Rationale and Objectives
To propose a useful computed tomography (CT) criterion, the diameter with compression (DWC), especially in appendices with borderline diameters.
Materials and Methods
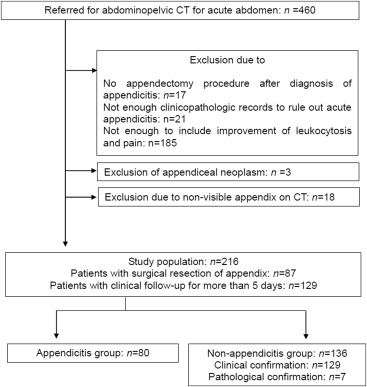
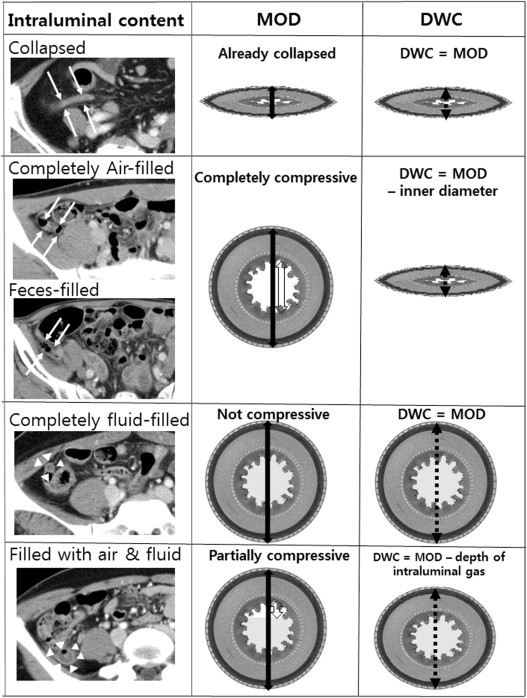
We retrospectively collected 216 patients with visible appendices on CT after clinicopathologic confirmation of appendicitis. Each CT criterion of appendicitis was evaluated by an experienced abdominal radiologist: maximal outer diameter (MOD), DWC, mural thickness and enhancement, periappendiceal infiltration, and appendicolith. DWC is the expected diameter after deduction of the intraluminal compressible contents such as air and feces. All the CT criteria were compared in the appendicitis and nonappendicitis group.
Results
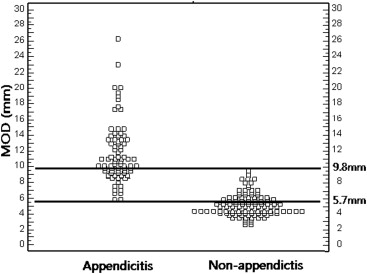
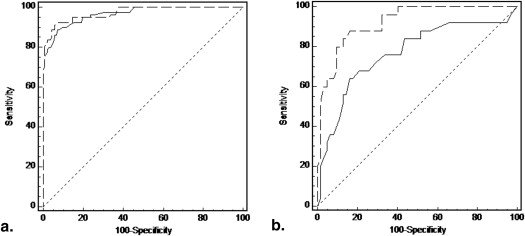
The areas under the receiver operating characteristic curve (AUC) of the MOD and the DWC were 0.967 and 0.973, respectively. The optimal cutoff value was 8.2 mm for the MOD and 6.6 mm for the DWC. Twenty-five of the 80 appendicitis patients (31.2%) and 62 of the 136 nonappendicitis patients (45.6%) had MODs between 5.7 mm and 9.8 mm in the overlap between the two groups. In this overlap, the AUC of the MODs declined sharply to 0.767, whereas the AUC of the DWCs remained 0.923. Use of the criterion of DWC >6.6 mm yielded a sensitivity of 84.0%, a specificity of 88.7%, and an accuracy of 87.4%. There were no other criteria with both sensitivity and specificity >80% in the range of overlap.
Conclusions
The proposed CT criterion of the DWC is not affected by normal distension or periappendiceal inflammation but only by true appendicitis. Therefore, DWC can improve the diagnostic performance of appendicitis regardless of the MOD.
Making a diagnosis of acute appendicitis begins with history taking and physical examination by clinicians and is completed by computed tomography (CT) and ultrasonography (US) in >50% of patients . US and CT are complementary approaches. US was the first diagnostic imaging modality for right lower quadrant pain until the early 2000s because it requires neither radiation nor an intravenous contrast medium . Use of CT has increased in the last decade as multidetector row computed tomography (MDCT) scanners have become more common, because these can provide rapid and accurate information not only on the appendix but also on other organs . US has a limited ability to locate the appendix, while incorrect diagnoses occur in CT examinations . Diagnostic errors in CT interpretation happen in two different circumstances depending on the visibility of the appendix. Visibility can be improved by optimization of CT scanning protocols and application of three-dimensional techniques or simply by using US . This is because the main problems are patients’ paucity of intra-abdominal fat or abnormal locations of the appendix . Diagnostic difficulties in cases of visible appendices arise from indeterminate CT findings especially in appendices with borderline diameters . Some important CT criteria for appendicitis are the same as the US criteria ; however, simple extrapolation from US to CT may not be valid because CT images are obtained without compression . For this and other reasons, several studies have compared the MODs of appendices on CT in patients with appendicitis to those of healthy people. A normal appendix is defined as <10 mm in diameter in most publications . On the basis of these results, an appendix with an MOD of 6–10 mm is indeterminate. Several groups have tried to improve the diagnostic performance for appendices with borderline MOD by proposing new CT criteria or combining established CT criteria . However, there are no published reports investigating diagnostic performance by established CT criteria for appendices with borderline MOD from the perspective of appendiceal compressibility, as in the case of the US criteria.
Hence, we investigate the diagnostic performance of established CT criteria in appendices with borderline MOD. We propose a possible new criterion to take account of appendiceal enlargement not because of appendicitis, namely diameter with compression (DWC), derived from the US criteria.
Materials and methods
Patients
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
CT Scan Protocol
Get Radiology Tree app to read full this article<
Interpretation of CT Studies
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Statistical Analysis
Get Radiology Tree app to read full this article<
Results
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Table 1
Sensitivity, Specificity, and Accuracy of Established Criteria
Criterion Sensitivity (%) Specificity (%) Accuracy (%) All ∗ Overlap † All ∗ Overlap † All ∗ Overlap † Maximal outer diameter > 8.2 mm 88.8 (71/80) 64.0 (16/25) 93.4 (127/136) 83.9 (52/62) 91.7 (198/216) 78.2 (68/87) Maximal outer diameter > 6 mm 97.5 (78/80) 92.0 (23/25) 59.6 (81/136) 11.3 (7/62) 73.6 (159/216) 34.5 (30/87) Diameter with compression > 6.6 mm 93.8 (75/80) 84.0 (21/25) 94.9 (129/136) 88.7 (55/62) 94.4 (204/216) 87.4 (76/87) Mural thickness > 1.1 mm 87.5 (70/80) 88.0 (22/25) 41.2 (56/136) 30.6 (19/62) 58.3 (126/216) 47.1 (41/87) Mural thickness > 3 mm 78.8 (63/80) 16.0 (21/25) 8.8 (12/136) 80.6 (50/62) 34.7 (75/216) 62.1 (54/87) Presence of mural enhancement 96.3 (77/80) 100 (25/25) 80.9 (110/136) 69.4 (43/62) 86.6 (187/216) 78.2 (68/87) Presence of periappendiceal infiltration 85.0 (68/80) 80.0 (20/25) 73.5 (100/136) 66.1 (41/62) 77.8 (168/216) 70.1 (61/87) Presence of appendicoliths 32.5 (26/80) 16.0 (4/25) 97.8 (133/136) 96.8 (60/62) 73.6 (159/216) 73.6 (64/87)
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Discussion
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
References
1. Rybkin A.V., Thoeni R.F.: Current concepts in imaging of appendicitis. Radiol Clin North Am 2007; 45: pp. 411-422. vii
2. Wagner P.L., Eachempati S.R., Soe K., et. al.: Defining the current negative appendectomy rate: for whom is preoperative computed tomography making an impact?. Surgery 2008; 144: pp. 276-282.
3. Jang KM, Lee K, Kim MJ, et al. What is the complementary role of ultrasound evaluation in the diagnosis of acute appendicitis after CT? Eur J Radiol74:71–76.
4. Courtney A.C., Nelson R.C., Patel M.B., et. al.: Making the diagnosis of acute appendicitis: do more preoperative CT scans mean fewer negative appendectomies? A 10-year study. Radiology 2010; 254: pp. 460-468.
5. Strouse P.J.: Pediatric appendicitis: an argument for US. Radiology 2010; 255: pp. 8-13.
6. Stoker J., van Randen A., Lameris W., et. al.: Imaging patients with acute abdominal pain. Radiology 2009; 253: pp. 31-46.
7. Webb E.M., Wang Z.J., Coakley F.V., et. al.: The equivocal appendix at CT: prevalence in a control population. Emerg Radiol 2010; 17: pp. 57-61.
8. Levine C.D., Aizenstein O., Lehavi O., et. al.: Why we miss the diagnosis of appendicitis on abdominal CT: evaluation of imaging features of appendicitis incorrectly diagnosed on CT. AJR Am J Roentgenol 2005; 184: pp. 855-859.
9. Levine C.D., Aizenstein O., Wachsberg R.H.: Pitfalls in the CT diagnosis of appendicitis. Br J Radiol 2004; 77: pp. 792-799.
10. Kosaka N., Sagoh T., Uematsu H., et. al.: Difficulties in the diagnosis of appendicitis: review of CT and US images. Emerg Radiol 2007; 14: pp. 289-295.
11. Jan Y.T., Yang F.S., Huang J.K.: Visualization rate and pattern of normal appendix on multidetector computed tomography by using multiplanar reformation display. J Comput Assist Tomogr 2005; 29: pp. 446-451.
12. Paulson E.K., Harris J.P., Jaffe T.A., et. al.: Acute appendicitis: added diagnostic value of coronal reformations from isotropic voxels at multi-detector row CT. Radiology 2005; 235: pp. 879-885.
13. Kim M.Y., Lee Y.M., Suh C.H., et. al.: Computed tomographic features of appendiceal serositis in pelvic inflammatory disease: comparison with pathological findings. J Comput Assist Tomogr 2007; 31: pp. 104-108.
14. Moteki T., Ohya N., Horikoshi H.: Evaluation of the maximum depth of intraluminal appendiceal fluid to diagnose appendicitis with a 64-detector row CT scanner. J Comput Assist Tomogr 2011; 35: pp. 703-710.
15. Pinto Leite N., Pereira J.M., Cunha R., et. al.: CT evaluation of appendicitis and its complications: imaging techniques and key diagnostic findings. AJR Am J Roentgenol 2005; 185: pp. 406-417.
16. Huwart L., El Khoury M., Lesavre A., et. al.: [What is the thickness of the normal appendix on MDCT?]. J Radiol 2007; 88: pp. 385-389.
17. Tamburrini S., Brunetti A., Brown M., et. al.: CT appearance of the normal appendix in adults. Eur Radiol 2005; 15: pp. 2096-2103.
18. Morse B.C., Roettger R.H., Kalbaugh C.A., et. al.: Abdominal CT scanning in reproductive-age women with right lower quadrant abdominal pain: does its use reduce negative appendectomy rates and healthcare costs?. Am Surg 2007; 73: pp. 580-584. discussion 584
19. Bursali A., Arac M., Oner A.Y., et. al.: Evaluation of the normal appendix at low-dose non-enhanced spiral CT. Diagn Interv Radiol 2005; 11: pp. 45-50.
20. Johnson P.T., Eng J., Moore C.J., et. al.: Multidetector-row CT of the appendix in healthy adults. Emerg Radiol 2006; 12: pp. 248-253.
21. Benjaminov O., Atri M., Hamilton P., et. al.: Frequency of visualization and thickness of normal appendix at nonenhanced helical CT. Radiology 2002; 225: pp. 400-406.
22. Sim J.Y., Kim H.J., Yeon J.W., et. al.: Added value of ultrasound re-evaluation for patients with equivocal CT findings of acute appendicitis: a preliminary study. Eur Radiol 2013; 23: pp. 1882-1890.
23. Jang K.M., Lee K., Kim M.J., et. al.: What is the complementary role of ultrasound evaluation in the diagnosis of acute appendicitis after CT?. Eur J Radiol 2010; 74: pp. 71-76.
24. Karabulut N., Boyaci N., Yagci B., et. al.: Computed tomography evaluation of the normal appendix: comparison of low-dose and standard-dose unenhanced helical computed tomography. J Comput Assist Tomogr 2007; 31: pp. 732-740.
25. Lai V., Chan W.C., Lau H.Y., et. al.: Diagnostic power of various computed tomography signs in diagnosing acute appendicitis. Clin Imaging 2012; 36: pp. 29-34.
26. Ives E.P., Sung S., McCue P., et. al.: Independent predictors of acute appendicitis on CT with pathologic correlation. Acad Radiol 2008; 15: pp. 996-1003.
27. Moteki T., Horikoshi H.: New CT criterion for acute appendicitis: maximum depth of intraluminal appendiceal fluid. AJR Am J Roentgenol 2007; 188: pp. 1313-1319.
28. Moteki T., Ohya N., Horikoshi H.: Prospective examination of patients suspected of having appendicitis using new computed tomography criteria including “maximum depth of intraluminal appendiceal fluid greater than 2.6 mm”. J Comput Assist Tomogr 2009; 33: pp. 383-389.