Rationale and Objectives
The aim of this study was to evaluate the usefulness of computer-aided diagnosis (CAD) software for the detection of lung nodules on multidetector-row computed tomography (MDCT) in terms of improvement in radiologists’ diagnostic accuracy in detecting lung nodules, using jackknife free-response receiver-operating characteristic (JAFROC) analysis.
Materials and Methods
Twenty-one patients (6 without and 15 with lung nodules) were selected randomly from 120 consecutive thoracic computed tomographic examinations. The gold standard for the presence or absence of nodules in the observer study was determined by consensus of two radiologists. Six expert radiologists participated in a free-response receiver operating characteristic study for the detection of lung nodules on MDCT, in which cases were interpreted first without and then with the output of CAD software. Radiologists were asked to indicate the locations of lung nodule candidates on the monitor with their confidence ratings for the presence of lung nodules.
Results
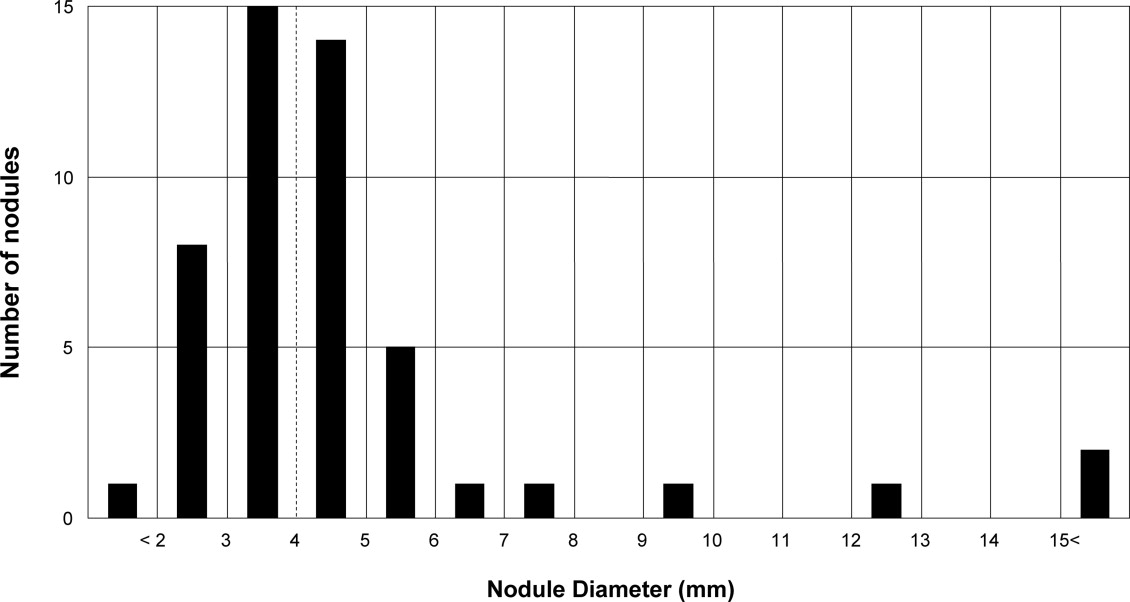
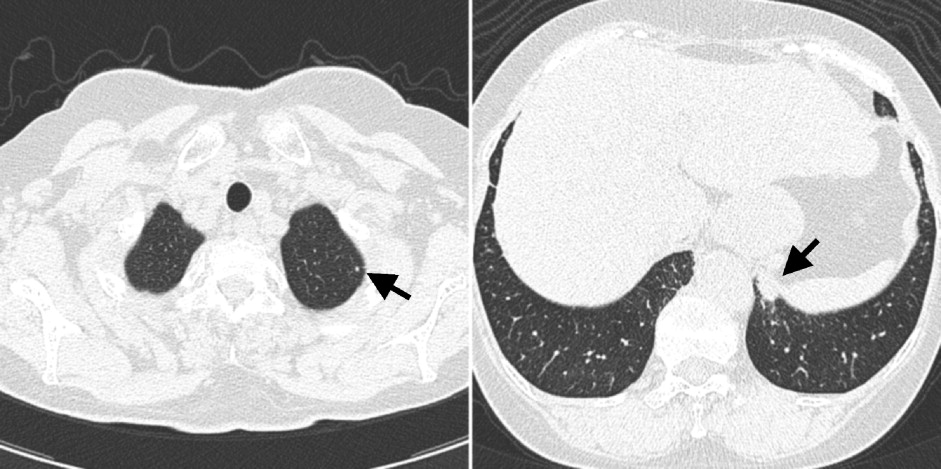
The performance of the CAD software indicated that the sensitivity in detecting lung nodules was 71.4%, with 0.95 false-positive results per case. When radiologists used the CAD software, the average sensitivity improved from 39.5% to 81.0%, with an increase in the average number of false-positive results from 0.14 to 0.89 per case. The average figure-of-merit values for the six radiologists were 0.390 without and 0.845 with the output of the CAD software, and there was a statistically significant difference ( P < .0001) using the JAFROC analysis.
Conclusion
The CAD software for the detection of lung nodules on MDCT has the potential to assist radiologists by increasing their accuracy.
Because some evidence suggests that the early detection of lung cancer may allow timely therapeutic intervention and thus favorable prognoses for patients ( ), lung cancer screening using low-dose computed tomography has been proposed ( ). For example, in a 2006 report by the International Early Lung Cancer Action Program ( ), computed tomographic (CT) lung cancer screening resulted in diagnoses of lung cancer in 484 of 31,567 participants. Of these 484 participants, 412 (85%) had clinical stage I lung cancer, and the estimated 10-year survival rate was 88% in this subgroup. Among the 484 participants, 302 had clinical stage I cancer and underwent surgical resection within 1 month after diagnosis. Their survival rate was 92%.
The development of multidetector-row computed tomography (MDCT) has made it easier to cover the whole lung with thin-section images. In addition, it has become possible to obtain isotropic voxel data, which can be useful in the observation of lesions and/or vessels from multiple directions. As a result, more than 300 images with thin-section thickness in millimeters per thoracic CT examination are reconstructed for radiologists’ routine work.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Materials and methods
Get Radiology Tree app to read full this article<
Image Database
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
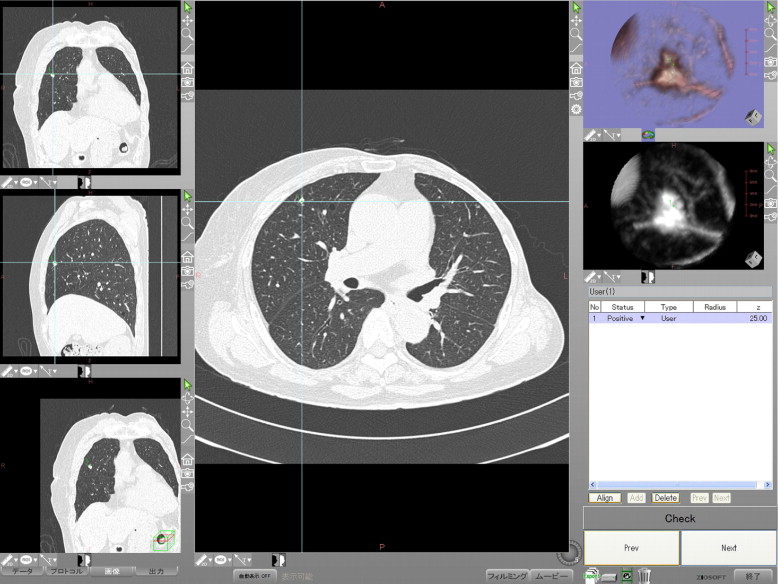
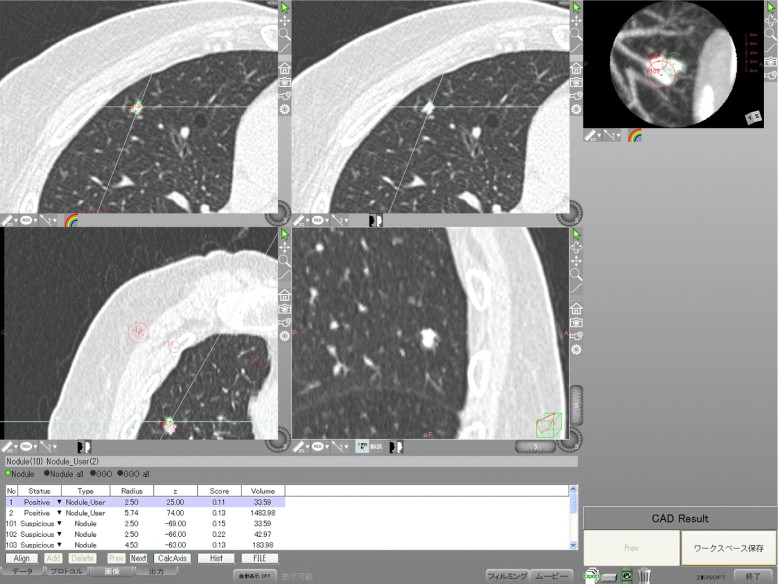
CAD Software
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Observer Study
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Results
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Table 1
FOM Values Obtained from JAFROC Analysis (Method 2) without and with Output of the CAD Software for the Six Radiologists
Reader Without CAD With CAD Sensitivity FP Results/Case FOM Sensitivity FP Results/Case FOM 1 24.5% 0.10 0.236 75.5% 0.90 0.808 2 30.6% 0.14 0.312 75.5% 1.00 0.792 3 59.2% 0.24 0.563 85.7% 1.10 0.870 4 40.8% 0.19 0.433 79.6% 0.52 0.819 5 38.8% 0.05 0.364 85.7% 0.95 0.881 6 42.9% 0.14 0.434 83.7% 0.86 0.901 Average 39.5% 0.14 0.390 ⁎ 81.0% 0.89 0.845 ⁎
CAD, computer-aided diagnosis; FOM, figure-of-merit; FP, false-positive; JAFROC, jackknife free-response receiver operating characteristic.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Discussion
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Acknowledgment
Get Radiology Tree app to read full this article<
References
1. Heelan R.T., Flehinger B.J., Melamed M.R., et. al.: Non-small-cell lung cancer: results of the New York screening program. Radiology 1984; 151: pp. 289-293.
2. Sone S., Takashima S., Li F., et. al.: Mass screening for lung cancer with mobile spiral computed tomography scanner. Lancet 1998; 351: pp. 1242-1245.
3. Flehinger B.J., Kimmel M., Melamed M.R.: The effect of surgical treatment on survival from early lung cancer. Chest 1992; 101: pp. 1013-1018.
4. Sobue T., Suzuki T., Matsuda M., Kuroishi T., Ikeda S., Naruke T.: Survival for clinical stage I lung cancer not surgically treated. Cancer 1992; 69: pp. 685-692.
5. Miettinen O.S.: Screening for lung cancer. Radiol Clin North Am 2000; 38: pp. 479-486.
6. Muhm J.R., Miller W.E., Fontana R.S., Sanderson D.R., Uhlenhopp M.A.: Lung cancer detected during a screening program using four-month chest radiographs. Radiology 1983; 148: pp. 609-615.
7. Henschke C.I., McCauley D.I., Yankelevitz D.F., et. al.: Early Lung Cancer Action Project: overall design and findings from baseline screening. Lancet 1999; 354: pp. 99-105.
8. Austin J.H., Romney B.M., Goldsmith L.S.: Missed bronchogenic carcinoma: radiographic findings in 27 patients with a potentially resectable lesion evident in retrospect. Radiology 1992; 182: pp. 115-122.
9. Henschke C.I., Yankelevitz D.F., Libby D.M., et. al.: Survival of patients with stage I lung cancer detected on CT screening. N Engl J Med 2006; 355: pp. 1763-1771.
10. Giger M.L., Bae K.T., MacMahon H.: Computerized detection of pulmonary nodules in computed tomography images. Invest Radiol 1994; 29: pp. 459-465.
11. Lee Y., Hara T., Fujita H., Itoh S., Ishigaki T.: Automated detection of pulmonary nodules in helical CT images based on an improved template-matching technique. IEEE Trans Med Imaging 2001; 20: pp. 595-604.
12. Armato S.G., Giger M.L., Moran C.J., Blackburn J.T., Doi K., MacMahon H.: Computerized detection of pulmonary nodules on CT scans. RadioGraphics 1999; 19: pp. 1303-1311.
13. Armato S.G., Giger M.L., MacMahon H.: Automated detection of lung nodules in CT scans: preliminary results. Med Phys 2001; 28: pp. 1552-1561.
14. Gurcan M.N., Sahiner B., Petrick N., et. al.: Lung nodule detection on thoracic computed tomography images: preliminary evaluation of a computer-aided diagnosis system. Med Phys 2002; 29: pp. 2552-2558.
15. Wormanns D., Fiebich M., Saidi M., Diederich S., Heindel W.: Automatic detection of pulmonary nodules at spiral CT: clinical application of a computer-aided diagnosis system. Eur Radiol 2002; 12: pp. 1052-1057.
16. Arimura H., Katsuragawa S., Suzuki K., et. al.: Computerized scheme for automated detection of lung nodules in low-dose computed tomography images for lung cancer screening. Acad Radiol 2004; 11: pp. 617-629.
17. Awai K., Murao K., Ozawa A., et. al.: Pulmonary nodules at chest CT: effect of computer-aided diagnosis on radiologists’ detection performance. Radiology 2004; 230: pp. 347-352.
18. Wormanns D., Beyer F., Diederich S., Ludwig K., Heindel W.: Diagnostic performance of a commercially available computer-aided diagnosis system for automatic detection of pulmonary nodules: comparison with single and double reading. Rofo 2004; 176: pp. 953-958.
19. Chakraborty D.P., Berbaum K.S.: Observer studies involving detection and localization: modeling, analysis, and validation. Med Phys 2004; 31: pp. 2313-2330.
20. Chakraborty D.P.: Analysis of location specific observer performance data: validated extensions of the jackknife free-response (JAFROC) method. Acad Radiol 2006; 13: pp. 1187-1193.
21. Chakraborty D.P.: Maximum likelihood analysis of free-response receiver operating characteristic (FROC) data. Med Phys 1989; 16: pp. 561-568.
22. Wagner R.F., Metz C.E., Campbell G.: Assessment of medical imaging systems and computer aids: a tutorial review. Acad Radiol 2007; 14: pp. 723-748.
23. Yuan R., Vos P.M., Cooperberg P.L.: Computer-aided detection in screening CT for pulmonary nodules. AJR Am J Roentgenol 2006; 186: pp. 1280-1287.
24. Das M., Muhlenbruch G., Mahnken A.H., et. al.: Small pulmonary nodules: effect of two computer-aided detection systems on radiologist performance. Radiology 2006; 241: pp. 564-571.
25. Bae K.T., Kim J.S., Na Y.H., Kim K.G., Kim J.H.: Pulmonary nodules: automated detection on CT images with morphologic matching algorithm—preliminary results. Radiology 2005; 236: pp. 286-293.
26. MacMahon H., Austin J.H., Gamsu G., et. al.: Guidelines for management of small pulmonary nodules detected on CT scans: a statement from the Fleischner Society. Radiology 2005; 237: pp. 395-400.