Rationale and Objectives
The aims of this study were to determine the feasibility of diffusion-weighted magnetic resonance imaging (DWI) in the detection of bowel inflammation and to investigate the changes in apparent diffusion coefficient (ADC) values in the inflamed bowel in patients with Crohn’s disease.
Materials and Methods
Eleven patients who underwent magnetic resonance enterography (including DWI) for Crohn’s disease and colonoscopy or surgery within 4 weeks of examination were recruited. Two radiologists reviewed diffusion-weighted images and ADC maps to evaluate for inflammation in each bowel segment (terminal ileum, cecum, ascending colon, transverse colon, descending colon, and rectosigmoid colon) and measured the ADC values of each bowel segment. Endoscopic and pathologic results were correlated with DWI findings.
Results
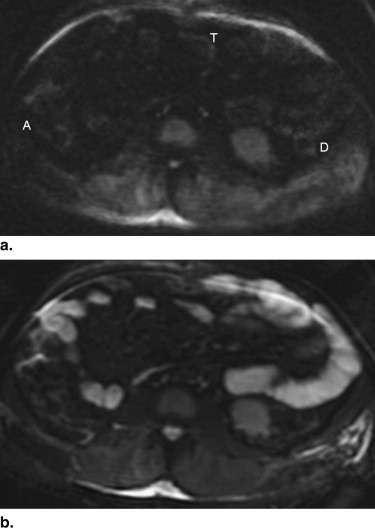
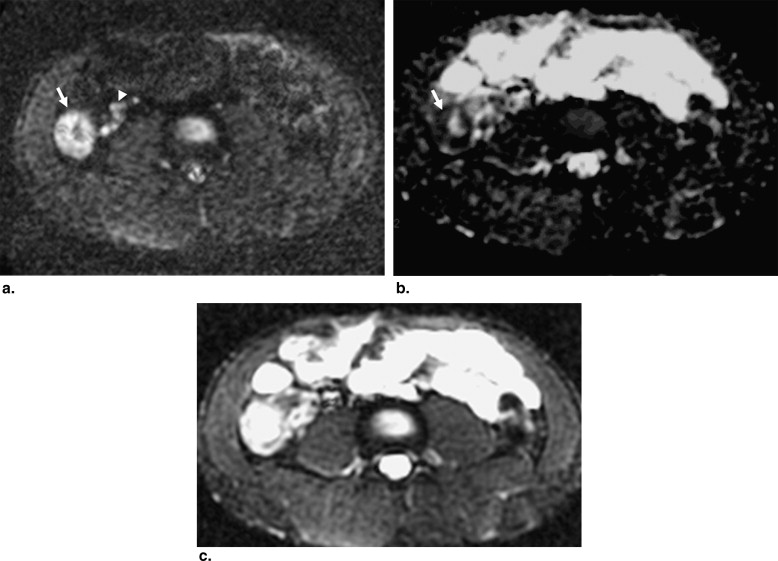
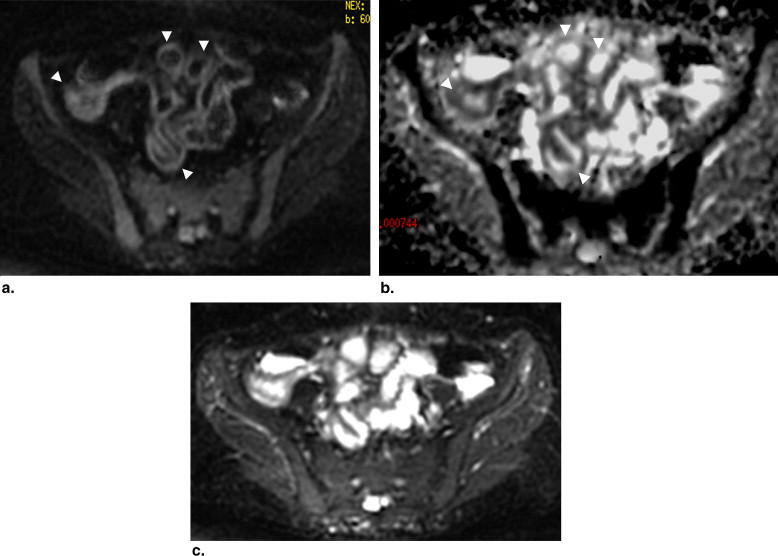
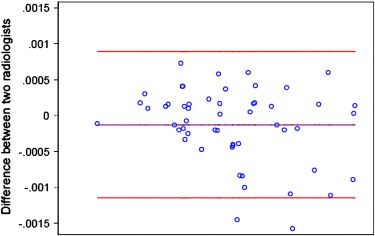
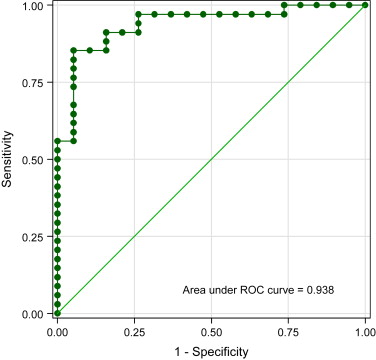
Fifty-three segments (19 with inflammation, 34 normal) were included. DWI detected inflammation in 18 of 19 segments (94.7%) and showed normal results in 28 of 34 segments (82.4%). On diffusion-weighted images, bowel segments with inflammation revealed higher signal compared to normal segments. Artifact levels were none or minimal in 10 of 11 patients (90.9%) and moderate in one patient. On quantitative analysis, ADC values of inflamed and normal bowel were measured as 0.47 − 2.60 × 10 −3 and 1.39 − 4.03 × 10 −3 mm 2 /s, respectively ( P < .05).
Conclusion
DWI with parallel imaging is a feasible technique for the detection of inflammation in patients with Crohn’s disease. ADC values are decreased in inflamed bowel segments, indicating restricted diffusion.
Magnetic resonance (MR) imaging has been increasingly used for the diagnosis and follow-up of patients with inflammatory bowel disease. Its lack of ionizing radiation, excellent soft-tissue contrast resolution, and potential to perform real-time and functional imaging are the important advantages of MR imaging that make it well suited for imaging the gastrointestinal tract . Currently, evaluation of the bowel wall by MR imaging is based on its signal on T2-weighted images, thickness, and the degree of contrast enhancement . Although the results of MR imaging using these criteria are promising, several clinically important issues, such as the accurate estimation of the extent of disease, reliable differentiation between chronic and active inflammation, and monitoring response to treatment, remain as diagnostic challenges.
A new possibility to expand the capability of MR imaging is to apply new MR applications that can give additional information about the structural organization of tissues on bowel imaging. Diffusion-weighted imaging (DWI) reflects the changes in the water mobility caused by interactions with cell membranes, macromolecules, and alterations of the tissue environment. DWI has been widely used for intracranial diseases but has only recently been applied to the abdomen. Initial results suggest that it can be useful for the evaluation of various hepatic, renal, and pancreatic diseases . The available published descriptions of DWI for the evaluation of the bowel are focused on the detection of colorectal cancer . To our knowledge, the use of DWI for the detection of bowel wall inflammation and its associated features has not been previously described.
Get Radiology Tree app to read full this article<
Materials and methods
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
MR Imaging Protocol
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Image Analysis
Get Radiology Tree app to read full this article<
Qualitative Analysis
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Quantitative Analysis
Get Radiology Tree app to read full this article<
Endoscopic and Surgical Findings
Get Radiology Tree app to read full this article<
Statistical Analysis
Get Radiology Tree app to read full this article<
Results
Get Radiology Tree app to read full this article<
Table 1
Disease Activity by Endoscopy or Surgery, Inflammation Grading Score on a per Segment Basis, and Artifact Level
Patient Terminal Ileum Cecum Ascending Colon Transverse Colon Descending Colon Rectosigmoid Colon 1 N/A N/A N/A N/A Inf (3) Inf (1) 2 N/A N/A N/A N/A N/A N (1) 3 N (1) Inf (2) Inf (2) N (2) Inf (3) Inf (2) 4 N (1) Inf (3) Inf (3) Inf (2) Inf (3) Inf (2) 5 N (1) N (1) N (1) Inf (3) Inf (3) Inf (2) 6 Inf (2) X X N (2) N (2) N (2) 7 N N N N N N 8 Inf N N N N N 9 N N N N N N 10 Inf X N N N N 11 N/A Inf Inf N N N
Inf, inflamed segment; N, normal segment; N/A, segment could not be evaluated by colonoscopy; X, segment was previously excised.
Numbers in parenthesis are artifact level grading scores: 0 = no artifacts, 1 = minimal artifacts (no significant impact on evaluation), 2 = moderate artifacts (significant impact on evaluation), and 3 = severe artifacts (nondiagnostic).
Get Radiology Tree app to read full this article<
Qualitative Evaluation
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Quantitative Analysis
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Discussion
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
References
1. Fidler J.: MR imaging of the small bowel. Radiol Clin North Am 2007; 45: pp. 317-331.
2. Taouli B., Tolia A.J., Losada M., et. al.: Diffusion-weighted MRI for quantification of liver fibrosis: preliminary experience. AJR Am J Roentgenol 2007; 189: pp. 799-806.
3. Matsuki M., Inada Y., Nakai G., et. al.: Diffusion-weighed MR imaging of pancreatic carcinoma. Abdom Imaging 2007; 32: pp. 481-483.
4. Zhang J., Tehrani Y.M., Wang L., Ishill N.M., Schwartz L.H., Hricak H.: Renal masses: characterization with diffusion-weighted MR imaging—a preliminary experience. Radiology 2008; 247: pp. 458-464.
5. Ichikawa T., Erturk S.M., Motosugi U., et. al.: High-B-value diffusion-weighted MRI in colorectal cancer. AJR Am J Roentgenol 2006; 187: pp. 181-184.
6. Nasu K., Kuroki Y., Kuroki S., Murakami K., Nawano S., Moriyama N.: Diffusion-weighted single shot echo planar imaging of colorectal cancer using a sensitivity-encoding technique. Jpn J Clin Oncol 2004; 34: pp. 620-626.
7. Hosonuma T., Tozaki M., Ichiba N., et. al.: Clinical usefulness of diffusion-weighted imaging using low and high b-values to detect rectal cancer. Magn Reson Med Sci 2006; 5: pp. 173-177.
8. Jaggi R.S., Husain M., Chawla S., Gupta A., Gupta R.K.: Diagnosis of bacterial cerebellitis; diffusion imaging and proton magnetic resonance spectroscopy. Pediatr Neurol 2005; 32: pp. 72-74.
9. Kiroglu Y., Calli C., Yunten N., et. al.: Diffusion-weighted MR imaging of viral encephalitis. Neuroradiology 2006; 48: pp. 875-880.
10. Verswijvel G., Vandecaveye V., Gelin G., et. al.: Diffusion-weighted MR imaging in the evaluation of renal infection: preliminary results. JBR-BTR 2002; 85: pp. 100-103.
11. Riddell R.H.: Pathology of idiopathic inflammatory bowel disease.Kirsner J.B.Inflammatory bowel disease.2000.W.B. SaundersPhiladephia, PA:pp. 427-452.
12. Sostegni R., Daperno M., Scaglione N., Lavagna A., Rocca R., Pera A.: Review article: Crohn’s disease: monitoring disease activity. Aliment Pharmacol Ther 2003; 17: pp. 11-17.
13. Koh D., Collins D.J.: Diffusion-weighted MRI in the body: applications and challenges in oncology. AJR Am J Roentgenol 2007; 188: pp. 1622-1635.
14. Takahara T., Imai Y., Yamashita T., et. al.: Diffusion weighted whole body imaging with background body signal suppression (DWIBS): technical improvement using free breathing, STIR and high resolution 3D display. Radiat Med 2004; 22: pp. 275-282.