Rationale and Objectives
Neonates are at increased risk for cold stress and hypothermia in cool environments. An infant transport mattress (ITM) is commonly used to increase neonate temperature during transport and has been used during CT scanning. This study determined the impact of an ITM on radiation dose and image artifacts during CT scanning.
Materials and Methods
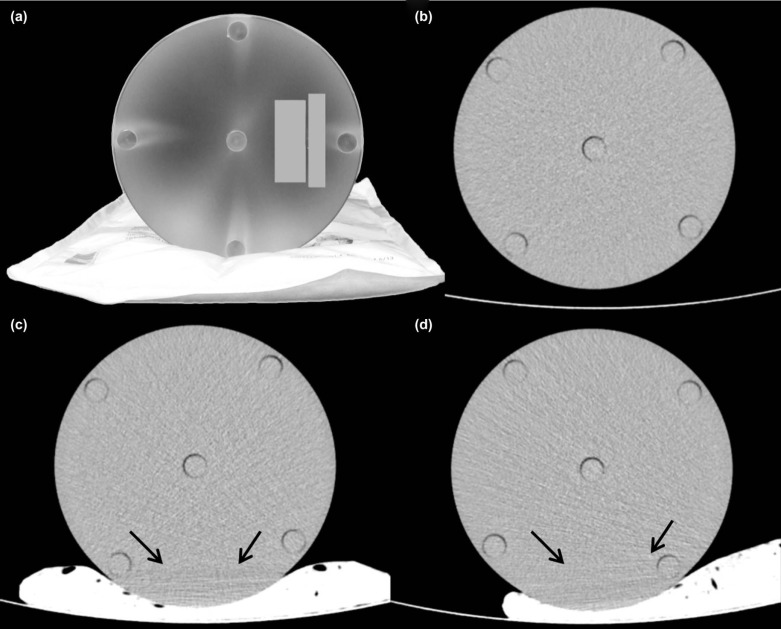
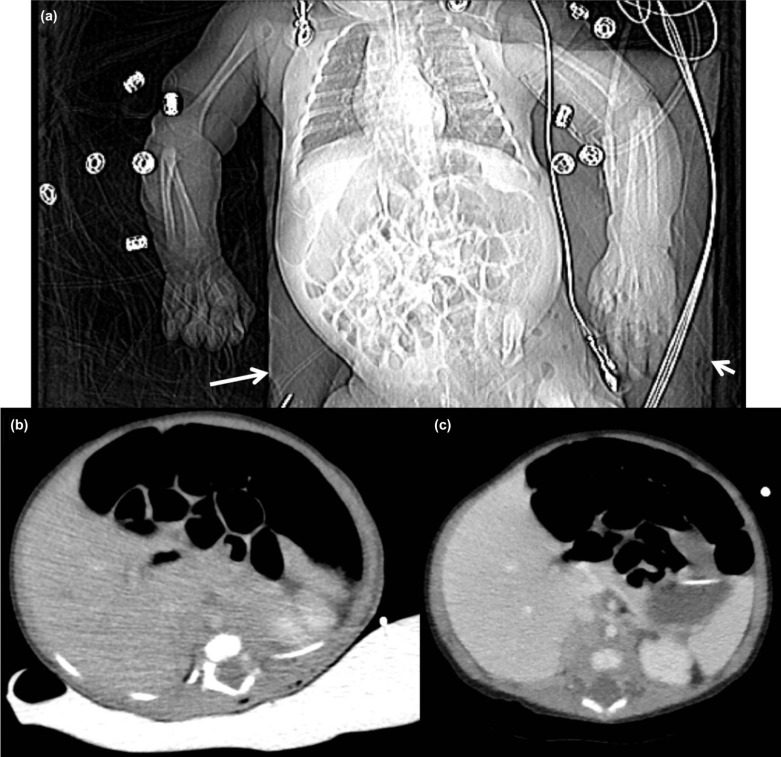
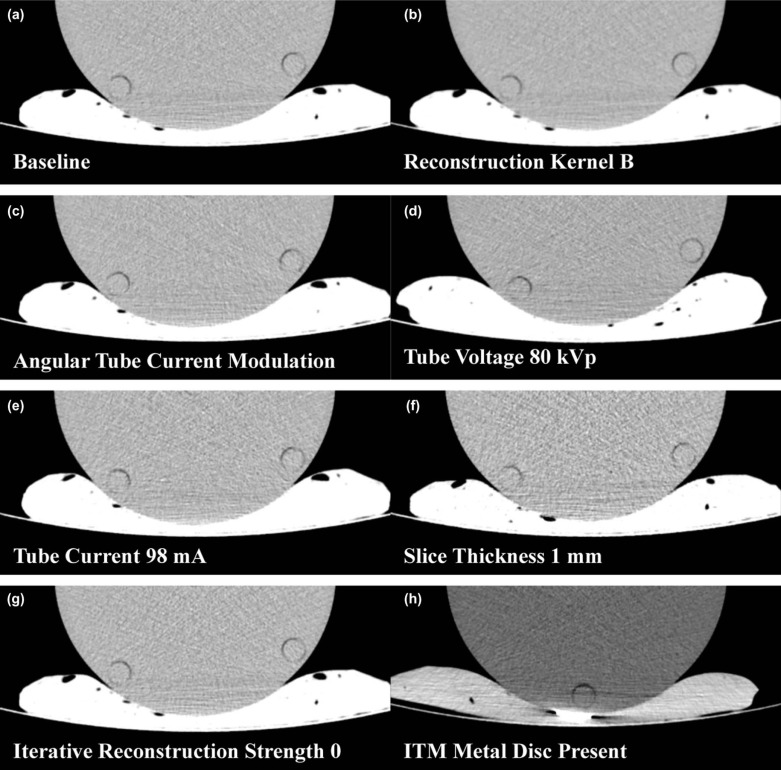
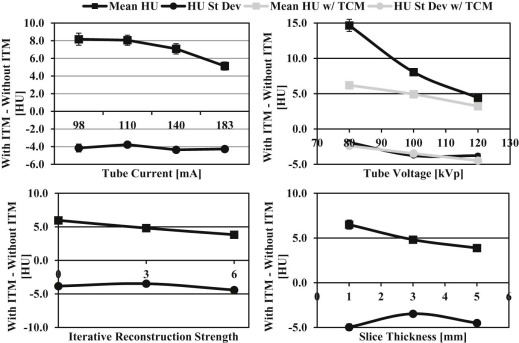
CT images from a single clinical patient scanned with an ITM were reviewed, and observations of image artifacts were recorded. A phantom was scanned with and without the ITM while varying tube-current modulation, reconstruction method, slice thickness, metal reduction algorithm, tube voltage, and tube current. The effects of the ITM on computed tomography dose index (CTDI vol ), mean Hounsfield unit (HU), and HU standard deviation were recorded.
Results
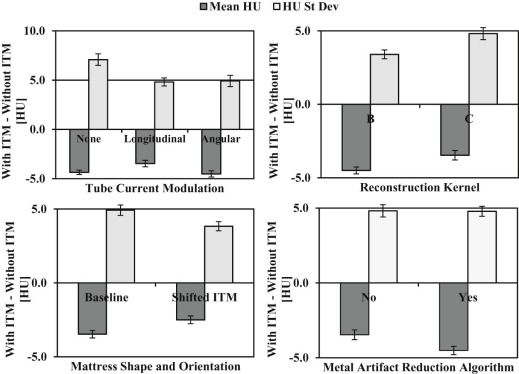
The clinical patient scan demonstrated significantly decreased mean HU and increased HU standard deviation. In the phantom, the ITM increased CTDI vol 27% and induced an artifact that decreased the mean HU by 3.5 HU and increased HU standard deviation by 4.6 HU. Angular tube-current modulation, strong iterative reconstruction, thick slices, metal artifact reduction, and high mA reduced the artifact.
Conclusion s
Using ITM during CT scanning is not recommended given the relatively brief scanning time, increased dose, and induced image artifacts. Based on our results, several acquisition parameters may be altered to mitigate the image artifact if an ITM is required during scanning.
Introduction
Thermal maintenance of the patient is an essential aspect of neonatal care, especially in pre-term and low birth weight infants . Cold stress and possible hypothermia due to loss of thermal maintenance can contribute to increased morbidity and mortality . Previous studies have demonstrated that covering the patient with a polyethylene wrap immediately after birth reduces cold stress and rates of hypothermia among neonates in the delivery room . Similarly, a specially designed warming infant transport mattress (ITM) placed under the neonate during transport has been shown to increase admission temperature and decrease the incidence of hypothermia . The use of a polyethylene or a warming mattress has also been endorsed by the American Heart Association and American Academy of Pediatric . In a survey of English neonatal units, 25.2% of units employed a warming mattress either alone or in conjunction with a polyethylene wrap for premature infants .
Little information currently exists related to neonatal cold stress and hypothermia during imaging. One brief study from 1980 suggests using a warming mattress during computed tomography (CT) scanning to decrease cold stress and the chance of hypothermia; however, studies using modern CT technology do not exist. Modern CT scanners implement several automatic exposure control technologies to reduce patient radiation dose and improve image quality. Although these technologies typically lead to reduced patient radiation dose, it is possible that the presence of a foreign object could confuse the automatic exposure control algorithms leading to increased patient radiation dose. Further, a foreign object could alter beam characteristics and cause image artifacts .
Get Radiology Tree app to read full this article<
Materials and Methods
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Clinical Patient Scan
Get Radiology Tree app to read full this article<
Table 1
CT Scanning Protocol for Clinical Patient Scan
Patient (Baseline) Protocol Phantom Protocol Tube voltage (kVp) 100 80, 100, 120 Tube current (mA) Automatic (110 at kidneys) Automatic (140 average); fixed: 98, 110, 140, and 182 Rotation time (s) 0.4 0.4 Automatic tube-current selection? Yes Yes and no Tube-current modulation Longitudinal None, longitudinal, and angular Reconstruction kernel C B and C Slice thickness (mm) 3 1, 3, and 5 Statistical iterative reconstruction strength 3 0, 3, and 6 Pitch 0.891 0.891 CT localizer AP only AP only Collimation 64 × 0.625 64 × 0.625 Metal artifact compensation algorithm? No Yes and no
AP, anteroposterior; CT, computed tomography.
Get Radiology Tree app to read full this article<
Phantom Scans
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Results
Clinical Patient Scan
Get Radiology Tree app to read full this article<
Phantom Scans
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Table 2
Acquisition Parameter Impact on Image Artifact. P -Values are between Given Parameters with the ITM
Mean HU with ITM Mean HU without ITM Mean HU change HU Standard Deviation with ITM HU Standard Deviation without ITM HU Standard Deviation Change_P_ -Value (Mean HU/HU Standard Deviation) Baseline 114.0 ± 0.6 117.5 ± 0.5 −3.5 ± 0.8 15.4 ± 0.9 10.8 ± 0.5 4.6 ± 1.0 vs 140 mA: 0.26/ < 0.01 Shifted ITM 115.0 ± 0.4 117.5 ± 0.5 −2.5 ± 0.6 14.6 ± 0.5 10.8 ± 0.5 3.8 ± 0.7 vs Baseline: 0.03/0.01 Angular tube-current modulation 113.3 ± 0.8 117.8 ± 0.2 −4.5 ± 0.8 16.1 ± 0.9 11.2 ± 1.1 4.9 ± 1.4 vs Baseline: 0.52/0.79 vs 140 mA: 0.65/ < 0.01 Iterative reconstruction strength 0 114.1 ± 0.6 117.9 ± 0.3 −3.8 ± 0.7 19.5 ± 1.0 13.5 ± 0.5 6.0 ± 1.1 – Iterative reconstruction strength 6 113.7 ± 0.6 118.1 ± 0.3 −4.4 ± 0.7 11.6 ± 0.7 7.8 ± 0.3 3.8 ± 0.8 vs Strength 0: 0.02/ < 0.01 1 mm Slice thickness 113.4 ± 0.9 118.4 ± 0.2 −5.0 ± 0.9 27.1 ± 0.8 20.6 ± 1.0 6.5 ± 1.3 – 5 mm Slice thickness 113.6 ± 0.2 118.1 ± 0.3 −4.5 ± 0.4 12.2 ± 0.6 8.3 ± 0.6 3.9 ± 0.8 vs 1 mm: 0.42/ < 0.01 Metal artifact reduction algorithm 113.6 ± 0.6 118.1 ± 0.4 −4.5 ± 0.7 15.4 ± 0.8 10.6 ± 0.3 4.8 ± 0.9 vs Baseline: 0.26/0.69 80 kVp 101.7 ± 0.4 104.1 ± 0.3 −2.4 ± 0.5 18.3 ± 0.7 12.1 ± 0.6 6.2 ± 0.9 – 120 kVp 119.8 ± 0.4 124.3 ± 0.1 −4.5 ± 0.4 15.2 ± 0.6 12.0 ± 0.3 3.2 ± 0.7 vs. 80 kVp: 0.03/ < 0.01 80 kVp at 110 mA 102.1 ± 0.9 104.0 ± 0.2 −1.9 ± 0.9 33.7 ± 1.7 19.1 ± 1.2 14.7 ± 2.1 – 120 kVp at 110 mA 121.0 ± 0.6 124.8 ± 0.2 −3.8 ± 0.6 14.5 ± 0.9 10.1 ± 0.5 4.4 ± 1.1 vs 80 kVp at 110 mA: < 0.01/ < 0.01 98 mA 114.0 ± 1.1 118.1 ± 0.2 −4.1 ± 1.1 20.9 ± 1.7 12.7 ± 0.2 8.2 ± 1.7 – 110 mA 113.8 ± 0.3 117.7 ± 0.2 −3.9 ± 0.4 19.9 ± 1.7 12.0 ± 0.4 7.9 ± 1.7 – 140 mA 113.5 ± 0.5 117.8 ± 0.2 −4.3 ± 0.5 18.3 ± 1.1 11.2 ± 0.9 7.1 ± 1.4 – 182 mA 113.5 ± 0.5 117.7 ± 0.2 −4.2 ± 0.5 15.1 ± 1.0 9.9 ± 0.5 5.2 ± 1.1 vs 98 mA: 0.85/0.03 Kernel B 112.6 ± 0.5 116.8 ± 0.3 −4.2 ± 0.6 10.7 ± 0.7 7.3 ± 0.3 3.4 ± 0.8 vs Baseline: 0.27/ < 0.01
HU, Hounsfield units; ITM, infant transport mattress.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Table 3
Acquisition Parameter Impact on Radiation Output
Slice mA with ITM Slice mA without ITM Slice mA change Slice CTDI vol with ITM (mGy) Slice CTDI vol without ITM (mGy) Slice CTDI vol change (mGy) Scan CTDI vol with ITM (mGy) Scan CTDI vol without ITM (mGy) Scan CTDI vol change Baseline 180 140 40 (28.6%) 6.6 5.2 1.4 (26.9%) 6.1 4.8 1.3 (27.1%) Shifted ITM 180 140 40 (28.6%) 6.5 5.2 1.3 (25.0%) 6.1 4.8 1.3 (27.1%) 80 kVp 342 269 96 (35.7%) 6.1 4.8 1.3 (27.1%) 5.7 4.4 1.3 (29.5%) 120 kVp 106 84 22 (26.2%) 6.2 5.1 1.1 (21.6%) 6.0 4.7 1.3 (27.7%) Angular tube-current modulation 162 140 22 (15.7%) 5.9 5.0 0.9 (18%) 5.8 5.0 0.8 (16.0%) 80 kVp with fixed 110 mA 110 110 – 2.0 2.0 – 2.0 2.0 – 120 kVp with fixed 110 mA 110 110 – 6.6 6.6 – 6.6 6.6 – 98 mA 98 98 – 3.6 3.6 – 3.6 3.6 – 110 mA 110 110 – 4.0 4.0 – 4.0 4.0 – 140 mA 140 140 – 5.1 5.1 – 5.1 5.1 – 182 mA 182 182 – 6.6 6.6 – 6.6 6.6 –
CTDI vol , volumetric computed tomography dose index; ITM, infant transport mattress.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Discussion
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Conclusions
Get Radiology Tree app to read full this article<
References
1. Silverman W.A, Fertig J.W., Berger A.P.: The influence of the thermal environment upon the survival of newly born premature infants. Pediatrics 1958; 22: pp. 876-886.
2. Almeida P.G., Chandley J., Davis J., et. al.: Use of the heated gel mattress and its impact on admission temperature of very low birth-weight infants. Adv Neonatal Care 2009; 9: pp. 34-39.
3. Buetow K.C., Klein S.W.: Effect of maintenance of “normal” skin temperature on survival of infants of low birth weight. Pediatrics 1964; 34: pp. 163-170.
4. Day R.L., Caliguiri L., Kamenski C., et. al.: Body temperature and survival of premature infants. Pediatrics 1964; 34: pp. 171-181.
5. Russo A., McCready M., Torres L., et. al.: Reducing hypothermia in preterm infants following delivery. Pediatrics 2014; 133: pp. e1055-e1062.
6. Chawla S., Amaram A., Gopal S.P., et. al.: Safety and efficacy of Trans-warmer mattress for preterm neonates: results of a randomized controlled trial. J Perinatol 2011; 31: pp. 780-784.
7. Kattwinkel J., Perlman J.M., Aziz K., et. al.: Part 15: Neonatal resuscitation 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2010; 122: pp. S909-S919.
8. Perlman J.M., Wyllie J., Kattwinkel J., et. al.: Special report—neonatal resuscitation: 2010 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Circulation 2010; 122: pp. S516-S538.
9. Godhamgaonkar A., Parmar V., Kyte E., et. al.: The use of polythene bags for delivery-room thermoregulation in premature babies across England. Arch Dis Child Fetal Neonatal Ed 2011; 96: pp. Fa36.
10. Marks K., Maisels J., Lee C.A.: Temperature control during computerized tomography and in-hospital transport of low-birth-weight infants. Am J Dis Child 1980; 134: pp. 1176-1177.
11. Coursey C., Frush D.P., Yoshizumi T., et. al.: Pediatric chest MDCT using tube current modulation: effect on radiation dose with breast shielding. AJR Am J Roentgenol 2008; 190: pp. W54-W61.
12. Rizzo S.M., Kalra M.K., Maher M.M., et. al.: Do metallic endoprostheses increase radiation dose associated with automatic tube-current modulation in abdominal-pelvic MDCT? A phantom and patient study. AJR Am J Roentgenol 2005; 184: pp. 491-496.
13. Boone J.M., Strauss K.J., Cody D.D., et. al.: Size-specific dose estimates (SSDE) in pediatric and adult body CT examinations: Report of AAPM Task Group 204. American Association of Physicists in Medicine, College Park, MD2011.
14. Kak A.C., Slaney M.: Aliasing artifacts and noise in CT images.Kak A.C.Slaney M.Principles of computerized tomographic imaging.1988.IEEE PressPiscataway Township, NJ:pp. 177-201.
15. Raman S.P., Johnson P.T., Deshmukh S., et. al.: CT Dose reduction applications: available tools on the latest generation of CT scanners. J Am Coll Radiol 2013; 10: pp. 37-41.