Rationale and Objectives
To assess practice patterns in evaluating incidental findings at chest computed tomography (CT) to determine the need for further education.
Materials and Methods
A survey was given to 1600 radiologists, presenting four clinical case questions regarding the evaluation/significance of the following incidental findings at chest CT: thyroid lesion; enlarged mediastinal lymph nodes; asymptomatic, small pulmonary embolus; and small lung nodule. The respondents’ answers were compared with “truth,” as defined by the best evidence available in the medical literature. Additional questions elicited the respondents’ demographics and comfort levels in addressing the findings. Analysis of variance models with a Tukey correction for post hoc comparisons and chi-square tests were used to determine if any demographic factors or comfort levels were predictive of higher correct response rates.
Results
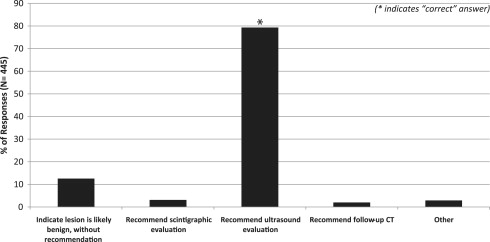
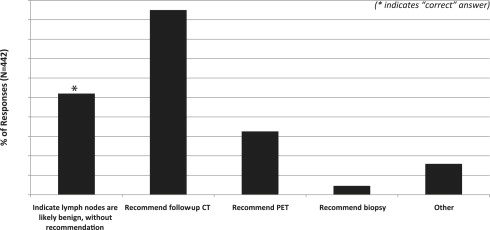
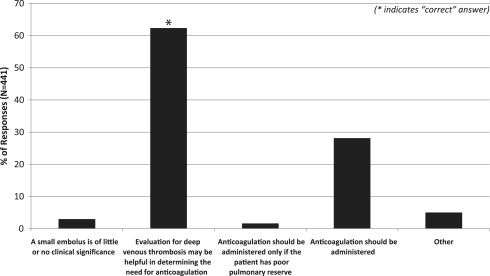
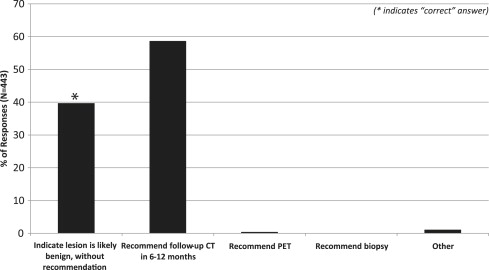
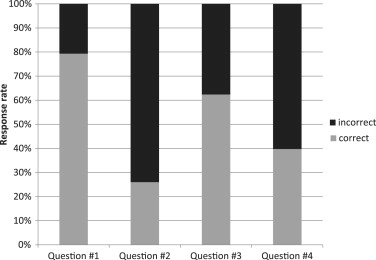
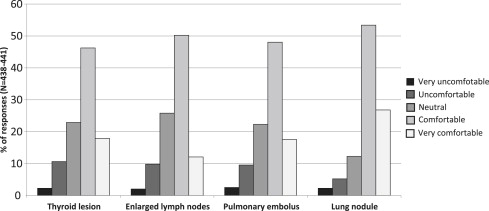
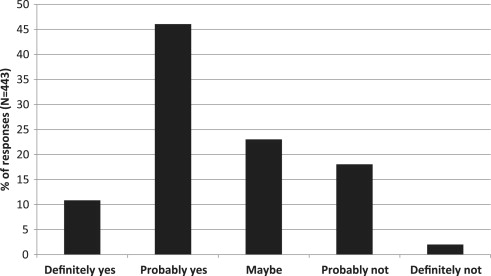
The overall survey response rate was 28% (445/1600). Correct case response rates ranged from 26% (115/442) to 79% (343/445). Only 6% (28/438) of respondents chose the correct answers for all cases. Up to 80% (353/440) of respondents felt comfortable in addressing findings, and only 57% (252/443) of respondents felt that they needed more training in this area. Fellowship training in cardiothoracic radiology, working in a teaching practice, and subspecialization in abdominal or cardiothoracic radiology were predictive of higher correct response rates. Except for one case question, the comfort level was not predictive of correct response rate.
Conclusions
There was considerable variability among radiologists and substantial deviation from best medical practice with regard to the interpretation/evaluation of incidental findings at chest CT, signifying a significant need for further education.
Chest computed tomography (CT) scans have been employed with increasing frequency over the past two decades, both in patients with known diseases as well as in screening situations (eg, for lung cancer and coronary artery disease), leading to an explosion in the use of the modality. Approximately 3%–24% of chest CT exams show potentially significant incidental findings that require further evaluation or follow-up . The evaluation of such a large number of findings presents a huge potential burden on the health care system. The purpose of this survey-style study was to gain information about current practice patterns in the interpretation and evaluation of incidental chest CT findings, and to compare these patterns with the best available medical evidence, to assess the need for in-training and continuing medical education in this area.
Methods
An electronic survey was given to three groups of radiologists, as follows:
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Statistical Analysis
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Results
Get Radiology Tree app to read full this article<
Table 1
Demographic Data for 445 Survey Respondents
Variable Number of Responses (%) Job description ∗ Trainee (resident or fellow) 46 (10.4) General practice radiologist 227 (51.4) Abdominal radiology specialist 96 (21.7) Cardiothoracic radiology specialist 39 (8.8) Other 34 (7.7) Number of years in practice ∗ <1 51 (11.5) 1–5 69 (15.6) 6–10 65 (14.7) 11–15 58 (13.1) 16–20 62 (14.0) >20 137 (31.0) Type of practice † In training 46 (10.4) University/teaching 133 (30.2) Nonteaching 262 (59.4) Fellowship training in cardiothoracic radiology (nontrainees only) Yes (personal) ‡ 38 (9.6) Yes (member of group) § 161 (40.6)
Note: some respondents omitted certain responses regarding demographics, as follows:
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Discussion
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Conclusions
Get Radiology Tree app to read full this article<
Appendix
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Very Uncomfortable Uncomfortable Neutral Comfortable Very Comfortable Thyroid lesion ○ ○ ○ ○ ○ Enlarged lymph Nodes ○ ○ ○ ○ ○ Pulmonary embolus ○ ○ ○ ○ ○ Lung nodule ○ ○ ○ ○ ○
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
References
1. Jacobs P.C., Mali W.P., Grobbee D.E., et. al.: Prevalence of incidental findings in computed tomographic screening of the chest: a systematic review. J Comp Assisted Tomogr 2008; 32: pp. 214-221.
2. Johnson K.M., Dennis J.M., Dowe D.A.: Extracardiac findings on coronary CT angiograms: limited versus complete image review. AJR Am J Roentgenol 2010; 195: pp. 143-148.
3. Veronesi G., Bellomi M., Spaggiari L.: The rate of incidental findings in lung cancer screening trials is not negligible. Eur Radiol 2008; 18: pp. 529.
4. van de Wiel J.C., Wang Y., Xu D.M., et. al.: Neglectable benefit of searching for incidental findings in the Dutch-Belgian lung cancer screening trial (NELSON) using low-dose multidetector CT. Eur Radiol 2007; 17: pp. 1474-1482.
5. Hall W.B., Truitt S.G., Scheunemann L.P., et. al.: The prevalence of clinically relevant incidental findings on chest computed tomographic angiograms ordered to diagnose pulmonary embolism. Arch Intern Med 2009; 169: pp. 1961-1965.
6. Yoon D.Y., Chang S.K., Choi C.S., et. al.: The prevalence and significance of incidental thyroid nodules identified on computed tomography. J Comput Assisted Tomogr 2008; 32: pp. 810-815.
7. Shetty S.K., Maher M.M., Hahn P.F., et. al.: Significance of incidental thyroid lesions detected on CT: correlation among CT, sonography, and pathology. AJR Am J Roentgenol 2006; 187: pp. 1349-1356.
8. Cooper D.S., Doherty G.M., Haugen B.R., et. al.: Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid 2009; 19: pp. 1167-1214.
9. Ahmed S., Horton K.M., Jeffrey R.B., et. al.: Incidental thyroid nodules on chest CT: review of the literature and management suggestions. AJR Am J Roentgenol 2010; 195: pp. 1066-1071.
10. Attili A.K., Kazerooni E.A., Gross B.H., et. al.: Thoracic lymph node enlargement in usual interstitial pneumonitis and nonspecific-interstitial pneumonitis: prevalence, correlation with disease activity and temporal evolution. J Thoracic Imaging 2006; 21: pp. 288-292.
11. Niimi H., Kang E.Y., Kwong J.S., et. al.: CT of chronic infiltrative lung disease: prevalence of mediastinal lymphadenopathy. J Comp Assisted Tomogr 1996; 20: pp. 305-308.
12. Souza C.A., Muller N.L., Lee K.S., et. al.: Idiopathic interstitial pneumonias: prevalence of mediastinal lymph node enlargement in 206 patients. AJR Am J Roentgenol 2006; 186: pp. 995-999.
13. Goodman L.R.: Small pulmonary emboli: what do we know?. Radiology 2005; 234: pp. 654-658.
14. MacMahon H., Austin J.H., Gamsu G., et. al.: Guidelines for management of small pulmonary nodules detected on CT scans: a statement from the Fleischner Society. Radiology 2005; 237: pp. 395-400.
15. Gould M.K., Fletcher J., Iannettoni M.D., et. al.: Evaluation of patients with pulmonary nodules: when is it lung cancer? ACCP evidence-based clinical practice guidelines (2nd edition). Chest 2007; 132: pp. 108S-130S.
16. Casarella W.J.: A Patient’s Viewpoint on a Current Controversy. Radiology 2002; 224: pp. 927.
17. Berland L.L., Silverman S.G., Gore R.M., et. al.: Managing incidental findings on abdominal CT: white paper of the ACR incidental findings committee. J Am Coll Radiol JACR 2010; 7: pp. 754-773.
18. Eisenberg R.L., Bankier A.A., Boiselle P.M.: Compliance with Fleischner Society guidelines for management of small lung nodules: a survey of 834 radiologists. Radiology 2010; 255: pp. 218-224.
19. Prosch H., Strasser G., Oschatz E., et. al.: Management of patients with small pulmonary nodules: a survey of radiologists, pulmonologists, and thoracic surgeons. AJR Am J Roentgenol 2006; 187: pp. 143-148.