Rationale and Objectives
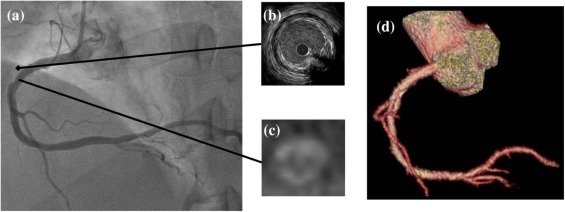
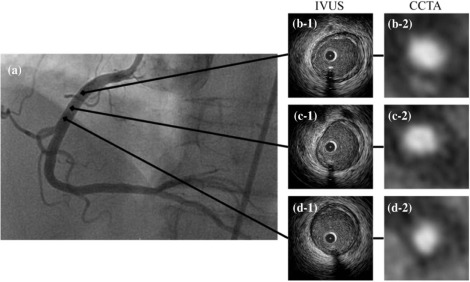
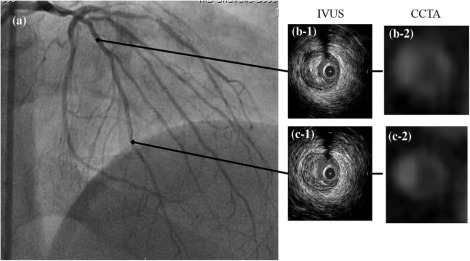
Although intravascular ultrasound (IVUS) is the current gold standard for plaque characterization, noninvasive coronary computed tomographic angiography (CCTA) requires further evaluation. The ability to detect plaque morphology by CCTA remains unclear. The purpose of this study was to evaluate the diagnostic accuracy of CCTA for plaque detection and morphology.
Materials and Methods
Thirty-one patients underwent cardiac catheterization with IVUS and CCTA. The presence of plaque was evaluated by both modalities in nonocclusive segments (<50% stenosis) of the left anterior descending artery, left circumflex artery, and right coronary artery. Plaque morphology was classified as (1) normal, (2) soft or fibrous, (3) fibrocalcific, or (4) calcific. Results by IVUS and CCTA were compared blindly on a segment-to-segment basis with subgroup analysis based on CCTA tube voltage.
Results
Among the 31 patients (mean age 56.2 ± 8.6 years, 27% female), 152 segments were analyzed. Of these segments, 42% were in the left anterior descending artery, 32% were in the left circumflex artery, and 26% were in the right coronary artery. Plaque morphology by IVUS identified 103 segments as fibrous (68%), 31 as fibrocalcific (20%), and 6 as calcific (4.0%); 12 segments were normal (8.0%). To evaluate for the presence of plaque, CCTA had an overall sensitivity and specificity of 99% and 75%, respectively. In patients who underwent CCTA with a tube voltage of 100 kV, both sensitivity and specificity were 100%. The sensitivity and specificity of CCTA to identify plaque as calcified (fibrocalcific or calcific) vs noncalcified (soft or fibrous) were 87% and 96%, respectively. Overall, the accuracy of CCTA to detect the presence of plaque was 97%; the accuracy to detect plaque calcification was 94%.
Conclusions
CCTA offers excellent sensitivity and accuracy for plaque detection and morphology characterization in nonocclusive coronary segments. In addition, diagnostic accuracy is preserved with a reduced tube voltage protocol.
Introduction
Coronary computed tomographic angiography (CCTA) offers a noninvasive, anatomically based approach for the accurate assessment of coronary artery disease. Previous studies have already established coronary artery calcium as a surrogate for plaque burden and a predictor of future coronary events among a variety of populations in the United States . More than two-thirds of myocardial infarctions are now estimated to occur in coronary arteries with only moderate stenosis . There is also evidence that nonobstructive plaques play an important role in death . Therefore, focus has deservedly turned to the use and validation of CCTA to identify the presence of nonobstructive plaque and to characterize plaque type.
Intravascular ultrasound (IVUS) is the current gold standard for the assessment of coronary plaque morphology. Although invasive, IVUS provides superior plaque characterization and more accurate quantification of plaque burden compared to traditional coronary angiography. However, recent studies also indicate that CCTA can accurately assess plaque morphology in both obstructive and nonobstructive coronary segments . With this growing role, CCTA may be able to noninvasively detect “at-risk” or vulnerable plaques in nonobstructive coronary segments before the patient develops symptomatic disease in the form of myocardial infarction or sudden cardiac death. Moreover, lower-voltage CCTA protocols, which offer improved signal- and contrast-to-noise ratios, may enhance diagnostic accuracy for the detection of coronary plaque and plaque morphology with the added benefit of reduced radiation exposure to the patient .
Get Radiology Tree app to read full this article<
Materials and Methods
Get Radiology Tree app to read full this article<
Study Population
Get Radiology Tree app to read full this article<
Coronary Computed Tomographic Angiography
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Conventional ICA and IVUS
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Statistical Analyses
Get Radiology Tree app to read full this article<
Results
Get Radiology Tree app to read full this article<
Table 1
Plaque Morphology by CCTA and IVUS
Segment Classification
( n = 152) Imaging Method CCTA IVUS Normal 10 12 Plaque Soft or fibrous 106 103 Fibrocalcific 30 31 Calcific 6 6
CCTA, computed tomographic angiography; IVUS, intravenous ultrasound.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Table 2
Sensitivity, Specificity, and Overall Accuracy of CCTA in the Detection of Plaque and Plaque Calcification Compared to IVUS
Normal vs Plaque Noncalcified vs Calcified Plaque Sensitivity (%) 99 (139/140) 87 (32/37) Specificity (%) 75 (9/12) 96 (99/103) Overall accuracy (%) 97 (148/152) 94 (131/140)
CCTA, computed tomographic angiography; IVUS, intravenous ultrasound.
Table 3
Statistical Comparison of CCTA Based on Tube Voltage Protocol
Tube Voltage 120 kV 100 kV Normal vs plaque Sensitivity (%) 99 (93/94) 100 (46/46) Specificity (%) 63 (5/8) 100 (4/4) Overall accuracy (%) 96 (98/102) 100 (50/50) Noncalcified vs calcified plaque Sensitivity (%) 89 (23/26) 82 (9/11) Specificity (%) 94 (64/68) 100 (35/35) Overall accuracy (%) 93 (87/94) 96 (44/46)
CCTA, computed tomographic angiography.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Table 4
Hounsfield Unit Measurements Based on Tube Voltage Protocol and Plaque Type
Combined Group 120-kV Group 100-kV Group Fibrous or soft 102 ± 78 \* 114 ± 78 \* 80 ± 58 \* Fibrocalcific 331 ± 99 335 ± 99 309 ± 103 Calcific 944 ± 440 466 ± 440 1183 ± 343
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Discussion
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Study Limitations
Get Radiology Tree app to read full this article<
Conclusions
Get Radiology Tree app to read full this article<
Acknowledgment
Get Radiology Tree app to read full this article<
References
1. Detrano R., Guerci A.D., Carr J.J., et. al.: Coronary calcium as a predictor of coronary events in four racial or ethnic groups. N Engl J Med 2008; 358: pp. 1336-1345.
2. Budoff M.J., Shaw L.J., Liu S.T., et. al.: Long-term prognosis associated with coronary calcification: observations from a registry of 25,253 patients. J Am Coll Cardiol 2007; 49: pp. 1860-1870.
3. Libby P.: Coronary artery injury and the biology of atherosclerosis: inflammation, thrombosis, and stabilization. Am J Cardiol 2000; 86: pp. 3J-8J. discussion 8J–9J
4. Libby P., Ridker P.M., Maseri A.: Inflammation and atherosclerosis. Circulation 2002; 105: pp. 1135-1143.
5. Lin F.Y., Shaw L.J., Dunning A.M., et. al.: Mortality risk in symptomatic patients with nonobstructive coronary artery disease: a prospective 2-center study of 2,583 patients undergoing 64-detector row coronary computed tomographic angiography. J Am Coll Cardiol 2011; 58: pp. 510-519.
6. Leber A.W., Becker A., Knez A., et. al.: Accuracy of 64-slice computed tomography to classify and quantify plaque volumes in the proximal coronary system: a comparative study using intravascular ultrasound. J Am Coll Cardiol 2006; 47: pp. 672-677.
7. Voros S., Rinehart S., Qian Z., et. al.: Prospective validation of standardized, 3-dimensional, quantitative coronary computed tomographic plaque measurements using radiofrequency backscatter intravascular ultrasound as reference standard in intermediate coronary arterial lesions: results from the ATLANTA (assessment of tissue characteristics, lesion morphology, and hemodynamics by angiography with fractional flow reserve, intravascular ultrasound and virtual histology, and noninvasive computed tomography in atherosclerotic plaques) I study. JACC Cardiovasc Interv 2011; 4: pp. 198-208.
8. Voros S., Rinehart S., Qian Z., et. al.: Coronary atherosclerosis imaging by coronary CT angiography: current status, correlation with intravascular interrogation and meta-analysis. JACC Cardiovasc Imaging 2011; 4: pp. 537-548.
9. Gopal A., Mao S.S., Karlsberg D., et. al.: Radiation reduction with prospective ECG-triggering acquisition using 64-multidetector Computed Tomographic angiography. Int J Cardiovasc Imaging 2009; 25: pp. 405-416.
10. Bischoff B., Hein F., Meyer T., et. al.: Impact of a reduced tube voltage on CT angiography and radiation dose: results of the PROTECTION I study. JACC Cardiovasc Imaging 2009; 2: pp. 940-946.
11. Gopal A., Mao S.S., Karlsberg D., et. al.: Radiation reduction with prospective ECG-triggering acquisition using 64-multidetector computed tomographic angiography. Int J Cardiovasc Imaging 2009; 25: pp. 405-416.
12. Bischoff B., Hein F., Meyer T., et. al.: Impact of a reduced tube voltage on CT angiography and radiation dose: results of the PROTECTION I study. JACC Cardiovasc Imaging 2009; 2: pp. 940-946.
13. Kitagawa T., Yamamoto H., Ohhashi N., et. al.: Comprehensive evaluation of noncalcified coronary plaque characteristics detected using 64-slice computed tomography in patients with proven or suspected coronary artery disease. Am Heart J 2007; 154: pp. 1191-1198.
14. Mintz G.S., Nissen S.E., Anderson W.D., et. al.: American College of Cardiology Clinical Expert Consensus Document on Standards for Acquisition, measurement and reporting of Intravascular Ultrasound Studies (IVUS). A report of the American College of Cardiology Task Force on Clinical Expert Consensus Documents. J Am Coll Cardiol 2001; 37: pp. 1478-1492.
15. Mintz G.S., Garcia-Garcia H.M., Nicholls S.J., et. al.: Clinical expert consensus document on standards for acquisition, measurement and reporting of intravascular ultrasound regression/progression studies. EuroIntervention 2011; 6: pp. 1123-1130. 9
16. Fuster V., Moreno P.R., Fayad Z.A., et. al.: Atherothrombosis and high-risk plaque: part I: evolving concepts. J Am Coll Cardiol 2005; 46: pp. 937-954.
17. Leber A.W., Knez A., von Ziegler F., et. al.: Quantification of obstructive and nonobstructive coronary lesions by 64-slice computed tomography: a comparative study with quantitative coronary angiography and intravascular ultrasound. J Am Coll Cardiol 2005; 46: pp. 147-154.
18. Achenbach S., Moselewski F., Ropers D., et. al.: Detection of calcified and noncalcified coronary atherosclerotic plaque by contrast-enhanced, submillimeter multidetector spiral computed tomography: a segment-based comparison with intravascular ultrasound. Circulation 2004; 109: pp. 14-17.
19. Kitagawa T., Yamamoto H., Ohhashi N., et. al.: Comprehensive evaluation of noncalcified coronary plaque characteristics detected using 64-slice computed tomography in patients with proven or suspected coronary artery disease. Am Heart J 2007; 154: pp. 1191-1198.
20. Pundziute G., Schuijf J.D., Jukema J.W., et. al.: Head-to-head comparison of coronary plaque evaluation between multislice computed tomography and intravascular ultrasound radiofrequency data analysis. JACC Cardiovasc Interv 2008; 1: pp. 176-182.
21. Caussin C., Larchez C., Ghostine S., et. al.: Comparison of coronary minimal lumen area quantification by sixty-four-slice computed tomography versus intravascular ultrasound for intermediate stenosis. Am J Cardiol 2006; 98: pp. 871-876.
22. Inoue K., Motoyama S., Sarai M., et. al.: Serial coronary CT angiography-verified changes in plaque characteristics as an end point: evaluation of effect of statin intervention. JACC Cardiovasc Imaging 2010; 3: pp. 691-698.
23. Zeb I., Li D., Nasir K., et. al.: Effect of statin treatment on coronary plaque progression—a serial coronary CT angiography study. Atherosclerosis 2013; 231: pp. 198-204.
24. Matsumoto S., Nakanishi R., Li D., et. al.: Aged garlic extract reduces low attenuation plaque in coronary arteries of patients with metabolic syndrome in a prospective randomized double-blind study. J Nutr 2016; 146: 427S–32S
25. Lijmer J.G., Mol B.W., Heisterkamp S., et. al.: Empirical evidence of design-related bias in studies of diagnostic tests. JAMA 1999; 282: pp. 1061-1066.
26. Zhao X.Q., Yuan C., Hatsukami T.S., et. al.: Effects of prolonged intensive lipid-lowering therapy on the characteristics of carotid atherosclerotic plaques in vivo by MRI: a case-control study. Arterioscler Thromb Vasc Biol 2001; 21: pp. 1623-1629.
27. Crisby M., Nordin-Fredriksson G., Shah P.K., et. al.: Pravastatin treatment increases collagen content and decreases lipid content, inflammation, metalloproteinases, and cell death in human carotid plaques: implications for plaque stabilization. Circulation 2001; 103: pp. 926-933.