Rationale and Objectives
This study aimed to determine frequency of discordant lesions and discordant false-negative cancers at stereotactic vacuum-assisted biopsy (SVAB).
Materials and Methods
Institutional database was searched for discordant SVAB results between January 1, 2005 and December 31, 2012, in this retrospective institutional review board-approved Health Insurance Portability and Accountability Act-compliant study. Patient age, indication for initial mammogram, breast density, lesion size, Breast Imaging Reporting and Data System categorization, operator experience, biopsy needle gauge, biopsy histology, and final surgical histology of discordant lesions were collected and entered into a Microsoft Excel spreadsheet. Discordant rate and false-negative rates were calculated. Fisher exact test was used to assess prevalence of discordance using 11-Gauge needles versus 9-Gauge needles. Patient age, lesion Breast Imaging Reporting and Data System, operator days of experience, mammographic density, and lesion size were evaluated for association with false-negative discordant lesions using an exact Mann-Whitney U test.
Results
A total of 1861 SVABs were performed, 224 (12%) with an 11-Gauge VAB device and 1637 (88%) with a 9G Suros or Eviva device. Majority (1409 of 1861; 76%) of SVABs targeted calcifications. Twenty-three of 1861 (1.2%) discordant lesions were identified in 23 women. Seven of 23 (30%) discordant lesions were found to be cancers after final surgical pathology. Needle gauge was not associated with discordance. Operator experience was not associated with false-negative discordance.
Conclusions
A relatively low discordance rate (1.2%) was observed. However, a high percentage (30%; range in literature 11.7%–53.8%) of our discordant lesions were false negatives. This study emphasizes the need for careful radiological-pathologic review after SVAB and for repeat biopsy or surgical excision in the setting of discordance.
Introduction
The majority of the literature reviewing stereotactic vacuum-assisted biopsy (SVAB) and addressing discordance arises from the late 1990s and early 2000s when SVAB was an emerging technology. Early studies served to validate the efficacy of SVAB and demonstrated that SVAB was statistically less likely to lead to radiological-pathologic discordance and undersampling compared to stereotactic core biopsy . SVAB has now become a standard tool for tissue sampling of breast lesions, particularly lesions without a sonographic correlate, most frequently calcifications.
Recognition and documentation of discordance by the radiologist after tissue sampling is a key element of SVAB and is mandated by the American College of Radiology . Discordance suggests a lesion has not been sampled adequately and therefore raises the possibility of a missed cancer.
Get Radiology Tree app to read full this article<
Materials and Methods
Data Collection
Get Radiology Tree app to read full this article<
Stereotactic Vacuum Biopsy Techniques
Get Radiology Tree app to read full this article<
Determination of Discordance
Get Radiology Tree app to read full this article<
Statistical Analysis
Get Radiology Tree app to read full this article<
Results
Stereotactic Vacuum Biopsy Pathology Results
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Characteristics of Women with Discordant Lesions
Get Radiology Tree app to read full this article<
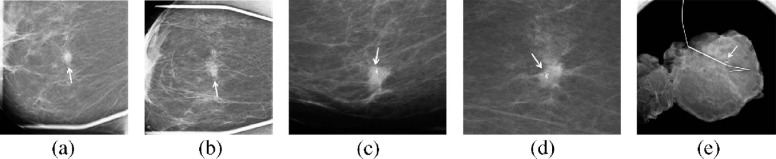
Characteristics of Discordant Lesions
Get Radiology Tree app to read full this article<
Reasons for Discordance
Get Radiology Tree app to read full this article<
Benign and High-risk Discordant Lesions
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
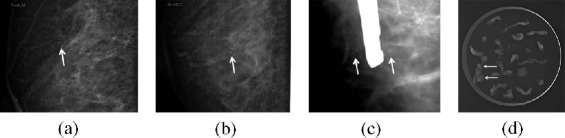
False-negative Discordant Lesions
Get Radiology Tree app to read full this article<
Table 1
Characteristics of False-negative Discordant Lesions
Lesion Type Description BI-RADS Biopsy Pathology Needle Gauge Needle Position Residual Calcs Final Pathology Calcs Pleomorphic 4c FCC 9G Correct A few HNG DCIS Calcs Pleomorphic 4c FCC 9G Correct, scant calcs Yes LNG DCIS Calcs Pleomorphic 5 FCC 9G Correct Yes IDC/HNG DCIS Calcs Amorphous 4b FCC 11G Incorrect Yes IDC/ING DCIS Calcs Pleomorphic 4c FCC 9G Incorrect Yes HNG DCIS Calcs Pleomorphic 5 FCC 9G Correct Yes IDC/HNG DCIS AD NA 5 FCC 9G Correct NA ING DCIS
AD, architectural distortion; BI-RADS, Breast Imaging Reporting and Data System; calcs, calcifications; DCIS, ductal carcinoma in situ; FCC, fibrocystic change; HNG, high nuclear grade; IDC, invasive ductal carcinoma; ING, intermediate nuclear grade; LNG, low nuclear grade; NA, not applicable.
Get Radiology Tree app to read full this article<
Impact of Needle Gauge
Get Radiology Tree app to read full this article<
Impact of Operator Experience
Get Radiology Tree app to read full this article<
Discussion
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Table 2
Studies Evaluating Discordance After Stereotactic Vacuum-assisted Biopsy
Study Sample Size (Lesions) Calcification Cases Needle Gauge Discordant Cases False-negative Discordant Cases (Cancers) Liberman et al. 741 523/741 (71%) 14G SVAB, 11G SVAB 19/741 (2.5%) 2/17 (11.7%) (only 17/19 lesions had repeat biopsy) Pfarl et al. 318 166/318 (52%) 11G SVAB 13/318 (4%) 7/13 (53.8%) Ciatto et al. \* 1388 1223/1388 (88%) 11G SVAB 4.4% (N/D not available; false negatives given for all lesions and modalities)
4/1391 (0.29%) (inadequacy rate VAB11G-includes two US cases) 50/151 (33%) (all lesions and modalities combined) Jackman et al. 1280 766/1280 (60%) 11G SVAB, 14G SVAB 16/1280 (1.3%) (nine with repeat biopsy; six stable imaging follow-up, mean 90 months; one lost to follow-up) 2/9 (22%) Venkataraman et al. 912 858/912 (94%) 11G SVAB, 8G SVAB 21/471 (4.4%) (471 = total benign lesions after initial biopsy) 3/21 (14%) Present study 1861 1409/1861 (76%) 11G SVAB, 9G SVAB 23/1861 (1.2%) 7/23 (30%)
N/D, numerator/denominator; SVAB, stereotactic vacuum assisted biopsy; US, ultrasound.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Limitations
Get Radiology Tree app to read full this article<
Conclusion
Get Radiology Tree app to read full this article<
References
1. Soo M.S., Ghate S., Delong D.: Stereotactic biopsy of noncalcified breast lesions: utility of vacuum-assisted technique compared to multipass automated gun technique. Clin Imaging 1999; 23: pp. 347-352.
2. Jackman R.J., Marzoni F.A., Nowels K.W.: Percutaneous removal of benign mammographic lesions: comparison of automated large-core and directional vacuum-assisted stereotactic biopsy techniques. AJR Am J Roentgenol 1998; 171: pp. 1325-1330.
3. Liberman L., Smolkin J.H., Dershaw D.D., et. al.: Calcification retrieval at stereotactic, 11-gauge, directional, vacuum-assisted breast biopsy. Radiology 1998; 208: pp. 251-260.
4. Philpotts L.E., Shaheen N.A., Carter D., et. al.: Comparison of rebiopsy rates after stereotactic core needle biopsy of the breast with 11-gauge vacuum suction probe versus 14-gauge needle and automatic gun. AJR Am J Roentgenol 1999; 172: pp. 683-687.
5. Lee S.-J., Mahoney M.C.: American College of Radiology practice parameter for the performance of stereotactic-guided breast interventional procedures. Available at: http://www.acr.org/~/media/62f6e5a180134df6a014447bdeb5384d.pdf Accessed December 15, 2015
6. National Institute on Aging : Menopause. Available at: https://www.nia.nih.gov/health/publication/menopause Accessed February 13, 2016
7. Lai J.T., Burrowes P., MacGregor J.H.: Diagnostic accuracy of a stereotaxically guided vacuum-assisted large-core breast biopsy program in Canada. Can Assoc Radiol J 2001; 52: pp. 223-227.
8. Apesteguia L., Mellado M., Sáenz J., et. al.: Vacuum-assisted breast biopsy on digital stereotaxic table of nonpalpable lesions non-recognisable by ultrasonography. Eur Radiol 2002; 12: pp. 638-645.
9. Kettritz U., Rotter K., Schreer I., et. al.: Stereotactic vacuum-assisted breast biopsy in 2874 patients: a multicenter study. Cancer 2004; 100: pp. 245-251.
10. Liberman L., Drotman M., Morris E.A., et. al.: Imaging-histologic discordance at percutaneous breast biopsy. Cancer 2000; 89: pp. 2538-2546.
11. Liberman L., Kaplan J.B., Morris E.A., et. al.: To excise or to sample the mammographic target: what is the goal of stereotactic 11-gauge vacuum-assisted breast biopsy?. AJR Am J Roentgenol 2002; 179: pp. 679-683.
12. Pfarl G., Helbich T.H., Riedl C.C., et. al.: Stereotactic 11-gauge vacuum-assisted breast biopsy: a validation study. AJR Am J Roentgenol 2002; 179: pp. 1503-1507.
13. Ciatto S., Houssami N., Ambrogetti D., et. al.: Accuracy and underestimation of malignancy of breast core needle biopsy: the Florence experience of over 4000 consecutive biopsies. Breast Cancer Res Treat 2007; 101: pp. 291-297.
14. Jackman R.J., Marzoni F.A., Rosenberg J.: False-negative diagnoses at stereotactic vacuum-assisted needle breast biopsy: long-term follow-up of 1,280 lesions and review of the literature. AJR Am J Roentgenol 2009; 192: pp. 341-351.
15. Venkataraman S., Dialani V., Gilmore H.L., et. al.: Stereotactic core biopsy: comparison of 11 gauge with 8 gauge vacuum assisted breast biopsy. Eur J Radiol 2012; 81: pp. 2613-2619.
16. Liberman L.: Percutaneous image-guided core breast biopsy. Radiol Clin North Am 2002; 40: pp. 483-500.
17. Johnson J.M., Johnson A.K., O’Meara E.S., et. al.: Breast cancer detection with short-interval follow-up compared with return to annual screening in patients with benign stereotactic or US-guided breast biopsy results. Radiology 2015; 275: pp. 54-60.