Rationale and Objectives
Cardiovascular (CV) disease is predominately influenced by CV risk factors and coronary computed tomography angiography (CTA) is capable of detecting early-stage coronary artery disease. We sought to determine the influence of CV risk factors on the prevalence of nonobstructive atherosclerosis in patients with normal-appearing coronary arteries in invasive coronary angiography (ICA).
Materials and Methods
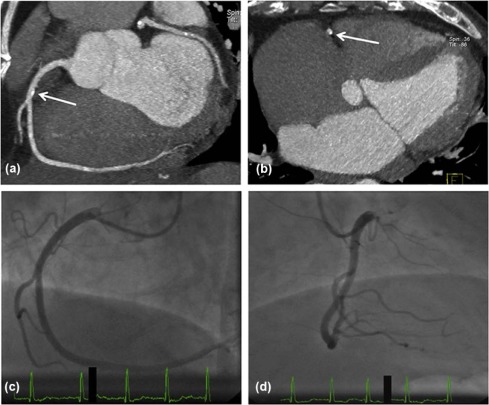
In this retrospective analysis, we included 60 consecutive symptomatic patients, having undergone ICA and coronary CTA. Coronary dual source CTA was performed using electrocardiogram-triggered retrospective gated image acquisition at 40%–70% of RR interval (tube voltage 100–120 kV, tube current time product 320–440 mAs, 60 mL contrast, and flow rate 6 mL/s).
Results
Out of 60 patients (32 men, mean age 61 ± 11 years) with a normal coronary artery appearance in ICA, 45 (75%) patients showed atherosclerotic plaque in CTA. Plaque was present in 14 of 60 (23%) left main, 41 of 60 (68%) left anterior descending, 21 of 60 (35%) circumflex coronary arteries, and 24 of 60 (40%) right coronary arteries. More than 15% of all coronary artery segments showed detectable plaques. Interobserver agreement ranged from good to very good on a per-patient, per-vessel, and per-segment level. Patients with presence of plaque were significantly older ( P = 0.005) and showed higher incidence of arterial hypertension ( P = 0.019) as compared to individuals without coronary plaque in dual source computed tomography.
Conclusions
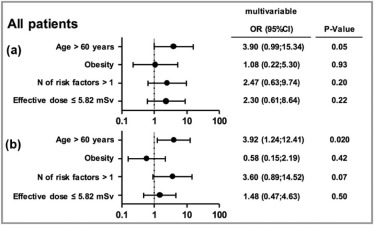
The prevalence of coronary atherosclerosis by CTA is substantial in symptomatic patients with normal invasive coronary angiogram. Hypertension and older age significantly influence the prevalence of atherosclerotic plaque and highlight the importance of risk-modifying therapy.
Introduction
Cardiovascular (CV) risk factors are widely used for risk assessment and direction of medical management in patients with suspected coronary heart disease. In patients with known coronary artery disease (CAD), strict risk factor control is crucial .
Coronary computed tomography angiography (CTA) can detect coronary artery stenosis noninvasively with excellent diagnostic accuracy and hence is successfully used to predict prognosis . Importantly, not only obstructive CAD increases the risk of all-cause mortality. There are substantial data consistently demonstrating a significant increase in risk for major adverse cardiac events (MACE) with increasing burden of atherosclerotic disease in CTA . Clinical relevance to detect even small amounts of coronary artery calcification (CAC), for instance, has been demonstrated by the Multi-Ethnic Study of Atherosclerosis (MESA), as individuals with CAC have significantly (threefold) increased risk for future cardiac events . It is also known that CAC has not only strong incremental value to predict cardiac events but also provides independent information in addition to traditional risk factors . The identification of nonobstructive, noncalcified lesions by CTA has also been shown to be of prognostic value . In 10,418 patients undergoing CTA, the international multicenter registry, CONFIRM, found a 6% higher risk of mortality for each additional segment with nonobstructive atherosclerotic plaque ( P = 0.021). Moreover, in patients with nonobstructive CAD, baseline statin use was associated with a 56% decreased mortality risk (hazard ratio 0.44) compared to patients without statin therapy. Statin use at baseline did not decrease the risk in patients without plaque in CTA .
Get Radiology Tree app to read full this article<
Materials and Methods
Study Design and Patient Population
Get Radiology Tree app to read full this article<
DSCT Data Acquisition and Image Analysis
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Analysis of Coronary Atherosclerosis
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Statistical Analyses
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Results
Patient and DSCT Scan Characteristics
Get Radiology Tree app to read full this article<
TABLE 1
Patient and Scan Characteristics
Mean ± SD or n (%) Patients characteristics Age (years) 61 ± 11 Male gender 32(53) Weight(kg) 80 ± 14 Height(m) 1.7 ± 0.1 BMI(kg/m 2 ) 28.0 ± 4.4 Obesity 15(25) Cardiovascular risk factors Hypertension 39(65) Diabetes mellitus 3(5) Smoker, current or prior 28(47) Familial history 17(28) Hyperlipidemia 39(65) Number of risk factors 2.1 ± 1.0 Scan parameters Tube voltage(100 kV) 39(65) Tube voltage(120 kV) 21(35) Tube current time product(mAs) 371 ± 60 CTDI(mGy) 37.4 ± 46.0 DLP(mGy∙cm) 450 ± 282 Effective dose(mSv) 6.3 ± 3.9
BMI, body mass index; CTDI, computed tomography dose index; DLP, dose length product; SD, standard deviation.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Interobserver Differences for Plaque Detection
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
TABLE 2
Segment-Based Analysis
Group Number of Diseased Segments Per Patient Number of Patients Number of Segments With Plaque Interobserver Differences 1 0 15 0 2 1–5 35 94 2 3 >5 10 69 10Total6016312
Number of computed tomography angiographically detected segments with any plaque.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
TABLE 3
Vessel-Based Analysis
O2 O1 No Plaque NCP CP MixedCoronary arteriesLM (PdV: 23.3%; PcV: 15.0%; κ: 0.83 [CI 0.67–0.99]) No plaque 46 0 0 0 NCP 0 5 0 0 CP 0 0 2 3 Mixed 0 0 1 3LAD (PdV: 68.3%; PcV: 41.7%; κ: 0.93 [CI 0.84–1.00]) No plaque 19 0 0 0 NCP 0 16 0 0 CP 0 0 0 3 Mixed 0 0 0 22LCX (PdV: 35.0%; PcV: 18.3%; κ: 0.97 [CI 0.91–1.00]) No plaque 38 1 0 0 NCP 0 10 0 0 CP 0 0 2 0 Mixed 0 0 0 9RCA (PdV: 40.0%; PcV: 20.0%; κ: 0.91 [CI 0.82–1.00]) No plaque 35 1 0 0 NCP 0 12 0 0 CP 0 0 1 2 Mixed 0 0 0 9Total All (PdV: 41.7%; PcV: 23.8%; κ: 0.92 [CI 0.87–0.97]) No Plaque NCP CP MixedSum No plaque 138 2 0 0 140 NCP 0 43 0 0 43 CP 0 0 5 8 13 Mixed 0 0 1 43 44Sum 138 45 6 51 240
No Plaque, disease-free condition; NCP, exclusively noncalcified plaque; CP, exclusively calcified plaque; Mixed, mixed plaque; LM, left main coronary artery; LAD, left anterior descending coronary artery; LCX, left circumflex coronary artery; RCA, right coronary artery; O1, Observer 1 (columns); O2, Observer 2 (rows); PcV, percentage of exclusively or partly calcified vessels; PdV, percentage of diseased vessels.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Segment-Based Analysis
Get Radiology Tree app to read full this article<
Vessel-Based Analysis
Get Radiology Tree app to read full this article<
Patient-Based Analysis
Get Radiology Tree app to read full this article<
TABLE 4
Patient-Based Analysis with Regard to (a) Plaque Composition and (b) Number of Affected Vessels
(a) Plaque Composition O2 O1 No Plaque NCP CP Mixed No plaque 15 0 0 0 NCP 0 16 0 0 CP 0 0 0 0 Mixed 0 0 0 29
(b) Number of Affected Vessels Per Patient O2 O1 0 1 2 3 0 15 0 0 0 1 0 16 2 0 2 0 0 9 0 3 0 0 0 18
No Plaque, disease-free condition; NCP, exclusively noncalcified plaque; CP, exclusively calcified plaque; Mixed, mixed plaque; O1, Observer 1 (columns); O2, Observer 2 (rows).
Values in diagonals represent number of patients without differences between both observers.
Get Radiology Tree app to read full this article<
Influence of CV Risk Factors
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Discussion
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Limitations
Get Radiology Tree app to read full this article<
Conclusion
Get Radiology Tree app to read full this article<
Supplementary Data
Get Radiology Tree app to read full this article<
Table S1
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
References
1. Perk J., De Backer G., Gohlke H., et. al.: European Guidelines on cardiovascular disease prevention in clinical practice (version 2012). The Fifth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of nine societies and by invited experts). Eur Heart J 2012; 33: pp. 1635-1701.
2. Montalescot G., Sechtem U., Achenbach S., et. al.: 2013 ESC guidelines on the management of stable coronary artery disease: the Task Force on the management of stable coronary artery disease of the European Society of Cardiology. Eur Heart J 2013; 34: pp. 2949-3003.
3. Budoff M.J., Dowe D., Jollis J.G., et. al.: Diagnostic performance of 64-multidetector row coronary computed tomographic angiography for evaluation of coronary artery stenosis in individuals without known coronary artery disease: results from the prospective multicenter ACCURACY (Assessment by Coronary Computed Tomographic Angiography of Individuals Undergoing Invasive Coronary Angiography) trial. J Am Coll Cardiol 2008; 52: pp. 1724-1732.
4. Miller J.M., Rochitte C.E., Dewey M., et. al.: Diagnostic performance of coronary angiography by 64-row CT. N Engl J Med 2008; 359: pp. 2324-2336.
5. Meijboom W.B., Meijs M.F., Schuijf J.D., et. al.: Diagnostic accuracy of 64-slice computed tomography coronary angiography: a prospective, multicenter, multivendor study. J Am Coll Cardiol 2008; 52: pp. 2135-2144.
6. Ostrom M.P., Gopal A., Ahmadi N., et. al.: Mortality incidence and the severity of coronary atherosclerosis assessed by computed tomography angiography. J Am Coll Cardiol 2008; 52: pp. 1335-1343.
7. Hadamitzky M., Freissmuth B., Meyer T., et. al.: Prognostic value of coronary computed tomographic angiography for prediction of cardiac events in patients with suspected coronary artery disease. JACC Cardiovasc Imaging 2009; 2: pp. 404-411.
8. Kwon S.W., Kim Y.J., Shim J., et. al.: Coronary artery calcium scoring does not add prognostic value to standard 64-section CT angiography protocol in low-risk patients suspected of having coronary artery disease. Radiology 2011; 259: pp. 92-99.
9. Min J.K., Shaw L.J., Devereux R.B., et. al.: Prognostic value of multidetector coronary computed tomographic angiography for prediction of all-cause mortality. J Am Coll Cardiol 2007; 50: pp. 1161-1170.
10. Abdulla J., Asferg C., Kofoed K.F.: Prognostic value of absence or presence of coronary artery disease determined by 64-slice computed tomography coronary angiography a systematic review and meta-analysis. Int J Cardiovasc Imaging 2011; 27: pp. 413-420.
11. Habib P.J., Green J., Butterfield R.C., et. al.: Association of cardiac events with coronary artery disease detected by 64-slice or greater coronary CT angiography: a systematic review and meta-analysis. Int J Cardiol 2013; 169: pp. 112-120.
12. Min J.K., Dunning A., Lin F.Y., et. al.: Age- and sex-related differences in all-cause mortality risk based on coronary computed tomography angiography findings results from the International Multicenter CONFIRM (Coronary CT Angiography Evaluation for Clinical Outcomes: an International Multicenter Registry) of 23,854 patients without known coronary artery disease. J Am Coll Cardiol 2011; 58: pp. 849-860.
13. Budoff M.J., McClelland R.L., Nasir K., et. al.: Cardiovascular events with absent or minimal coronary calcification: the Multi-Ethnic Study of Atherosclerosis (MESA). Am Heart J 2009; 158: pp. 554-561.
14. Detrano R., Guerci A.D., Carr J.J., et. al.: Coronary calcium as a predictor of coronary events in four racial or ethnic groups. N Engl J Med 2008; 358: pp. 1336-1345.
15. Budoff M.J., Shaw L.J., Liu S.T., et. al.: Long-term prognosis associated with coronary calcification: observations from a registry of 25,253 patients. J Am Coll Cardiol 2007; 49: pp. 1860-1870.
16. Puchner S.B., Liu T., Mayrhofer T., et. al.: High-risk plaque detected on coronary CT angiography predicts acute coronary syndromes independent of significant stenosis in acute chest pain: results from the ROMICAT-II trial. J Am Coll Cardiol 2014; 64: pp. 684-692.
17. Chow B.J., Small G., Yam Y., et. al.: Prognostic and therapeutic implications of statin and aspirin therapy in individuals with nonobstructive coronary artery disease: results from the CONFIRM (COronary CT Angiography EvaluatioN For Clinical Outcomes: an InteRnational Multicenter registry) registry. Arterioscler Thromb Vasc Biol 2015; 35: pp. 981-989.
18. Raff G.L., Abidov A., Achenbach S., et. al.: SCCT guidelines for the interpretation and reporting of coronary computed tomographic angiography. J Cardiovasc Comput Tomogr 2009; 3: pp. 122-136.
19. Altman D.: Practical statistics for medical research.1991.Chapman and HallLondon
20. Pundziute G., Schuijf J.D., Jukema J.W., et. al.: Prognostic value of multislice computed tomography coronary angiography in patients with known or suspected coronary artery disease. J Am Coll Cardiol 2007; 49: pp. 62-70.
21. Hulten E.A., Carbonaro S., Petrillo S.P., et. al.: Prognostic value of cardiac computed tomography angiography: a systematic review and meta-analysis. J Am Coll Cardiol 2011; 57: pp. 1237-1247.
22. Schlett C.L., Banerji D., Siegel E., et. al.: Prognostic value of CT angiography for major adverse cardiac events in patients with acute chest pain from the emergency department: 2-year outcomes of the ROMICAT trial. JACC Cardiovasc Imaging 2011; 4: pp. 481-491.
23. Kim M.S., Kang S.J., Lee C.W., et. al.: Prevalence of coronary atherosclerosis in asymptomatic healthy subjects: an intravascular ultrasound study of donor hearts. J Atheroscler Thromb 2013; 20: pp. 465-471.
24. Tuzcu E.M., Kapadia S.R., Tutar E., et. al.: High prevalence of coronary atherosclerosis in asymptomatic teenagers and young adults: evidence from intravascular ultrasound. Circulation 2001; 103: pp. 2705-2710.
25. Stone G.W., Maehara A., Lansky A.J., et. al.: A prospective natural-history study of coronary atherosclerosis. N Engl J Med 2011; 364: pp. 226-235.
26. Voros S., Rinehart S., Qian Z., et. al.: Coronary atherosclerosis imaging by coronary CT angiography: current status, correlation with intravascular interrogation and meta-analysis. JACC Cardiovasc Imaging 2011; 4: pp. 537-548.
27. Fischer C., Hulten E., Belur P., et. al.: Coronary CT angiography versus intravascular ultrasound for estimation of coronary stenosis and atherosclerotic plaque burden: a meta-analysis. J Cardiovasc Comput Tomogr 2013; 7: pp. 256-266.
28. Lichtlen P.R., Bargheer K., Wenzlaff P.: Long-term prognosis of patients with anginalike chest pain and normal coronary angiographic findings. J Am Coll Cardiol 1995; 25: pp. 1013-1018.