Rationale and Objectives
To determine if the rate of major discrepancies between resident preliminary reports and faculty final reports increases during the final hours of consecutive 12-hour overnight call shifts.
Materials and methods
Institutional review board exemption status was obtained for this study. All overnight radiology reports interpreted by residents on-call between January 2010 and June 2010 were reviewed by board-certified faculty and categorized as major discrepancies if they contained a change in interpretation with the potential to impact patient management or outcome. Initial determination of a major discrepancy was at the discretion of individual faculty radiologists based on this general definition. Studies categorized as major discrepancies were secondarily reviewed by the residency program director (M.H.S.) to ensure consistent application of the major discrepancy designation. Multiple variables associated with each report were collected and analyzed, including the time of preliminary interpretation, time into shift study was interpreted, volume of studies interpreted during each shift, day of the week, patient location (inpatient or emergency department), block of shift (2-hour blocks for 12-hour shifts), imaging modality, patient age and gender, resident identification, and faculty identification. Univariate risk factor analysis was performed to determine the optimal data format of each variable (ie, continuous versus categorical). A multivariate logistic regression model was then constructed to account for confounding between variables and identify independent risk factors for major discrepancies.
Results
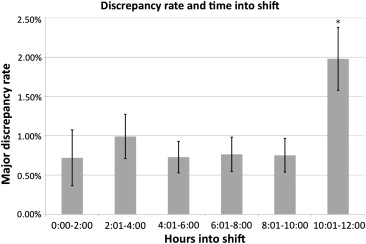
We analyzed 8062 preliminary resident reports with 79 major discrepancies (1.0%). There was a statistically significant increase in major discrepancy rate during the final 2 hours of consecutive 12-hour call shifts. Multivariate analysis confirmed that interpretation during the last 2 hours of 12-hour call shifts (odds ratio (OR) 1.94, 95% confidence interval (CI) 1.18–3.21), cross-sectional imaging modality (OR 5.38, 95% CI 3.22–8.98), and inpatient location (OR 1.81, 95% CI 1.02–3.20) were independent risk factors for major discrepancy.
Conclusions
In a single academic medical center, major discrepancies in resident preliminary reports increased significantly during the final 2 hours of consecutive 12-hour overnight call shifts. This finding could be related to either fatigue or circadian desynchronization. Discrimination of these two potential etiologies requires additional investigation as major discrepancies in resident reports have the potential to negatively impact patient care/outcome. Cross-sectional imaging modalities including computed tomography and ultrasound (versus conventional radiography), as well as inpatient location (versus Emergency Department location), were also associated with significantly higher major discrepancy rates.
The recurring controversy involving resident work hour restrictions was initially driven by an increasing perception of the negative impact of fatigue and medical error on health care quality and patient safety. New York State enacted a health-code regulation in 1989 to restrict resident work hours and increase supervision of physicians in training . In 2003, the Accreditation Council for Graduate Medical Education (ACGME) enacted the first iteration of the common duty hour standards in response to public consumer advocate concerns that excessive resident duty hours may jeopardize quality of care . The New York State regulation and first generation duty hour standards resulted in a litany of both retrospective and prospective studies evaluating the impact work hour restrictions on various performance measures ranging from fine motor coordination, response time, and self-reported sleepiness to sharps-related injuries, medication ordering errors, and morbidity/mortality rates. While many controlled studies convincingly demonstrated that increasing shift length is associated with deterioration in attention and motor and cognitive skills , subsequent restriction of resident work hours has not translated into clear or convincing improvements in patient outcomes. Continued changes to the existing work-hour limitations have prompted physician, government, and patient safety advocate groups to call for more rigorous study of the impact of existing work hour regulations .
Implicit in the movement toward shorter work hours is the assumption that physician cognitive performance deteriorates during the course of a prolonged call shift. Detecting such deficits experimentally, however, can be challenging; structured laboratory cognitive experiments may fail to capture the full complexities of medical practice, while the highly variable clinical environment of most medical specialties does not lend itself well to uniform measurement. In contrast to many clinical specialties, however, there is relatively little variation in the cognitive tasks performed by radiology residents during the course of a call shift. Although particular diagnoses differ between individual cases, the overall process of image interpretation tends to remain constant. Moreover, discrete cognitive decisions (ie, diagnostic impressions) rendered by radiology residents are clearly documented and can be subsequently reviewed in a formalized process by faculty radiologists. These features, along with the relatively constant workload throughout call shifts, make the study of fatigue-related cognitive deterioration particularly attractive in this context. Therefore, we sought to evaluate major discrepancy rates during consecutive 12-hour overnight call shift to determine if there is a decrement in performance during the final hours of these shifts.
Materials and Methods
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Results
Get Radiology Tree app to read full this article<
Table 1
Results of Univariate and Multivariate Risk Factor Analyses for Major Discrepancies
Univariate Analysis Major Discrepancy ( n = 79) Concordant ( n = 7983)P ∗ Examination characteristic Hours into shift (median) 6.83 6.53 .176 † <2 5.06% 6.96% .508 2 to <4 15.19% 15.17% .996 4 to <6 16.46% 22.36% .210 6 to <8 15.19% 19.68% .318 8 to <10 15.19% 20.02% .290 10 to <12 29.11% 14.56% <.001 Imaging modality Conventional radiography 29.11% 68.08% <.001 Computed tomography (CT) 59.49% 25.32% <.001 Ultrasound US) 11.39% 6.60% .089 Cross-sectional (CT or US) 70.89% 31.92% <.001 Patient characteristics Age, y (median) 52.08 51.58 .710 † Male gender 43.04% 46.86% .498 Inpatient 21.52% 19.87% .714 Shift characteristics Examinations per shift 50 52 .158 † ≤25 8.86% 4.74% .103 ‡ 26–50 41.77% 42.99% .828 51–75 43.04% 41.29% .753 >75 6.33% 4.82% .281 ‡ Weekend shift 35.44% 34.82% .909
Logistic Regression Regression Coefficient_P_ Odds Ratio (95% Confidence Interval) Exam characteristic Hours 10 to <12 0.665 .009 1.94 (1.18–3.21) Cross-sectional modality 1.682 <.001 5.38 (3.22–8.98) Patient characteristics Age, y −0.00006 .893 1.00 (0.99–1.01) § Male gender −0.044 .849 0.97 (0.61–1.51) Inpatient location 0.593 .042 1.81 (1.02–3.20) Shift characteristics Examinations per shift −0.005 .455 1.00 (0.98–1.01) § Weekend 0.212 .412 1.24 (0.75–2.05)
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Discussion
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
References
1. Laine C., Goldman L., Soukup J.R., et. al.: The impact of a regulation restricting medical house staff working hours on the quality of patient care. JAMA 1993; 269: pp. 374-378.
2. ACGME Duty Hours Standards Fact Sheet. 2003. (Accessed January 10, 2011, at http://www.acgme.org/acWebsite/newsRoom/newsRm_dutyHours.asp .)
3. Arnedt J.T., Owens J., Crouch M., et. al.: Neurobehavioral performance of residents after heavy night call vs after alcohol ingestion. JAMA 2005; 294: pp. 1025-1033.
4. Bartel P., Offermeier W., Smith F., et. al.: Attention and working memory in resident anaesthetists after night duty: group and individual effects. Occup Environ Med 2004; 61: pp. 167-170.
5. Ayalon R.D., Friedman F.: The effect of sleep deprivation on fine motor coordination in obstetrics and gynecology residents. Am J Obstet Gynecol 2008; 199: pp. 576.e1-576.e5.
6. Halbach M.M., Spann C.O., Egan G.: Effect of sleep deprivation on medical resident and student cognitive function: A prospective study. Am J Obstet Gynecol 2003; 188: pp. 1198-1201.
7. Hawkins M.R., Vichick D.A., Silsby H.D., et. al.: Sleep and nutritional deprivation and performance of house officers. J Med Educ 1985; 60: pp. 530-535.
8. Kahol K., Leyba M.J., Deka M., et. al.: Effect of fatigue on psychomotor and cognitive skills. Am J Surg 2008; 195: pp. 195-204.
9. Leonard C., Fanning N., Attwood J., et. al.: The effect of fatigue, sleep deprivation and onerous working hours on the physical and mental wellbeing of pre-registration house officers. Ir J Med Sci 1998; 167: pp. 22-25.
10. Lingenfelser T., Kaschel R., Weber A., et. al.: Young hospital doctors after night duty: their task-specific cognitive status and emotional condition. Med Educ 1994; 28: pp. 566-572.
11. Lockley S.W., Cronin J.W., Evans E.E., et. al.: Effect of reducing interns’ weekly work hours on sleep and attentional failures. N Engl J Med 2004; 351: pp. 1829-1837.
12. Robbins J., Gottlieb F.: Sleep deprivation and cognitive testing in internal medicine house staff. West J Med 1990; 152: pp. 82-86.
13. Mainiero M.B., Davis L.P., Chertoff J.D.: Resident duty hour limits: recommendations by the IOM and the response from the radiology community. J Am Coll Radiol 2010; 7: pp. 56-60.
14. Itri J.N., Kim W., Scanlon M.H.: Orion: a web-based application designed to monitor resident and fellow performance on-call. J Digit Imaging 2011; 24: pp. 897-907.
15. Ruutiainen A.T., Scanlon M.H., Itri J.N.: Identifying benchmarks for discrepancy rates in preliminary interpretations provided by radiology trainees at an academic institution. J Am Coll Radiol 2011; 8: pp. 644-648.
16. Itri J.N., Redfern R.O., Scanlon M.H.: Using a web-based application to enhance resident training and improve performance on-call. Acad Radiol 2010; 17: pp. 917-920.
17. Barger L.K., Lockley S.W., Rajaratnam S.M., et. al.: Neurobehavioral, health, and safety consequences associated with shift work in safety-sensitive professions. Curr Neurol Neurosci Rep 2009; 9: pp. 155-164.
18. Hendey G.W., Barth B.E., Soliz T.: Overnight and postcall errors in medication orders. Acad Emerg Med 2005; 12: pp. 629-634.
19. Horwitz L.I., Kosiborod M., Lin Z., et. al.: Changes in outcomes for internal medicine inpatients after work-hour regulations. Ann Intern Med 2007; 147: pp. 97-103.
20. Frankel H.L., Foley A., Norway C., et. al.: Amelioration of increased intensive care unit service readmission rate after implementation of work-hour restrictions. J Trauma 2006; 61: pp. 116-121.
21. Landrigan C.P., Rothschild J.M., Cronin J.W., et. al.: Effect of reducing interns’ work hours on serious medical errors in intensive care units. N Engl J Med 2004; 351: pp. 1838-1848.
22. Gopaldas R.R., Huh J., Bakaeen F.G., et. al.: The impact of resident work-hour restrictions on outcomes of cardiac operations. J Surg Res 2009; 157: pp. 268-274.
23. Morrison C.A., Wyatt M.M., Carrick M.M.: Impact of the 80-hour work week on mortality and morbidity in trauma patients: an analysis of the National Trauma Data Bank. J Surg Res 2009; 154: pp. 157-162.
24. Privette A.R., Shackford S.R., Osler T., et. al.: Implementation of resident work hour restrictions is associated with a reduction in mortality and provider-related complications on the surgical service: a concurrent analysis of 14,610 patients. Ann Surg 2009; 250: pp. 316-321.
25. Shetty K.D., Bhattacharya J.: Changes in hospital mortality associated with residency work-hour regulations. Ann Intern Med 2007; 147: pp. 73-80.
26. Volpp K.G., Rosen A.K., Rosenbaum P.R., et. al.: Mortality among patients in VA hospitals in the first 2 years following ACGME resident duty hour reform. JAMA 2007; 298: pp. 984-992.
27. Bailit J.L., Blanchard M.H.: The effect of house staff working hours on the quality of obstetric and gynecologic care. Obstet Gynecol 2004; 103: pp. 613-616.
28. Davydov L., Caliendo G., Mehl B., et. al.: Investigation of correlation between house-staff work hours and prescribing errors. Am J Health Syst Pharm 2004; 61: pp. 1130-1134.
29. de Virgilio C., Yaghoubian A., Lewis R.J., et. al.: The 80-hour resident workweek does not adversely affect patient outcomes or resident education. Curr Surg 2006; 63: pp. 435-439. discussion 40
30. Ellman P.I., Kron I.L., Alvis J.S., et. al.: Acute sleep deprivation in the thoracic surgical resident does not affect operative outcomes. Ann Thorac Surg 2005; 80: pp. 60-64. discussion 4-5
31. Howard D.L., Silber J.H., Jobes D.R.: Do regulations limiting residents’ work hours affect patient mortality?. J Gen Intern Med 2004; 19: pp. 1-7.
32. Kaafarani H.M., Itani K.M., Petersen L.A., et. al.: Does resident hours reduction have an impact on surgical outcomes?. J Surg Res 2005; 126: pp. 167-171.
33. Landrigan C.P., Fahrenkopf A.M., Lewin D., et. al.: Effects of the accreditation council for graduate medical education duty hour limits on sleep, work hours, and safety. Pediatrics 2008; 122: pp. 250-258.
34. Mycyk M.B., McDaniel M.R., Fotis M.A., et. al.: Hospitalwide adverse drug events before and after limiting weekly work hours of medical residents to 80. Am J Health Syst Pharm 2005; 62: pp. 1592-1595.
35. Poulose B.K., Ray W.A., Arbogast P.G., et. al.: Resident work hour limits and patient safety. Ann Surg 2005; 241: pp. 847-856. discussion 56-60
36. Rosen A.K., Loveland S.A., Romano P.S., et. al.: Effects of resident duty hour reform on surgical and procedural patient safety indicators among hospitalized Veterans Health Administration and Medicare patients. Med Care 2009; 47: pp. 723-731.
37. Schenarts P., Bowen J., Bard M., et. al.: The effect of a rotating night-float coverage scheme on preventable and potentially preventable morbidity at a level 1 trauma center. Am J Surg 2005; 190: pp. 147-152.
38. Volpp K.G., Rosen A.K., Rosenbaum P.R., et. al.: Did duty hour reform lead to better outcomes among the highest risk patients?. J Gen Intern Med 2009; 24: pp. 1149-1155.
39. Salim A., Teixeira P.G., Chan L., et. al.: Impact of the 80-hour workweek on patient care at a level I trauma center. Arch Surg 2007; 142: pp. 708-712. discussion 12-4
40. Fisman D.N., Harris A.D., Rubin M., et. al.: Fatigue increases the risk of injury from sharp devices in medical trainees: results from a case-crossover study. Infect Control Hosp Epidemiol 2007; 28: pp. 10-17.
41. Green-McKenzie J., Shofer F.S.: Duration of time on shift before accidental blood or body fluid exposure for housestaff, nurses, and technicians. Infect Control Hosp Epidemiol 2007; 28: pp. 5-9.
42. Davenport M.S., Ellis J.H., Khalatbari S.H., et. al.: Effect of work hours, caseload, shift type, and experience on resident call performance. Acad Radiol 2010; 17: pp. 921-927.
43. Shah N.A., Hoch M., Willis A., et. al.: Correlation among on-call resident study volume, discrepancy rate, and turnaround time. Acad Radiol 2010; 17: pp. 1190-1194.
44. Chan S.: What factors affect the discrepancy rate between preliminary resident interpretations of neuroimaging studies and the final attending interpretation?. Acad Radiol 2008; 15: pp. 817-819.
45. Summary of Hours-of-Service (HOS) Regulations. U.S. Department of Transportation Federal Motor Carrier Safety Administration, 2012. (Accessed May 6th, 2012, at http://www.fmcsa.dot.gov/rules-regulations/topics/hos/index.htm .)
46. VanDongen H., Dinges D.: Circadian rhythms in sleepiness, alertness, and performance.Kryger M.Roth T.Dement W.Principles and Practice of Sleep Medicine.2005.Elsevier SaundersPhiladelphia:pp. 435-443.
47. Reed D.A., Fletcher K.E., Arora V.M.: Systematic review: association of shift length, protected sleep time, and night float with patient care, residents’ health, and education. Ann Intern Med 2010; 153: pp. 829-842.
48. Mann F.A., Danz P.L.: The night stalker effect: quality improvements with a dedicated night-call rotation. Invest Radiol 1993; 28: pp. 92-96.
49. Krupinski E.A., Berbaum K.S., Caldwell R.T., et. al.: Long radiology workdays reduce detection and accommodation accuracy. J Am Coll Radiol 2010; 7: pp. 698-704.
50. Krupinski E.A., Berbaum K.S., Caldwell R.T., et. al.: Do long radiology workdays affect nodule detection in dynamic CT interpretation?. J Am Coll Radiol 2012; 9: pp. 191-198.
51. Chung J.H., Strigel R.M., Chew A.R., et. al.: Overnight resident interpretation of torso CT at a level 1 trauma center an analysis and review of the literature. Acad Radiol 2009; 16: pp. 1155-1160.
52. Sun G.W., Shook T.L., Kay G.L.: Inappropriate use of bivariable analysis to screen risk factors for use in multivariable analysis. J Clin Epidemiol 1996; 49: pp. 907-916.
53. Borgstede J.P., Lewis R.S., Bhargavan M., et. al.: RADPEER quality assurance program: a multifacility study of interpretive disagreement rates. J Am Coll Radiol 2004; 1: pp. 59-65.
54. Siegle R.L., Baram E.M., Reuter S.R., et. al.: Rates of disagreement in imaging interpretation in a group of community hospitals. Acad Radiol 1998; 5: pp. 148-154.
55. Robinson P.J.: Radiology’s Achilles’ heel: error and variation in the interpretation of the Rontgen image. Br J Radiol 1997; 70: pp. 1085-1098.
56. Robinson P.J., Wilson D., Coral A., et. al.: Variation between experienced observers in the interpretation of accident and emergency radiographs. Br J Radiol 1999; 72: pp. 323-330.
57. Carney E., Kempf J., DeCarvalho V., et. al.: Preliminary interpretations of after-hours CT and sonography by radiology residents versus final interpretations by body imaging radiologists at a level 1 trauma center. AJR Am J Roentgenol 2003; 181: pp. 367-373.
58. Cooper V.F., Goodhartz L.A., Nemcek A.A., et. al.: Radiology resident interpretations of on-call imaging studies: the incidence of major discrepancies. Acad Radiol 2008; 15: pp. 1198-1204.
59. Erly W.K., Berger W.G., Krupinski E., et. al.: Radiology resident evaluation of head CT scan orders in the emergency department. AJNR Am J Neuroradiol 2002; 23: pp. 103-107.
60. Meyer R.E., Nickerson J.P., Burbank H.N., et. al.: Discrepancy rates of on-call radiology residents’ interpretations of CT angiography studies of the neck and circle of Willis. AJR Am J Roentgenol 2009; 193: pp. 527-532.
61. Ruchman R.B., Jaeger J., Wiggins E.F., et. al.: Preliminary radiology resident interpretations versus final attending radiologist interpretations and the impact on patient care in a community hospital. AJR Am J Roentgenol 2007; 189: pp. 523-526.
62. Tieng N., Grinberg D., Li S.F.: Discrepancies in interpretation of ED body computed tomographic scans by radiology residents. Am J Emerg Med 2007; 25: pp. 45-48.
63. Walls J., Hunter N., Brasher P.M., et. al.: The DePICTORS Study: discrepancies in preliminary interpretation of CT scans between on-call residents and staff. Emerg Radiol 2009; 16: pp. 303-308.
64. Wechsler R.J., Spettell C.M., Kurtz A.B., et. al.: Effects of training and experience in interpretation of emergency body CT scans. Radiology 1996; 199: pp. 717-720.
65. Lal N.R., Murray U.M., Eldevik O.P., et. al.: Clinical consequences of misinterpretations of neuroradiologic CT scans by on-call radiology residents. AJNR Am J Neuroradiol 2000; 21: pp. 124-129.