Rationale and Objectives
Abdominal magnetic resonance angiography (MRA) has gained favor in pediatric patients owing to its lack of ionizing radiation and noninvasive nature. Reports exist regarding incidental findings on body MRA in adult patients. However, the incidental findings in pediatric abdominal MRA have not been previously reported. Our study aims to determine the frequencies, characteristics, and categories of incidental findings in pediatric patients undergoing abdominal MRA.
Materials and Methods
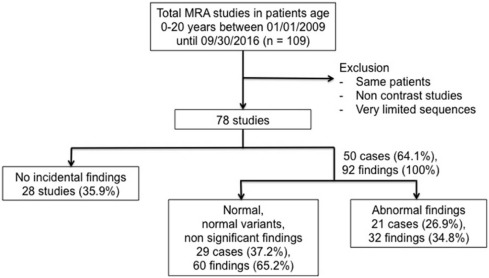
Retrospective study was performed in 78 consecutive contrast-enhanced abdominal MRA of patients between ages 0 and 20 years over a 7-year time period. The presence of incidental vascular and extravascular findings was noted. Reports were categorized in consensus by two radiologists as no incidental finding (group A), normal or normal variants or nonsignificant incidental common findings (group B), or abnormal incidental findings (group C). Group C was reviewed to determine whether additional management was performed.
Results
A total of 40 boys and 38 girls (51%:49%) were reported, with a mean age of 12.3 years (standard deviation ±5.6 years, range 7 days to 20 years). Three most common indications for MRA were renal artery stenosis (24.4%), vasculitis (21.8%), and suspected intra-abdominal venous thrombosis (14.1%). We identified a total of 92 incidental findings in 50 of 78 patients; 60 findings in 29 patients in group B, and 32 findings in 21 patients in group C. Atelectasis at the lung bases was the most common incidental finding in group B (14 of 78 patients). The most common findings in group C were ascites, scoliosis, and splenomegaly. There were three abnormal incidental findings that led to causative workup and/or further management (moderate ascites, pericardial and pleural effusion, and venous malformation). The remaining cases with abnormal findings received treatment of their primary conditions only.
Conclusions
Pediatric abdominal MRA revealed a large number of incidental findings. The large majority were findings without clinical significance. Basal lung atelectasis was the most common overall incidental and nonsignificant finding, whereas ascites was the most common abnormal incidental finding. Although not all abnormal incidental findings affected management, appropriate identification and communication of relevant findings would improve patient care.
Introduction
Magnetic resonance angiography (MRA) is a noninvasive method for evaluation of arterial blood vessels . It has many advantages such as excellent tissue contrast, multi-planar imaging capability, and non-contrast angiographic imaging. Recently, MRA has become the favored mode of angiographic imaging over computed tomography angiography or digital subtraction angiography in pediatric patients owing to its lack of ionizing radiation and noninvasive nature .
The preference for MRA in pediatric patients also holds true with respect to imaging of abdominal vasculature. Common indications for abdominal MRA of children are renal artery stenosis, vasculitis, tumor vascularity, portal hypertension, and transplant evaluation . There is no single widely accepted standard protocol of abdominal MRA in children. Additionally, there is variability in the amount of non-angiographic sequences performed to assess extravascular structures.
Get Radiology Tree app to read full this article<
Materials and Methods
Get Radiology Tree app to read full this article<
TABLE 1
Current Institutional Protocol for Pediatric MRA
Sequences Plane TR/TE (ms) Flip Angle NSA Slice Thickness/Spacing (mm) Rationale T2-weighted single-shot fast spin echo Coronal 1065/865 142 2 4/−2 Overview anatomic assessment T2-weighted motion correction radial fat-saturated sequence Axial 6375/93.6 142 2 4/0 General anatomic assessment, motion-resistant sequence useful in pediatric patients T1-weighted SPGR DIXON fat saturated (including in/opposed phase) Axial 7.4/1.9 10 0.7 3.2/−1.6 Anatomic assessment, characterization of the lesion before contrast-enhanced phase Time resolved MRA sequence Coronal 3.4/1.4 16 0.75 3/−1.5 High temporal and spatial volumetric MRA imaging T1-weighted SPGR DIXON fat saturated (including in/opposed phase) Axial and coronal 7.4/1.9 10 0.7 3.2/−1.6 Delayed imaging
MRA, magnetic resonance angiography; NSA, number of signal averages; SPGR, spoiled gradient recalled echo; TR/TE, repetition time/echo time.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Results
Demographic Data
Get Radiology Tree app to read full this article<
TABLE 2
Indications for MRA
Conditions Number of Cases (%) Renal artery stenosis 19 (24.4%) Vasculitis 17 (21.8%) Suspected intra-abdominal venous thrombosis 11 (14.1%) Vascular malformation, aneurysm, syndromic abnormality 11 (14.1%) Post liver transplantation concerning for vascular complication 7 (9.0%) Other venous conditions such as venous shunt, portal hypertension with shunt, Budd-Chiari syndrome 6 (7.7%) Preoperative evaluation of neuroblastoma or retroperitoneal mass 3 (3.8%) Others such as abdominal pain, nausea, vomiting 3 (3.8%) No given history 1 (1.3%)
MRA, magnetic resonance angiography.
Get Radiology Tree app to read full this article<
Incidental Findings on MRA
Get Radiology Tree app to read full this article<
TABLE 3
Incidental Findings Deemed Clinically Insignificant (“Group B”)
System, Organ Findings Total (%) Reproductive tract Small ovarian cyst (1) 1 (1.7%) Urinary tract Extrarenal pelvises (2), renal cysts (2), atrophic kidney (1), absent unilateral kidney (1), unilateral hypertrophy (1) 7 (11.7%) Lymph nodes Enlarged LN > 1 cm in short axis (3) 3 (5.0%) Visualized basal lungs and mediastinum Atelectasis (14), trace pleural effusion (3), trace pericardial effusion (3) 20 (33.3%) Hepatobiliary system Mild IHD dilatation (1), small hemangioma (1), hepatic cyst (1), bile sludge (1), variant left hepatic lobe (1) 5 (8.3%) Bowel Dilated loops (2) 2 (3.3%) Spleen and pancreas Pancreatic divisum (2), accessory spleen (1) 3 (5.0%) Musculoskeletal system Dependent edema (2), pectus excavatum (1), bilateral 13th ribs (1) 4 (6.7%) Incidental vascular findings Accessory renal artery (6), retroaortic left renal vein (2), circumaortic left renal vein (1), common origin of celiac axis and SMA (1), replaced right hepatic artery (1) 11 (18.3%) Others Minimal physiologic fluid in pelvic cavity (3), situs inversus (1) 4 (6.7%) Total 60 (100%)
IHD, intrahepatic duct; LN, lymph node; SMA, superior mesenteric artery.
TABLE 4
Incidental Findings Deemed Clinically Significant (“Group C”)
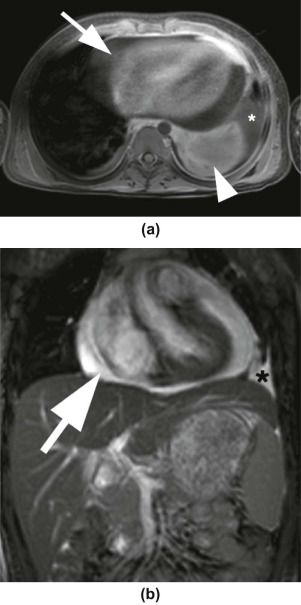
System, Organ Findings Total (%) Reproductive tract Hemorrhagic cyst (1) 1 (3.1%) Urinary tract Angiomyolipoma (1), atrophic kidney with scar (1) 2 (6.3%) Visualized basal lungs and mediastinum Moderate pleural effusion (1), large pericardial effusion (1), pneumonia (1) 3 (9.4%) Hepatobiliary system Hepatomegaly (1), hepatic steatosis (1), isolated CHD dilatation (1), gallstone (1) 4 (12.5%) Spleen and pancreas Splenomegaly (4), pancreatitis (1) 5 (15.6%) Musculoskeletal system Scoliosis (4), anterior compression fracture with degenerative disc and end plate (1), peripheral nerve sheath tumor or myxoid tumor (1) 6 (18.8%) Neurologic system Neurofibroma (1; Fig 4 ) 1 (3.1%) Incidental vascular findings Nutcracker syndrome (1; Fig 5 ), venous malformation (1), significant dilated superficial and deep vein of pelvis (1) 3 (9.4%) Others Ascites (6), umbilical hernia (1) 7 (21.8%) Total 32 (100%)
CHD, common hepatic duct.
Get Radiology Tree app to read full this article<
Further Management of Abnormal Incidental Findings
Get Radiology Tree app to read full this article<
TABLE 5
Recorded Follow-up of Clinically Significant Incidental Findings (“Group C”) Listed By Organ System
System Abnormal Incidental Findings (Group C) Further Workup or Management Musculoskeletal system A peripheral nerve sheath tumor or myxoid tumor Advised and followed up with ultrasound, not surgery Musculoskeletal system Mild to moderate S-shaped scoliosis Periodic X-ray and follow-up with orthopedist Incidental vascular findings Venous malformation at right renal hilum and dilated superficial and deep vein in pelvis Further dedicated MRI of the abdomen and pelvis Others Moderate amount of ascites Worked up and treated protein-losing enteropathy and multiple food allergies with enteritis (no definite diagnosis and patient was lost to follow-up), no record of abdominal paracentesis Others Moderate left and small right pleural effusion, large pericardial effusion, small amount of ascites, hepatomegaly, and splenomegaly Worked up and treated SLE with LN, no record of pleural or pericardial drainage
LN, Lupus nephritis; MRI, magnetic resonance imaging; SLE, systemic lupus erythematosus.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Discussion
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Appendix
Supplementary Data
Get Radiology Tree app to read full this article<
Table S1
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
References
1. Chavhan G.B., Babyn P.S., Philip J., et. al.: Pediatric body MR angiography: principles, techniques, and current status in body imaging. AJR Am J Roentgenol 2015; 205: pp. 173-184.
2. Sada D.M., Vellody R., Liu P.S.: Magnetic resonance angiography of the pediatric abdomen and pelvis: techniques and imaging findings. Magn Reson Imaging Clin N Am 2013; 21: pp. 843-860.
3. Glockner J.F.: Incidental findings on renal MR angiography. AJR Am J Roentgenol 2007; 189: pp. 693-700.
4. Sohns J.M., Wieland S., Jan M., et. al.: Vascular and extravascular findings on magnetic resonance angiography of the thoracic aorta and the origin of the great vessels. J Magn Reson Imaging 2013; 40: pp. 988-995.
5. Chen Q., Qun C., Stock K.W., et. al.: Fast magnetic resonance imaging techniques. Eur J Radiol 1999; 29: pp. 90-100.
6. Tusman G., Böhm S.H., Tempra A., et. al.: Effects of recruitment maneuver on atelectasis in anesthetized children. Anesthesiology 2003; 98: pp. 14-22.
7. Acosta C.M., Maidana G.A., Daniel J., et. al.: Accuracy of transthoracic lung ultrasound for diagnosing anesthesia-induced atelectasis in children. Anesthesiology 2014; 120: pp. 1370-1379.
8. Khosa F., Krinsky G., Macari M., et. al.: Managing incidental findings on abdominal and pelvic CT and MRI, part 2: white paper of the ACR incidental findings committee II on vascular findings. J Am Coll Radiol 2013; 10: pp. 789-794.
9. Pozo A.L., Godfrey E.M., Bowles K.M.: Splenomegaly: investigation, diagnosis and management. Blood Rev 2009; 23: pp. 105-111.
10. Runyon B.A.: Care of patients with ascites. N Engl J Med 1994; 330: pp. 337-342.
11. Akbarnia B.A.: Management themes in early onset scoliosis. J Bone Joint Surg Am 2007; 89: pp. 42-54.
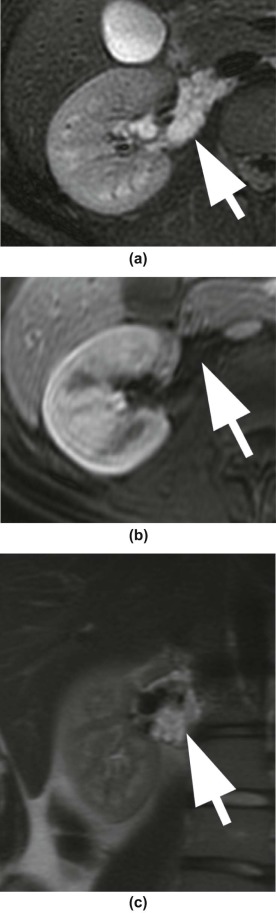
![Figure 4, Ten-year-old boy with hypertension referred to workup for renal artery stenosis. (a,b) Axial radial T2-weighted (Periodically Rotated Overlapping ParallEL Lines with Enhanced Reconstruction [PROPELLER]) with fat saturation (FS) images reveal perihepatic neurofibromas, seen as lobulated and ovoid T2-weighted hyperintense lesions in the periportal region ( large arrow ). (c,d) Axial radial T2-weighted (PROPELLER) with FS images show several subcutaneous and abdominal wall neurofibromas ( small arrows ).](https://storage.googleapis.com/dl.dentistrykey.com/clinical/IncidentalFindingsonPediatricAbdominalMagneticResonanceAngiography/3_1s20S1076633217300739.jpg)
![Figure 5, Eleven-year-old girl with clinical history of hypertension leading to concern for underlying renal artery stenosis. (a) Axial radial T2-weighted (Periodically Rotated Overlapping ParallEL Lines with Enhanced Reconstruction [PROPELLER]) with fat saturation (FS) and (b) axial postcontrast three-dimensional fat-saturated T1-weighted spoiled gradient echo images show severe compression of the left renal vein ( arrow ) between the superior mesenteric artery ( arrowhead ) and the aorta ( asterisk ).](https://storage.googleapis.com/dl.dentistrykey.com/clinical/IncidentalFindingsonPediatricAbdominalMagneticResonanceAngiography/4_1s20S1076633217300739.jpg)