Rationale and Objectives
This study aimed to assess the quality of and analyze trends among clinical indications received for emergency room radiograph studies.
Materials and Methods
Clinical indications provided by the emergency room and rapid care for consecutive chest, abdominal, and musculoskeletal radiographs were reviewed. Chart review was performed to analyze the provided indications compared to clinical information known to the ordering providers. Chest and abdominal radiograph indications were graded according to symptoms and physical examination signs and relevant past medical history. Musculoskeletal indications were graded according to symptoms, mechanism of injury, and positive physical examination findings. Each study indication was graded on a scale from 0 to 2 according to scales modified from those of prior published studies. Grades were further stratified according to ordering location, time of shift, ordering provider level, and specific anatomy involved.
Results
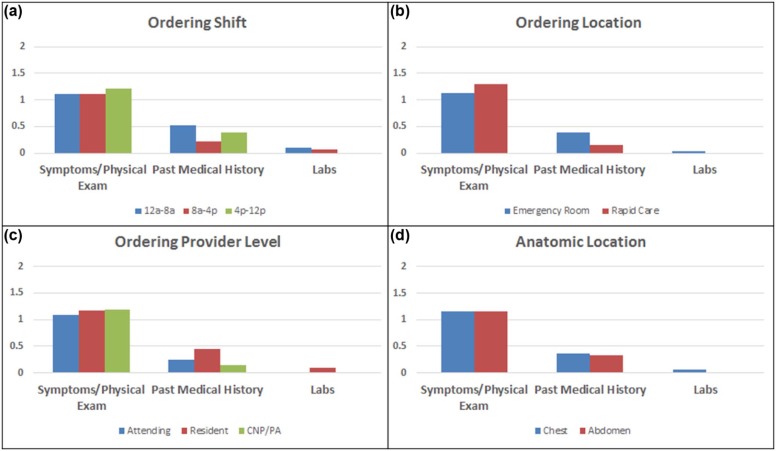
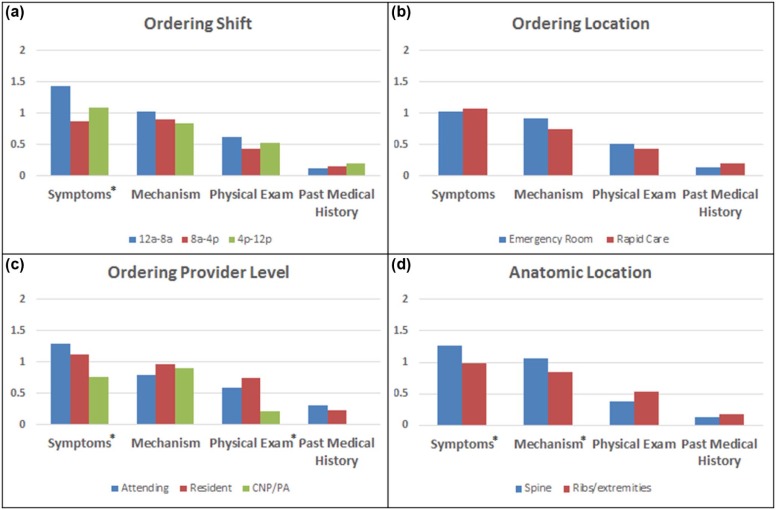
For chest and abdomen studies, mean scores for symptom and physical examination and provided past medical history grades were 1.16 and 0.36, respectively. There was a trend toward a significant difference in mean medical history grades among ordering provider levels. For musculoskeletal studies, mean scores for symptom, mechanism, and physical examination grades were 1.04, 0.89, and 0.51, respectively. Mean symptom and examination grades for physician extenders were significantly less than those of attendings and residents. Mean symptom and mechanism grades for extremity studies were significantly less than those for spinal studies.
Conclusions
For plain radiographs ordered through the emergency department, certain critical pieces of study indications tended to be underreported relative to other components. Furthermore, significant differences in select categories were seen among ordering provider levels and anatomic location.
Introduction
Incomplete and irrelevant provided histories accompanying imaging study requisitions are a prevalent problem facing many radiologists in a variety of care settings. Inadequate histories can be particularly problematic in the emergency department where the acuity of medical conditions is greater and rapid turnaround times are critical to provide optimal care.
Numerous studies have shown the importance and value that high-quality clinical histories can have on radiologists’ image interpretation across multiple modalities . Given time constraints and high volumes emergency radiologists face, obtaining relevant histories by routinely contacting clinicians or searching medical records is not feasible. Furthermore, as imaging volume through emergency departments continues to increase , radiologists will need to increasingly rely on clinical histories provided to them through study requisitions.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Materials and Methods
Get Radiology Tree app to read full this article<
Patient and Study Selection
Get Radiology Tree app to read full this article<
Assessment of Indication Quality
Get Radiology Tree app to read full this article<
Data Analysis
Get Radiology Tree app to read full this article<
Results
Get Radiology Tree app to read full this article<
Table 1
Study Characteristics
Chest and Abdomen Musculoskeletal Number of studies 218 212 Average age 54.6 47.5 Number of females (%) 120 (55%) 141 (67%) Anatomy Chest: 199
Abdomen: 19 Ribs or extremities: 169
Spine: 43 Shift 12 AM–8 AM: 52
8 AM–4 PM: 78
4 PM–12 AM: 87 12 AM–8 AM: 30
8 AM–4 PM: 99
4 PM–12 AM: 94 Patient location Emergency room: 183
Rapid care: 35 Emergency room: 173
Rapid care: 39 Provider role (no. of unique providers) Attending: 48 (15)
Resident: 133 (15)
CNP or PA: 37 (11) Attending: 56 (12)
Resident: 78 (14)
CNP or PA: 78 (10)
CNP, certified nurse practitioner; PA, physician’s assistant.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Table 2
Chest and Abdomen Variability Analysis
Symptoms and Physical Examination PMH Laboratories Inter-user 0.53 0.80 0.81 Intra-user 0.79 0.90 0.91
PMH, past medical history.
All data are listed as kappa values.
Table 3
Musculoskeletal Variability Analysis
Symptoms Mechanism Physical Examination PMH Inter-user 0.60 0.75 0.69 0.63 Intra-user 0.74 0.78 0.88 0.83
PMH, past medical history.
All data are listed as kappa values.
Get Radiology Tree app to read full this article<
Discussion
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
References
1. Doubilet P., Herman P.G.: Interpretation of radiographs: effect of clinical history. AJR Am J Roentgenol 1981; 137: pp. 1055-1058.
2. Berbaum K.S., el Khoury G.Y., Franken E.A., et. al.: Impact of clinical history on fracture detection with radiography. Radiology 1988; 168: pp. 507-511.
3. Song K.S., Song H.H., Park S.H., et. al.: Impact of clinical history on film interpretation. Yonsei Med J 1992; 33: pp. 168-172.
4. Berbaum K.S., Franken E.A., Dorfman D.D., et. al.: Influence of clinical history on perception of abnormalities in pediatric radiographs. Acad Radiol 1994; 1: pp. 217-223.
5. Leslie A., Jones A.J., Goddard P.R.: The influence of clinical information on the reporting of CT by radiologists. Br J Radiol 2000; 73: pp. 1052-1055.
6. Mullins M.E., Lev M.H., Schellingerhout D., et. al.: Influence of availability of clinical history on detection of early stroke using unenhanced CT and diffusion-weighted MR imaging. AJR Am J Roentgenol 2002; 179: pp. 223-228.
7. Levin D.C., Rao V.M., Parker L., et. al.: Continued growth in emergency department imaging is bucking the overall trends. J Am Coll Radiol 2014; 11: pp. 1044-1047.
8. Schuster D.M., Gale M.E.: The malady of incomplete, inadequate, and inaccurate radiology requisition histories: a computerized treatment. AJR Am J Roentgenol 1996; 167: pp. 855-859.
9. Gunderman R.B., Phillips M.D., Cohen M.D.: Improving clinical histories on radiology requisitions. Acad Radiol 2001; 8: pp. 299-303.
10. Alkasab T.K., Alkasab J.R., Abujudeh H.H.: Effects of a computerized provider order entry system on clinical histories provided in emergency department radiology requisitions. J Am Coll Radiol 2009; 6: pp. 194-200.
11. Pevnick J.M., Herzik A.J., Li X., et. al.: Effect of computerized physician order entry on imaging study indication. J Am Coll Radiol 2015; 12: pp. 70-74.
12. Hawkins C.M., Anton C.G., Bankes W.M., et. al.: Improving the availability of clinical history accompanying radiographic examinations in a large pediatric radiology department. AJR Am J Roentgenol 2014; 202: pp. 790-796.
13. Landis J.R., Koch G.G.: The measurement of observer agreement for categorical data. Biometrics 1977; 33: pp. 159-174.
14. Agarwal R., Bleshman M.H., Langlotz C.P.: Comparison of two methods to transmit clinical history information from referring providers to radiologists. J Am Coll Radiol 2009; 6: pp. 795-799.
15. Abujudeh H.H., Bruno M.A.: Quality and safety in radiology.2012.Oxford University Press