Rationale and Objectives
The conceptualization of acetabular fractures can present a daunting challenge to radiology residents. 3D models have been shown to aid in the spatial perception of complicated anatomy and may help residents grasp the elaborate classification systems for these anatomically complex fractures. Prior studies have explored the utility of 3D printed models for surgical planning in various settings. To our knowledge, no study has evaluated their efficacy in radiology resident training.
Materials and Methods
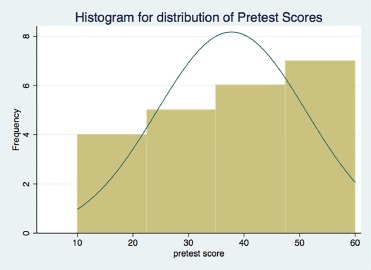
Following IRB approval, 22 radiology residents were randomized and stratified by Post Graduate Year into two groups of 11 residents. Both groups received separate identical presentations on the 5 most common acetabular fractures given by a musculoskeletal trained radiologist. Residents in the experimental group received 3D printed models of the five most common fracture types with which to interact during the presentation, while the control group did not. Both groups received a pretest and a follow up posttest three weeks later.
Results
A Wilcoxon rank sum test was performed to determine if statistically significant differences between the pretest and posttest scores of the experimental and control groups existed. There was no statistically significant difference in scores on the pre-test, which confirmed successful randomization. There was a statistically significant difference (P = 0.02) on the posttest scores between the experimental and control groups.
Conclusion
3D printed models promise as an effective educational tool for resident learning with respect to acetabular fractures, improving short-term understanding of complex anatomy and classification systems.
INTRODUCTION
Three Dimensional (3D) printing has increasingly become prevalent throughout medicine, particularly in its applications within neurosurgery, orthopedics, pulmonology, and cardiology ( ). The use of these models to enhance surgical simulation, pre-operative planning, intra-operative guidance, and for creating implants/prostheses has been well studied and documented ( ). However, much less has been studied on the educational effects of 3D models on education, learning, and retention of information. Preliminary studies have suggested that these models enhance knowledge of complex anatomy and understanding of difficult concepts for medical trainees ( ).
Understanding the classification of acetabular fractures is one among many applications of 3D printed models, given the complexity of the anatomy. This is particularly relevant in orthopedics and radiology, as an accurate diagnosis of the type of acetabular fracture influences treatment and outcomes; since different types of acetabular fractures are repaired by different surgical approaches and techniques ( ). The most widely used classification for acetabular fractures is the Judet and Letournel classification, which classifies fractures in 10 different types; with five (both column type, T-shaped, transverse, transverse with posterior wall, and isolated posterior wall) of the ten types accounting for approximately 90% of acetabular fractures seen on imaging ( ).
Get Radiology Tree app to read full this article<
MATERIALS AND METHODS
Study Population
Get Radiology Tree app to read full this article<
Table 1
Baseline Characteristics of Study Sample
Intervention Group Control Group Mean age (years) 30.0 30.1 Sex Male 7 (63.6%) 8 (72.7%) Female 4 (36.4%) 3 (27.3%) Number of residents 11 11 PGY*2 3 3 PGY3 3 3 PGY4 2 3 PGY5 3 2
Get Radiology Tree app to read full this article<
3D Printed Models
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Study Design
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Outcome Ascertainment and Statistical Analyses
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
RESULTS
Get Radiology Tree app to read full this article<
Table 2
Distribution of Mean and Median Test Scores by Study sample, Intervention Group, and Control Group
Entire study Intervention Group Control Group sample (N=11 residents) (N=22 residents) (N=11 residents) Mean score on pretest (standard deviation) 37.7 (13.4) 36.4 (15.0) 39.1 (12.2) Median score on pretest 40 40 40 Mean score on posttest (standard deviation) 63.6 (16.8) 71.8 (18.3) 55.5 (10.4) Median score on posttest 60 70 50 Mean difference in scores (standard deviation) 25.9 (21.5) 35.5 (23.4) 16.4 (15.0) Median difference in scores 25 30 20
Table 3
Distribution of Mean and Median Test Scores by Post Graduate Level (PGY) of Training.
(N = 6 residents) (N = 6 residents) (N = 5 residents) (N = 5 residents) Mean score on Pretest (Standard deviation) 38.3 (7.53) 41.7 (14.7) 38 (13.0) 32 (19.2) Median score on Pretest 40 45 40 30 Mean score on Posttest (Standard deviation) 58.3 (14.7) 71.7 (19.4) 58.0 (8.4) 66.0 (21.9) Median score on Posttest 55 75 60 60 Mean difference in scores (Standard deviation) 20.0 (14.1) 30.0 (32.2) 20.0 (12.2) 34.0 (23.0) Median difference in scores 20 25 20 30
Table 4
Results of the Wilcoxon Rank Sum Tests by Pretest, Posttest, and Difference between Pretest and Post test.
Pretest Posttest Difference between Pretest and Posttest P Value 0.74 0.02 0.04
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
DISCUSSION
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
CONCLUSION
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
References
1. Manganaro MS, Morag Y, Weadock WJ, et. al.: Creating three-dimensional printed models of acetabular fractures for use as educational tools. RadioGraphics 2017; 37: pp. 871-880.
2. Matsumoto JS, Morris JM, Foley TA, et. al.: Three-dimensional physical modeling: applications and experience at Mayo Clinic. RadioGraphics 2015; 35: pp. 1989-2006.
3. McMenamin PG, Quayle MR, McHenry CR, et. al.: The production of anatomical teaching resources using three-dimensional (3D) printing technology. Anat Sci Educ 2014; 7: pp. 479-486.
4. Bagaria V, Chaudhary K: A paradigm shift in surgical planning and simulation using 3Dgraphy: experience of first 50 surgeries done using 3D-printed biomodels. Injury 2017; 48: pp. 2501-2508.
5. Liu ZJ, Jia J, Zhang YG, et. al.: Internal fixation of complicated acetabular fractures directed by preoperative surgery with 3D printed models. Orthop Surg 2017; 9: pp. 257-260.
6. Chen X, Chen X, Zhang G, et. al.: Accurate fixation of plates and screws for the treatment of acetabular fractures using 3D-printed guiding templates: an experimental study. Injury 2017; 48: pp. 1147-1154.
7. Wang H, Wang F, Newman S, et. al.: Application of an innovative computerized virtual planning system in acetabular fracture surgery: a feasibility study. Injury 2016; 47: pp. 1698-1701.
8. Hassinger JP, Dozois EJ, Holubar EJ, et. al.: Virtual pelvic anatomy simulator: a pilot study of usability and perceived effectiveness. J Surg Res 2010; 161: pp. 23-27.
9. Potok PS, Hopper KD, Umlauf MJ: Fractures of the acetabulum: imaging, classification, and understanding. RadioGraphics 1995; 15: pp. 7-23.
10. Goulet JA, Bray TJ: Complex acetabular fractures. Clin Orthop Relat Res 1989; 240: pp. 9-20.
11. Brandser E, Marsh JL: Acetabular fractures: easier classification with a systematic approach. AJR Am J Roentgenol 1998; 171: pp. 1217-1228.
12. Letournel E, Judet R: Fractures of the acetabulum.2nd ed1993.Springer-VerlagHeidelberg, Germany
13. Hunter JC, Brandser EA, Tran KA: Pelvic and acetabular trauma. Radiol Clin North Am 1997; 35: pp. 559-590.
14. Huang Z, Song W, Zhang Y, et al. Three-dimensional printing model improves morphological understanding in acetabular fracture learning: aA multicenter, randomized, controlled study. PLoS One 2018: 13: e0191328.
15. Kim JW, Lee Y, Seo J, et. al.: Clinical experience with three-dimensional printing techniques in orthopedic trauma. J Orthop Sci 2018; 23: pp. 383-388.
16. Venail F, Deveze A, Lallemant B, et. al.: Enhancement of temporal bone anatomy learning with computer 3D rendered imaging software. Med Teach 2010; 32: pp. e282-e288.