Rationale and Objectives
Given recent advances in and wider availability of complex imaging, physicians are expected to understand imaging appropriateness. We introduced second-year medical students to the American College of Radiology Appropriateness Criteria (ACR-AC) in an interactive case-based elective to demonstrate their use in imaging for common emergency department clinical complaints.
Materials and Methods
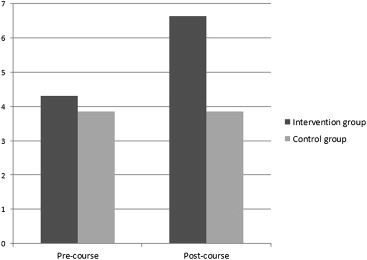
Prospective pre- and post-test design assessed second-year medical students’ performance on case-based knowledge applications and self-assessed confidence related to ACR-AC guidelines compared to second-year students participating in a different concurrent radiology elective. Students participated in a 3-day elective covering the ACR-AC, comparative effective imaging, and risks associated with imaging radiation exposure, with outcomes of perceived confidence using a 5-point Likert scale and knowledge of ACR-AC using case-based multiple choice questions. Analysis included computing mean scores and assessing effect sizes for changes in knowledge.
Results
Before the elective, 24 students scored an average of 3.45 questions correct of 8 (43.1%). On course completion, students scored an average of 5.3 questions correct of the same questions (66.3%) ( P < .001; effect size [Cohen’s d ] = 1.3940. In the comparison group, 12 students scored an average of 3.08 questions (38.5%) correctly pretest and 3.09 questions (38.6%) correctly post-test ( P > .85; effect size = 0.008). Students’ confidence in ordering appropriate imaging improved nearly 2-fold from a range of 1.9 to 3.2 (on a scale of 1.0 to 5.0) to a range of 3.7 to 4.5.
Conclusions
Following a short radiology elective, second-year medical students improved their knowledge of appropriate image utilization and perceived awareness of the indications, contraindications, and effects of radiation exposure related to medical imaging.
Over the past few decades, the United States has seen an unprecedented increase in the cost of health care to the point that sustainable health care delivery at this rate is doubtful. The evolution in advanced medical imaging is a major driving factor in escalating health care expenditures . Technological progress and widespread availability of complex imaging modalities have led to enormous increases in the numbers of appropriate (and inappropriate) imaging studies performed in the United States. It has been suggested that approximately one-third of health care spending is medically unnecessary . While advanced imaging does lead to more expeditious diagnoses and diagnostic certainty and can obviate the need for more invasive procedures, it is not without risks. The greater number of imaging tests ordered also increases reliance on technology over clinical history and examination skills, generates additional imaging or procedures to investigate and treat incidental findings, and adds to patient radiation exposure. With health care reform looming and the certainty of finite resources, it is more crucial than ever that future physicians are educated regarding appropriate imaging utilization and evidence-based imaging, not only to relieve stress on an overburdened health care system but also, most importantly, to provide optimal patient care and minimize risk.
Medical students receive little or no formal radiology training in most medical schools; if they receive training, it is limited to small amounts of didactic information at best . In a recent survey, only about 25% of US medical schools required radiology as a clinical rotation, and in schools that did not require it, up to 63% of students planned on taking radiology as an elective . In most North American medical schools, radiology is typically introduced in the preclinical years as a subsection of anatomy or pathology courses. Then, during clinical years, students are usually taught radiology by nonradiologist clinicians during medicine and surgery clerkships with occasional viewing of images, unless the student opts for a dedicated radiology elective. This is the status quo at our institution, where students receive some didactic teaching during the preclinical years that is delivered by radiologists during anatomy and systems-based pathology lectures, followed by a handful of lectures on chest radiology during the third-year medicine clerkship delivered by an attending internist. Students may then opt to take a dedicated radiology elective during their late third or fourth medical year.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Materials and methods
Course Curriculum
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Table 1
Division of Topics Presented during Three 2-Hour Sessions
Lecture title Subtopics covered Introductory Lecture Introduction to imaging (10 minutes) The ACR appropriateness criteria (10 minutes) Worked example of clinical case and use of the ACR-AC (10 minutes) Evidence-Based Medicine The current status of the health care system (10 minutes) Why we need evidence-based medicine and imaging now more than ever (10 minutes) Cardiothoracic Imaging in the Emergency Department Introduction to cardiothoracic imaging modalities (5 minutes)
Cases including noncardiac chest pain, suspected pneumonia, chest trauma, suspected aortic disease, and suspected pulmonary embolism (10 minutes) Pediatric and Musculoskeletal Imaging Pediatric nonaccidental trauma with worked examples of the ACR-AC (20 minutes)
Imaging of the ankle and foot injuries with worked examples of the ACR-AC (15 minutes) Abdominal Imaging Imaging of common causes of abdominal pain with emphasis on right upper and right lower quadrant pain in adults and children with worked examples using the ACR-AC (20 minutes) Pelvic Imaging Imaging workup of pelvic pain in pregnant and nonpregnant females with worked examples using the ACR-AC (15 minutes) Introduction to Neuroradiology Introduction to neurologic imaging of emergency department patients, including headache, acute and chronic back pain, and trauma, using a case-based approach and the ACR-AC (45 minutes)
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Table 2
Clinical Scenarios for Student Presentations in the Final Session
Vaginal Bleeding (First Trimester and Second/Third Trimester) Child with headache Diabetic foot ulcer Child with a limp Acute cold leg Hematuria Scrotal pain Vomiting neonate New-onset seizure Low back pain Neck mass (child and adult) Flank pain Pulsatile abdominal mass
Get Radiology Tree app to read full this article<
Course Evaluation
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Statistical Analysis
Get Radiology Tree app to read full this article<
Results
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Table 3
Selected Results from the Precourse and Postcourse Anonymous Assessment of Perceived Confidence in Knowledge of Course Material
Statement Mean precourse score Mean postcourse score_P_ ∗ I feel confident selecting the most appropriate imaging modality to investigate common emergency complaints. 1.875 3.73 <.001 I feel comfortable searching the medical literature to assist me in determining the most appropriate imaging study. 3.125 4.46 <.001 I am familiar with the radiation dose associated with the various imaging modalities. 2.7 4.21 <.001 I understand the role of diagnostic imaging in the workup of patients in the emergency department. 3.2 4.08 .002 I am aware of the indications of the various imaging modalities used in an emergent setting to investigate common emergency department complaints. 2.67 3.92 <.001 I am aware of the contraindications for various imaging modalities used in an emergent setting to investigate common emergency department complaints. 2.67 3.75 <.001 I am aware of the side effects of the various imaging modalities used in an emergent setting to investigate common emergency department complaints. 2.79 3.875 <.001 I am aware of the downstream effects of ionizing radiation of the various imaging modalities used in an emergent setting to investigate common emergency complaints. 2.75 4 <.001
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Discussion
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Appendix 1
Pre-test MCQ
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Appendix 2
Pretest survey
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
References
1. Hendee W.R., Becker G.J., Borgstede J.P., et. al.: Addressing overutilization in medical imaging. Radiology 2010; 257: pp. 240-245.
2. Dunnick N.R., Applegate K.E., Arenson R.L.: The inappropriate use of imaging studies: a report of the 2004 Intersociety Conference. J Am Coll Radiol 2005; 2: pp. 401-406.
3. Branstetter BFt, Humphrey A.L., Schumann J.B.: The long-term impact of preclinical education on medical students’ opinions about radiology. Acad Radiol 2008; 15: pp. 1331-1339.
4. Poot J.D., Hartman M.S., Daffner R.H.: Understanding the US medical school requirements and medical students’ attitudes about radiology rotations. Acad Radiol 2012; 19: pp. 369-373.
5. Gunderman R.B., Hill D.V.: Student concerns and misconceptions about a career in radiology. Acad Radiol 2012; 19: pp. 366-368.
6. Del Mar C., Glasziou P., Mayer D.: Teaching evidence based medicine. BMJ 2004; 329: pp. 989-990.
7. Erturk S.M., Ondategui-Parra S., Otero H., et. al.: Evidence-based radiology. J Am Coll Radiol 2006; 3: pp. 513-519.
8. Marshall N.L., Spooner M., Galvin P.L., et. al.: Informatics in radiology: evaluation of an e-learning platform for teaching medical students competency in ordering radiologic examinations. Radiographics 2011; 31: pp. 1463-1474.
9. Thurley P., Dennick R.: Problem-based learning and radiology. Clin Radiol 2008; 63: pp. 623-628.
10. Subramaniam R.M.: Problem-based learning: concept, theories, effectiveness and application to radiology teaching. Australas Radiol 2006; 50: pp. 339-341.
11. Cascade P.N.: Setting appropriateness guidelines for radiology. Radiology 1994; 192: pp. 50A-54A.
12. Chiunda A.B., Mohammed T.L.: Knowledge of ACR thoracic imaging Appropriateness Criteria® among trainees: one institution’s experience. Acad Radiol 2012; 19: pp. 635-639.
13. Nadgir R., Slanetz P.J.: Integrating evidence-based imaging into the radiology core clerkship: a proposed teaching tool of imaging strategies. J Am Coll Radiol 2010; 7: pp. 517-521.
14. Dillon J.E., Slanetz P.J.: Teaching evidence-based imaging in the radiology clerkship using the ACR appropriateness criteria. Acad Radiol 2010; 17: pp. 912-916.
15. Koontz N.A., Gunderman R.B.: Radiation safety and medical education: development and integration of a dedicated educational module into a radiology clerkship, outcomes assessment, and survey of medical students’ perceptions. Acad Radiol 2012; 19: pp. 491-497.
16. Branstetter B.F., Faix L.E., Humphrey A.L., et. al.: Preclinical medical student training in radiology: the effect of early exposure. AJR Am J Roentgenol 2007; 188: pp. W9-14.
17. Lynch D.C., Whitley T.W., Willis S.E.: A rationale for using synthetic designs in medical education research. Adv Health Sci Educ Theory Pract 2000; 5: pp. 93-103.
18. Hojat M., Xu G.: A visitor’s guide to effect sizes: statistical significance versus practical (clinical) importance of research findings. Adv Health Sci Educ Theory Pract 2004; 9: pp. 241-249.