Rationale and Objectives
To assess the applicability of a novel macromolecular polyethylene glycol (PEG)-core gadolinium contrast agent for monitoring early antiangiogenic effects of bevacizumab using dynamic contrast-enhanced (DCE) magnetic resonance imaging (MRI).
Materials and Methods
Athymic rats ( n = 26) implanted with subcutaneous human melanoma xenografts underwent DCE-MRI at 2.0 T using two different macromolecular contrast agents. The PEG core cascade polymer PEG12,000-Gen4-(Gd-DOTA) 16 , designed for clinical development, was compared to the prototype, animal-only, macromolecular contrast medium (MMCM) albumin-(Gd-DTPA) 35 . The treatment ( n = 13) and control ( n = 13) group was imaged at baseline and 24 hours after a single dose of bevacizumab (1 mg) or saline to quantitatively assess the endothelial-surface permeability constant (K PS , μL⋅min⋅100 cm 3 ) and the fractional plasma volume (fPV,%), using a two-compartment kinetic model.
Results
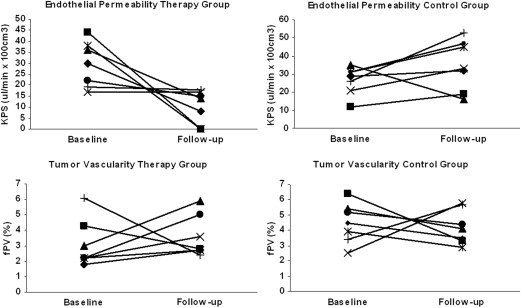
Mean K PS values, assessed with PEG12,000-Gen4-(Gd-DOTA) 16 , declined significantly ( P < .05) from 29.5 ± 10 μL⋅min⋅100 cm 3 to 10.4 ± 7.8 μL⋅min⋅100 cm 3 by 24 hours after a single dose of bevacizumab. In parallel, K PS values quantified using the prototype MMCM albumin-(Gd-DTPA) 35 showed an analogous, significant decline ( P < .05) in the therapy group. No significant effects were detected on tumor vascularity or on microcirculatory parameters in the control group between the baseline and the follow-up scan at 24 hours.
Conclusion
DCE-MRI enhanced with the novel MMCM PEG12,000-Gen4-(Gd-DOTA) 16 was able to monitor the effects of bevacizumab on melanoma xenografts within 24 hours of a single application, validated by the prototype, animal-only albumin-(Gd-DTPA) 35 . PEG12,000-Gen4-(Gd-DOTA) 16 may be a promising candidate for further clinical development as a macromolecular blood pool contrast MRI agent.
Functional and molecular imaging techniques have been examined extensively to define their potential for monitoring the tumor angiogenesis. Established morphologic assessments relying on tumor size such as Response Evaluation Criteria in Solid Tumors (RECIST) 1.1 do not have adequate sensitivity for detection of tumor responses to antiangiogenic therapy in a desirable short time period . Data indicate that magnetic resonance (MR) morphology alone, including size or contrast enhancement, will not be adequate to monitor angiogenesis treatment . Dynamic, contrast-enhanced (DCE) MR imaging (MRI) enhanced with macromolecular contrast media (MMCM) has been investigated in experimental studies for monitoring tumor angiogenesis, based on the dependence of endothelial macromolecular permeability on tissue vascular endothelial growth factor (VEGF) activity. VEGF potently increases macromolecular permeability whereas inhibition of VEGF, shown with a variety of antiangiogenesis drugs and cancer models, reduces macromolecular permeability . The range of diagnostic utility for MMCM-enhanced MRI in cancer characterization has been demonstrated in recent years using animal models and the prototypic MMCM albumin-(Gd-DTPA) 35 in differentiating benign and malignant tumors, in grading the degree of tumor aggressiveness, in detecting early responses to antiangiogenesis drug therapy, and in use as a predictive biomarker of tumor response . However, albumin-(Gd-DTPA) 35 is considered to be poorly suited for use in humans because of incomplete elimination and concerns of immunogenicity . Hence, new MMCM are being sought that have blood kinetic properties similar to albumin-(Gd-DTPA) 35 and will be appropriate for application in humans. Among currently investigated macromolecular contrast agents are polymers, dendrimers, and noncovalent complexes of small molecule agents with proteins including novel biodegradable compounds such as a polydisulfide with Gd-DOTA monoamide side chains or triazine dendrimers derivatized with a DOTA or DTPA .
The current study advances the evaluation of polyethylene glycol (PEG) core Gd macromolecular contrast agents, specifically PEG12,000-Gen4-(Gd-DOTA) 16 , representing a novel class of macromolecular contrast agents. PEG-core MMCM are designed specifically for clinical safety in humans, while meeting the physicochemical and pharmacologic requirements of contrast agents intended for quantitative MRI characterization of blood vessels . This initial experimental study was conducted to investigate the applicability of PEG12,000-Gen4-(Gd-DOTA) 16 for monitoring of antiangiogenic therapy analogous to the established prototype albumin-(Gd-DTPA) 35 .
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Materials and Methods
Animal Model
Get Radiology Tree app to read full this article<
Contrast Media
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
PEG Core MMCM Synthesis
Get Radiology Tree app to read full this article<
Dynamic MRI
Get Radiology Tree app to read full this article<
Data Analysis
Get Radiology Tree app to read full this article<
Results
Get Radiology Tree app to read full this article<
Table 1
Individual Values of K PS and fPV Quantified by DCE-MRI Enhanced With the Polymer MMCM PEG12,000-Gen4-(Gd-DOTA) 16 and the MMCM Prototype Albumin-(Gd-DTPA) 35 at Baseline and 24 Hours After a Single Intraperitoneal Injection of the Monoclonal Anti-VEGF Antibody Bevacizumab
PEG12,000-Gen4-(Gd-DOTA) 16 Therapy Control Baseline Follow-up Baseline Follow-up Tumor K PS (μL⋅min⋅100 cm 3 ) fPV (%) K PS (μL⋅min⋅100 cm 3 ) fPV (%) K PS (μL⋅min⋅100 cm 3 ) fPV (%) K PS (μL⋅min⋅100 cm 3 ) fPV (%) 1 30 1.8 8 2.7 29 4.5 32 3.5 2 44 4.3 0 2.8 118 6.4 19 3.3 3 36 3.0 14 5.9 35 5.4 15 4.1 4 17 2.2 17 3.6 21 2.5 33 5.8 5 38 2.2 0 2.7 31 3.9 45 2.9 6 22 2.2 15 5.0 31 5.1 47 4.4 7 19 6.1 18 2.4 26 3.4 53 5.7 Mean ± SD 29.5 ± 10.4 3.1 ± 1.6 10.4 ± 7.8 ∗ 3.6 ± 1.4 41 ± 34 4.5 ± 1.3 35 ± 14 4.2 ± 1.1
Albumin-(Gd-DTPA) Therapy Control Baseline Follow-up Baseline Follow-up Tumor K PS (μL⋅min⋅100 cm 3 ) fPV (%) K PS (μL⋅min⋅100 cm 3 ) fPV (%) K PS (μL⋅min⋅100 cm 3 ) fPV (%) K PS (μL⋅min⋅100 cm 3 ) fPV (%) 1 11 3.3 0 2.8 16 2.6 7 2.7 2 45 5.2 0 2.6 34 4.1 10 2.4 3 16 2.8 0 3.3 27 3.3 15 4.3 4 45 6.2 0 6.5 37 3.7 12 1.8 5 35 4.6 0 8.4 38 3.5 19 3.0 6 38 5.6 0 3.7 13 1.9 11 1.1 Mean ± SD 32 ± 15 4.6 ± 1.3 0 ∗ 4.5 ± 2.3 28 ± 11 3.2 ± 0.8 12 ± 4 2.5 ± 1
DCE, dynamic contrast-enhanced; fPV, tumor vascularity; K PS , tumor endothelial permeability; MMCM, macromolecular contrast medium; MRI, magnetic resonance imaging; PEG, poly ethylene; SD, standard deviation; VEGF, vascular endothelial growth factor.
Get Radiology Tree app to read full this article<
Table 2
Theoretical and Measured Effective MW, T1 Relaxivities, and Blood Half-Lives for PEG12,000-Gen4-(Gd-DOTA) and Albumin-(Gd-DTPA) 35
Contrast Agent Theoretical MW (kDa) Effective MW (kDa) T1 Relaxivity per Gd Ion (mM −1 •s −1 ) Blood Half-Life Mean ± SD (Minutes) PEG12,000-Gen4-(Gd-DOTA) 16 27 194 9.9 49 ± 6 Albumin-(Gd-DTPA) 35 92 180 10.4 54 ± 11
MW, molecular weight; PEG, polyethylene glycol; SD, standard deviation.
Effective molecular weights were determined by comparison to protein standards on size exclusion chromatography. T1 relaxivities were measured at 10 MHz and 37°C.
Get Radiology Tree app to read full this article<
DCE-MRI Enhanced With PEG12,000-Gen4-(Gd-DOTA) 16
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
DCE-MRI Enhanced With Albumin-(Gd-DTPA) 35
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Discussion
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Acknowledgment
Get Radiology Tree app to read full this article<
References
1. Ratain M.J., Eisen T., Stadler W.M., et. al.: Phase II placebo-controlled randomized discontinuation trial of sorafenib in patients with metastatic renal cell carcinoma. J Clin Oncol 2006; 24: pp. 2505-2512.
2. Wahl R.L., Jacene H., Kasamon Y., et. al.: From RECIST to PERCIST: evolving considerations for PET response criteria in solid tumors. J Nucl Med 2009; 50: pp. 122S-150S. 50/Suppl_1/122S [pii] 10.2967/jnumed.108.057307
3. Brasch R., Pham C., Shames D., et. al.: Assessing tumor angiogenesis using macromolecular MR imaging contrast media. J Magn Reson Imaging 1997; 7: pp. 68-74.
4. Cyran C.C., Sennino B., Chaopathomkul B., et. al.: Magnetic resonance imaging for monitoring the effects of thalidomide on experimental human breast cancers. Eur Radiol 2009; 19: pp. 121-131.
5. Fournier L.S., Novikov V., Lucidi V., et. al.: MR monitoring of cyclooxygenase-2 inhibition of angiogenesis in a human breast cancer model in rats. Radiology 2007; 243: pp. 105-111.
6. Pham C.D., Roberts T.P., van Bruggen N., et. al.: Magnetic resonance imaging detects suppression of tumor vascular permeability after administration of antibody to vascular endothelial growth factor. Cancer Invest 1998; 16: pp. 225-230.
7. Grist T.M., Korosec F.R., Peters D.C., et. al.: Steady-state and dynamic MR angiography with MS-325: initial experience in humans. Radiology 1998; 207: pp. 539-544.
8. Henderson E., Sykes J., Drost D., et. al.: Simultaneous MRI measurement of blood flow, blood volume, and capillary permeability in mammary tumors using two different contrast agents. J Magn Reson Imaging 2000; 12: pp. 991-1003.
9. Li D., Zheng J., Weinmann H.J.: Contrast-enhanced MR imaging of coronary arteries: comparison of intra- and extravascular contrast agents in swine. Radiology 2001; 218: pp. 670-678.
10. Bumb A., Brechbiel M.W., Choyke P.: Macromolecular and dendrimer-based magnetic resonance contrast agents. Acta Radiol 2010; 51: pp. 751-767.
11. Ye Z., Wu X., Tan M., et. al.: Synthesis and evaluation of a polydisulfide with Gd-DOTA monoamide side chains as a biodegradable macromolecular contrast agent for MR blood pool imaging. Contrast Media Mol Imaging 2013; 8: pp. 220-228.
12. Lim J., Turkbey B., Bernardo M., et. al.: Gadolinium MRI contrast agents based on triazine dendrimers: relaxivity and in vivo pharmacokinetics. Bioconjug Chem 2012; 23: pp. 2291-2299.
13. Raatschen H.J., Fu Y., Shames D.M., et. al.: Magnetic resonance imaging enhancement of normal tissues and tumors using macromolecular Gd-based cascade polymer contrast agents: preclinical evaluations. Invest Radiol 2006; 41: pp. 860-867.
14. Cyran C.C., Fu Y., Raatschen H.J., et. al.: New macromolecular polymeric MRI contrast agents for application in the differentiation of cancer from benign soft tissues. J Magn Reson Imaging 2008; 27: pp. 581-589.
15. Fu Y., Raatschen H.J., Nitecki D.E., et. al.: Cascade polymeric MRI contrast media derived from poly(ethylene glycol) cores: initial syntheses and characterizations. Biomacromolecules 2007; 8: pp. 1519-1529.
16. Cai J., Han S., Qing R., et. al.: In pursuit of new anti-angiogenic therapies for cancer treatment. Front Biosci 2011; 16: pp. 803-814.
17. Rose S.: FDA pulls approval for avastin in breast cancer. Cancer Discovery 2011; 1: pp. OF1-OF2.
18. Dienstmann R., Ades F., Saini K.S., et. al.: Benefit-risk assessment of bevacizumab in the treatment of breast cancer. Drug Saf 2012; 35: pp. 15-25.
19. Shames D.M., Kuwatsuru R., Vexler V., et. al.: Measurement of capillary permeability to macromolecules by dynamic magnetic resonance imaging: a quantitative noninvasive technique. Magn Reson Med 1993; 29: pp. 616-622.
20. Fu Y., Nitecki D.E., Maltby D., et. al.: Dendritic iodinated contrast agents with PEG-cores for CT imaging: synthesis and preliminary characterization. Bioconjug Chem 2006; 17: pp. 1043-1056.
21. Ogan M.D., Schmiedl U., Moseley M.E., et. al.: Albumin labeled with Gd-DTPA. An intravascular contrast-enhancing agent for magnetic resonance blood pool imaging: preparation and characterization. Invest Radiol 1987; 22: pp. 665-671.
22. Roberts T.P., Brasch R.C., Schwickert H.C., et. al.: Quantification of tissue gadolinium concentration using magnetic resonance imaging: comparison of ultrashort inversion time inversion recovery echoplanar and dynamic three-dimensional spoiled gradient-recalled approaches with in vitro measurements. Acad Radiol 1996; 3: pp. S282-S285.
23. Preda A., Turetschek K., Daldrup H., et. al.: The choice of region of interest measures in contrast-enhanced magnetic resonance image characterization of experimental breast tumors. Invest Radiol 2005; 40: pp. 349-354.
24. Stephen R.M., Gillies R.J.: Promise and progress for functional and molecular imaging of response to targeted therapies. Pharm Res 2007; 24: pp. 1172-1185.
25. Menichetti L., Manzoni L., Paduano L., et. al.: Iron oxide-gold core-shell nanoparticles as multi-modal imaging contrast agent. IEEE Sensors J 2013; 13: pp. 2305-2312.
26. Casciaro S., Soloperto G., Greco A., et. al.: Effectiveness of functionalized nanosystems for multimodal molecular sensing and imaging in medicine. IEEE Sensors J 2013; 13: pp. 2305-2312.
27. Malvindi M.A., Greco A., Conversano F., et. al.: Magnetic/silica nanocomposites as dual-mode contrast agents for combined magnetic resonance imaging and ultrasonography. Adv Funct Mater 2011; 21: pp. 2548-2555.
28. Kiessling F., Farhan N., Lichy M.P., et. al.: Dynamic contrast-enhanced magnetic resonance imaging rapidly indicates vessel regression in human squamous cell carcinomas grown in nude mice caused by VEGF receptor 2 blockade with DC101. Neoplasia 2004; 6: pp. 213-223.
29. Turetschek K., Preda A., Novikov V., et. al.: Tumor microvascular changes in antiangiogenic treatment: assessment by magnetic resonance contrast media of different molecular weights. J Magn Reson Imaging 2004; 20: pp. 138-144.
30. Cyran C.C., Paprottka P.M., Schwarz B., et. al.: Perfusion MRI for monitoring the effect of sorafenib on experimental prostate carcinoma: a validation study. AJR Am J Roentgenol 2012; 198: pp. 384-391. 198/2/384 [pii] 10.2214/AJR.11.6951
31. Afaq A., Akin O.: Imaging assessment of tumor response: past, present and future. Future Oncol 2011; 7: pp. 669-677.
32. Cyran C.C., Sennino B., Fu Y., et. al.: Permeability to macromolecular contrast media quantified by dynamic MRI correlates with tumor tissue assays of vascular endothelial growth factor (VEGF). Eur J Radiol 2012; 81: pp. 891-896.
33. Dvorak H.F., Sioussat T.M., Brown L.F., et. al.: Distribution of vascular permeability factor (vascular endothelial growth factor) in tumors: concentration in tumor blood vessels. J Exp Med 1991; 174: pp. 1275-1278.
![Figure 1, Schematic chemical structure of the polyethylene glycol (PEG) core dendrimeric contrast agent PEG12,000-Gen4-(Gd-DOTA) 16 . This new class of macromolecular contrast medium consists of a linear PEG core and two peripheral lysine-dendrimer amplifiers, which are conjugated, with multiple highly stable Gd-DOTA chelates serving as signal enhancing groups in magnetic resonance imaging. PEG12,000-Gen4-(Gd-DOTA) 16 , being extremely hydrophilic and bulky, creates a water shield around the polymer, making the effective size (molecular weight [MW] = 194 kDa) much greater than indicated by the actual MW (27 kDa).](https://storage.googleapis.com/dl.dentistrykey.com/clinical/EvaluationofaNovelMacromolecularCascadePolymerContrastMediumforDynamicContrastEnhancedMRIMonitoringofAntiangiogenicBevacizumabTherapyinaHumanMelanomaModel/0_1s20S1076633213003401.jpg)