Rationale and Objectives
To propose grid coordinate marker placement for patients with suspicious ductogram findings occult on routine workup. To compare the success of marker placement and wire localization (WL) with ductogram-guided WL.
Materials and Methods
A retrospective search of radiology records identified all patients referred for ductography between January 2001 and May 2008. Results for 16 patients referred for ductogram-guided WL and 5 patients with grid coordinate marker placement at the time of ductography and subsequent WL were reviewed. Surgical pathology results and clinical follow-up were reviewed for concordance.
Results
Nine of 16 patients (56.3%) underwent successful ductogram-guided WL. Eight of nine patients had papillomas, one of which also had atypical ductal hyperplasia (ADH). One of nine patients had ectatic ducts with inspisated debris. Seven patients who failed ductogram-guided WL eventually underwent open surgical biopsy. Four of seven patients had papillomas, one of which also had lobular carcinoma in situ. Remaining patients had ADH (1/7) and fibrocystic changes with chronic inflammation (3/7). All five (100%) patients with grid coordinate marker placement underwent successful WL and marker excision. Pathology results included three papillomas, papillary intraductal hyperplasia, and fibrocystic change.
Conclusion
Grid coordinate marker placement at the time of abnormal ductogram provided an accurate method of localizing ductal abnormalities that are occult on routine workup, thus facilitating future WL. Marker placement obviated the need for repeat ductogram on the day of surgery and ensured surgical removal of the ductogram abnormality.
Nipple discharge is a common clinical symptom among patients presenting for diagnostic mam-mography. Although the most common cause of spontaneous nipple discharge is a solitary papilloma , approximately 10–15 % of spontaneous nipple discharge may be attributable to breast cancer . Pathologic nipple discharge is generally defined as spontaneous, unilateral single duct discharge consisting of clear, serous, serosan-guinous, or bloody fluid . Although the prevalence of cancer may be low, nipple discharge may be the only clinical symptom .
According to National Comprehensive Cancer Network (NCCN) guidelines , the standard workup for nipple discharge includes a clinical history to determine whether the discharge is pathologic and directed physical examination to evaluate for a palpable abnormality. If the nipple discharge is judged to be pathologic, a mammogram and possible ultrasound are recommended. Should imaging findings be benign, a ductogram is considered optional. Biopsy is recommended for suspicious imaging or clinical findings. Subareolar duct excision is the gold standard of care.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Materials and methods
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Ductogram Technique
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
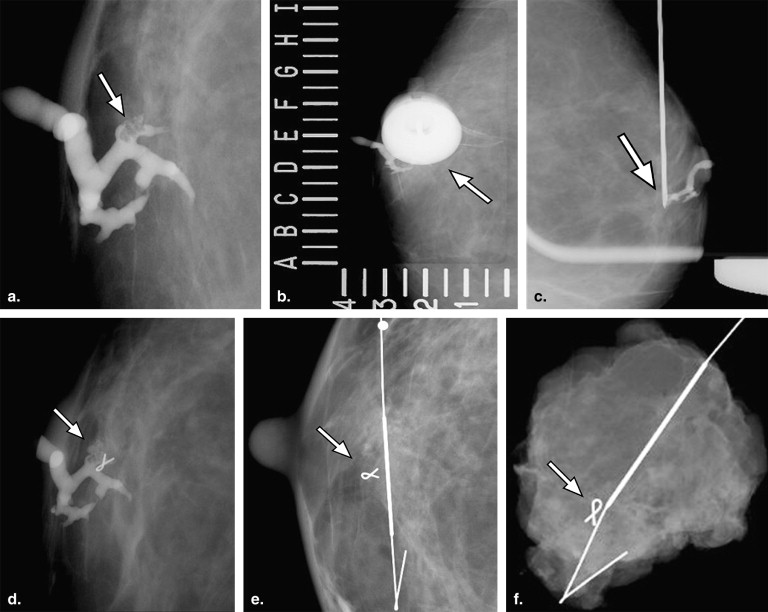
Ductogram-guided Marker Placement
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Results
Get Radiology Tree app to read full this article<
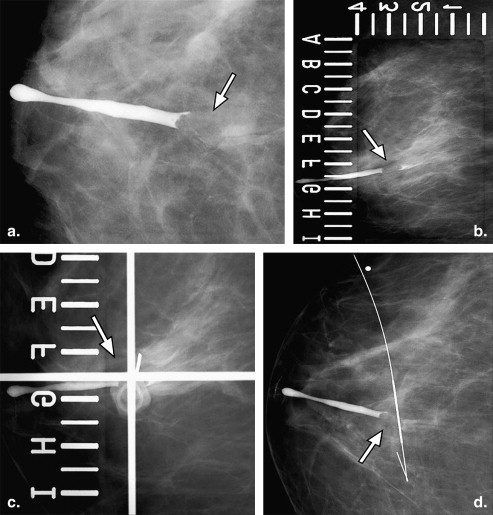
Ductogram-guided Wire Localization
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Marker Placement at Time of Ductogram
Get Radiology Tree app to read full this article<
Discussion
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
References
1. Cardenosa G., Doudna C., Eklund G.W.: Ductography of the breast: technique and findings. AJR Am J Roentgenol 1994; 162: pp. 1081-1087.
2. Dawes L.G., Bowen C., Venta L.A., et. al.: Ductography for nipple discharge: no replacement for ductal excision. Surgery 1998; 124: pp. 685-691.
3. King T.A., Carter K.M., Bolton J.S., et. al.: A simple approach to nipple discharge. Am Surg 2000; 66: pp. 960-966.
4. Simmons R., Adamovich T., Brennan M., et. al.: Nonsurgical evaluation of pathologic nipple discharge. Ann Surg Oncol 2003; 10: pp. 113-116.
5. Slawson S.H., Johnson B.A.: Ductography: how to and what if?. Radiographics 2001; 21: pp. 133-150.
6. Van Zee K.J., Ortega Perez G., Minnard E., et. al.: Preoperative galactography increases the diagnostic yield of major duct excision for nipple discharge. Cancer 1998; 82: pp. 1874-1880.
7. NCCN. The NCCN Clinical Practice Guidelines in Oncology™ Breast Cancer Screening and Diagnosis (Version 1.2010). Available online at: www.nccn.org . Accessed February 8, 2010.
8. Funovics M.A., Philipp M.O., Lackner B., et. al.: Galactography: method of choice in pathologic nipple discharge?. Eur Radiol 2003; 13: pp. 94-99.
9. Hild F., Duda V.F., Albert U., et. al.: Ductal orientated sonography improves the diagnosis of pathological nipple discharge of the female breast compared with galactography. Eur J Cancer Prev 1998; 7: pp. S57-S62.
10. Dash N., Chafin S.H., Johnson R.R., et. al.: Usefulness of tissue marker clips in patients undergoing neoadjuvant chemotherapy for breast cancer. AJR Am J Roentgenol 1999; 173: pp. 911-917.
11. Liberman L., Dershaw D.D., Morris E.A., et. al.: Clip placement after stereotactic vacuum-assisted breast biopsy. Radiology 1997; 205: pp. 417-422.
12. Patterson S.K., Joe A., Helvie M.A.: Sonographically-guided metallic marker placement at time of wire localization for intraductal or cystic lesions: a method to verify lesion retrieval. Acad Radiol 2008; 15: pp. 1316-1321.
13. Phillips S.W., Gabriel H., Comstock C.E., et. al.: Sonographically guided metallic clip placement after core needle biopsy of the breast. AJR Am J Roentgenol 2000; 175: pp. 1353-1355.
14. Baker K.S., Davey D.D., Stelling C.B.: Ductal abnormalities detected with galactography: frequency of adequate excisional biopsy. AJR Am J Roentgenol 1994; 162: pp. 821-824.
15. Cabioglu N., Hunt K.K., Singletary S.E., et. al.: Surgical decision making and factors determining a diagnosis of breast carcinoma in women presenting with nipple discharge. J Am Coll Surg 2003; 196: pp. 354-364.
16. Cardenosa G., Eklund G.W.: Benign papillary neoplasms of the breast: mammographic findings. Radiology 1991; 181: pp. 751-755.
17. Chung S.Y., Lee K.W., Park K.S., et. al.: Breast tumors associated with nipple discharge. Correlation of findings on galactography and sonography. Clin Imaging 1995; 19: pp. 165-171.
18. Morrogh M., Morris E.A., Liberman L., et. al.: The predictive value of ductography and magnetic resonance imaging in the management of nipple discharge. Ann Surg Oncol 2007; 14: pp. 3369-3377.