., Lin J.-L., et. al.: Characterization of thyroid nodules using the proposed thyroid imaging reporting and data system (TI-RADS). Head Neck 2013; 35: pp. 541-547.
21. Horvath E., Silva C.F., Majlis S., et. al.: Prospective validation of the ultrasound based TI-RADS (Thyroid Imaging Reporting And Data System) classification: results in surgically resected thyroid nodules. Eur Radiol 2017; 27: pp. 2619-2628.
22. Grani G., Lamartina L., Ascoli V., et. al.: Ultrasonography scoring systems can rule out malignancy in cytologically indeterminate thyroid nodules. Endocrine 2017; 57: pp. 256-261.
23. Srinivas M.N.S., Amogh V.N., Gautam M.S., et. al.: A prospective study to evaluate the reliability of thyroid imaging reporting and data system in differentiation between benign and malignant thyroid lesions. J Clin Imaging Sci 2016; 6: pp. 5.