Rationale and Objectives
Magnetic resonance–guided high-intensity focused ultrasound (MR-HIFU) ablation of tumors in the liver dome is challenging because of the presence of air in the costophrenic angle. In this study, we used a porcine liver model and a clinical MR-HIFU system to assess the feasibility and safety of using intrapleural fluid infusion (IPI) to create an acoustic window for MR-HIFU ablation in the liver dome.
Materials and Methods
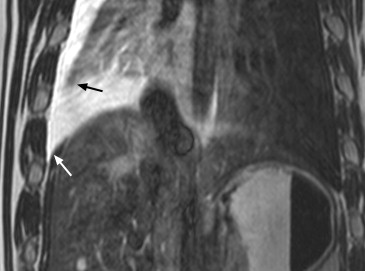
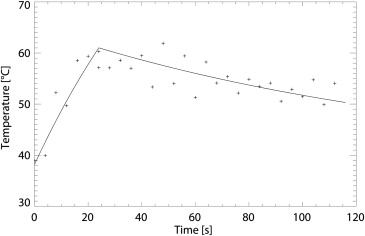
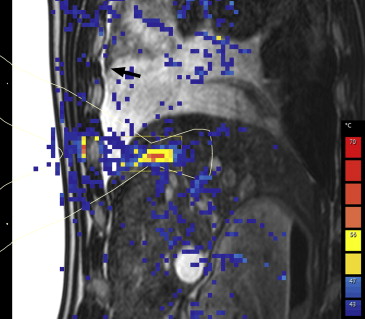
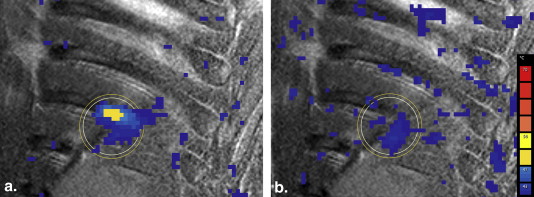
Healthy adult Dalland land pigs ( n = 6) under general anesthesia were used with animal committee approval. Degassed saline (200–800 mL) was infused into the intrapleural space under ultrasound guidance. A clinical 1.5-T MR-HIFU system was used to perform sonications (4-mm treatment cells, 300–450 W, 20–30 seconds) in the liver dome under real-time MR thermometry. An intercostal firing technique was used to prevent rib heating in one experiment. Technical success was defined as a temperature increase (>10°C) in the target area. After termination, the animal was examined for thermal damage to liver, diaphragm, pleura, lung, or intercostal muscle.
Results
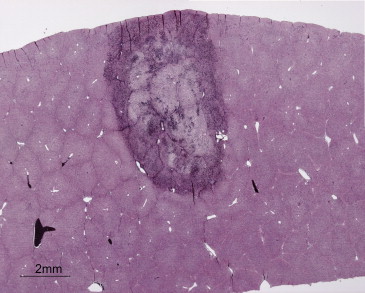
An acoustic window was established in all animals. A temperature increase in the target area was achieved in all animals (max. 47°C–67°C). MR thermometry showed no heating outside the target area. Intercostal firing effectively reduced rib heating (55°C vs. 42°C). Postmortem examination revealed no unwanted thermal damage. One complication occurred, in the first experiment, because of an ill-suited needle (displacement of the needle).
Conclusions
The results indicate that IPI may be used safely to assist MR-HIFU ablation of tumors in the liver dome. For reliable tissue coagulation, IPI must be combined with an intercostal sonication technique. Considering the proportion of patients with tumors in the liver dome, IPI widens the applicability of MR-HIFU ablation for liver tumors considerably.
Magnetic resonance–guided high-intensity focused ultrasound (MR-HIFU) is an image-guided, noninvasive, thermal ablation technique which allows for precisely targeted tumor ablation while sparing the surrounding healthy tissue. The MR guidance provides near real-time image guidance and temperature feedback during ablation . MR-HIFU is used clinically for the treatment of uterine fibroids and bone metastases and is currently under investigation for several other oncologic applications such as ablation of prostate, pancreas, breast, and liver tumors and for targeted drug delivery .
For clinical implementation of MR-HIFU ablation of liver tumors, several organ-specific challenges have to be overcome . One of these challenges is the fact that the lung overlaps the liver dome, which is the cranial subdiaphragmatic part of the liver in the costophrenic angle (or costodiaphragmatic recess). This air–tissue interface forms an impassable barrier for the ultrasound beam, preventing ablation of tumors in the liver dome. To overcome this challenge, the use of intrapleural fluid infusion (IPI) has been proposed. This creates an acoustic window by infusing fluid into the costophrenic angle. This strategy has been reported for low-intensity diagnostic ultrasound guidance of percutaneous ablation procedures in the liver dome (eg, during radiofrequency [RF] ablation) . The use of IPI in combination with ultrasound-guided HIFU has been reported; however, to the best of our knowledge, no studies have been reported which were dedicated to the IPI technique, in particular not with real-time MR thermometry .
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Materials and methods
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Results
Intrapleural Fluid Infusion
Get Radiology Tree app to read full this article<
Table 1
Overview of the Experiments
Animal Infused Fluid Volume Needle Complications Acoustic Window Respiratory Compensation Intercostal Firing Technique Number of Sonications Distance Focal Point—Diaphragm, mm Peak Temperature Animal 1 ∼200 mL Venous catheter Fluid in intercostal muscle Sufficient Breath hold No 6 8 67°C Animal 2 ∼750 mL Veress No Good Breath hold No 4 5 65°C Animal 3 ∼800 mL Veress No Good Breath hold No 6 7 47°C ∗ Animal 4 ∼800 mL Veress No Good Respiratory gated No 7 4 55°C Animal 5 ∼800 mL Veress No Good Respiratory gated No 4 6 62°C Animal 6 ∼700 mL Veress No Good Respiratory gated Yes 4 11 59°C
The quality of the acoustic window depended mostly on displacement of the right lower lung lobe.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
MR-HIFU Procedures
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Discussion
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
References
1. Hynynen K., Freund W.R., Cline H.E., et. al.: A clinical, noninvasive, MR imaging-monitored ultrasound surgery method. Radiographics 1996; 16: pp. 185-195.
2. Hwang J.H., Wang Y.N., Warren C., et. al.: Preclinical in vivo evaluation of an extracorporeal HIFU device for ablation of pancreatic tumors. Ultrasound Med Biol 2009; 35: pp. 967-975.
3. Schmitz A.C., Gianfelice D., Daniel B.L., et. al.: Image-guided focused ultrasound ablation of breast cancer: current status, challenges, and future directions. Eur Radiol 2008; 18: pp. 1431-1441.
4. Liu H.L., Yang H.W., Hua M.Y., et. al.: Enhanced therapeutic agent delivery through magnetic resonance imaging-monitored focused ultrasound blood-brain barrier disruption for brain tumor treatment: an overview of the current preclinical status. Neurosurg Focus 2012; 32: pp. E4.
5. Voogt M.J., Trillaud H., Kim Y.S., et. al.: Volumetric feedback ablation of uterine fibroids using magnetic resonance-guided high intensity focused ultrasound therapy. Eur Radiol 2012; 22: pp. 411-417.
6. Huisman M., van den Bosch M.A.: MR-guided high-intensity focused ultrasound for noninvasive cancer treatment. Cancer Imaging 2011; 11: pp. S161-S166.
7. Uchida T., Nakano M., Hongo S., et. al.: High-intensity focused ultrasound therapy for prostate cancer. Int J Urol 2012; 19: pp. 187-201.
8. Wijlemans J.W., Bartels L.W., Deckers R., et. al.: Magnetic resonance-guided high-intensity focused ultrasound (MR-HIFU) ablation of liver tumours. Cancer Imaging 2012; 12: pp. 387-394.
9. Shimada S., Hirota M., Beppu T., et. al.: A new procedure of percutaneous microwave coagulation therapy under artificial hydrothorax for patients with liver tumors in the hepatic dome. Surg Today 2001; 31: pp. 40-44.
10. Katayama K., Ooka Y., Uemura A., et. al.: Saline injection into the pleural cavity to detect tumors of the hepatic dome with sonography: a new approach for treatment of hepatocellular carcinoma. AJR Am J Roentgenol 2002; 179: pp. 102-104.
11. Cheung T.T., Chu F.S., Jenkins C.R., et. al.: Tolerance of high-intensity focused ultrasound ablation in patients with hepatocellular carcinoma. World J Surg 2012; 36: pp. 2420-2427.
12. Ng K.K., Poon R.T., Chan S.C., et. al.: High-intensity focused ultrasound for hepatocellular carcinoma: a single-center experience. Ann Surg 2011; 253: pp. 981-987.
13. Jung S.E., Cho S.H., Jang J.H., et. al.: High-intensity focused ultrasound ablation in hepatic and pancreatic cancer: complications. Abdom Imaging 2011; 36: pp. 185-195.
14. Louisnard O., González-García J.: Acoustic cavitation.Feng H.Barbosa-Canovas G.Weiss J.Ultrasound technologies for food and bioprocessing.2011.SpringerNew York:pp. 13-64.
15. Quesson B., Merle M., Köhler M.O., et. al.: A method for MRI guidance of intercostal high intensity focused ultrasound ablation in the liver. Med Phys 2010; 37: pp. 2533-2540.
16. Liu H.-L., Chang H., Chen W.-S., et. al.: Feasibility of transrib focused ultrasound thermal ablation for liver tumors using a spherically curved 2D array: a numerical study. Med Phys 2007; 34: pp. 3436-3448.
17. Sapareto S.A., Dewey W.C.: Thermal dose determination in cancer therapy. Int J Radiat Oncol Biol Phys 1984; 10: pp. 787-800.
18. Illing R.O., Kennedy J.E., Wu F., et. al.: The safety and feasibility of extracorporeal high-intensity focused ultrasound (HIFU) for the treatment of liver and kidney tumours in a Western population. Br J Cancer 2005; 93: pp. 890-895.
19. Kim J., Chung D.J., Jung S.E., et. al.: Therapeutic effect of high-intensity focused ultrasound combined with transarterial chemoembolisation for hepatocellular carcinoma <5 cm: comparison with transarterial chemoembolisation monotherapy—preliminary observations. Br J Radiol 2012; 85: pp. e940-e946.
20. Fukuno H., Tamaki K., Urata M., et. al.: Influence of an artificial pleural effusion technique on cardio-pulmonary function and autonomic activity. J Med Invest 2007; 54: pp. 48-53.
21. Koda M., Ueki M., Maeda Y., et. al.: Percutaneous sonographically guided radiofrequency ablation with artificial pleural effusion for hepatocellular carcinoma located under the diaphragm. AJR Am J Roentgenol 2004; 183: pp. 583-588.
22. Kondo Y., Yoshida H., Tateishi R., et. al.: Percutaneous radiofrequency ablation of liver cancer in the hepatic dome using the intrapleural fluid infusion technique. Br J Surg 2008; 95: pp. 996-1004.
23. Minami Y., Kudo M., Kawasaki T., et. al.: Percutaneous ultrasound-guided radiofrequency ablation with artificial pleural effusion for hepatocellular carcinoma in the hepatic dome. J Gastroenterol 2003; 38: pp. 1066-1070.
24. Grischuk. Archiv für Energiewirtschaft. 1957;11:136.
25. Wu C.C., Chen W.S., Ho M.C., et. al.: Minimizing abdominal wall damage during high-intensity focused ultrasound ablation by inducing artificial ascites. J Acoust Soc Am 2008; 124: pp. 674-679.
26. Laeseke P.F., Sampson L.A., Brace C.L., et. al.: Unintended thermal injuries from radiofrequency ablation: protection with 5% dextrose in water. AJR Am JRoentgenol 2006; 186: pp. S249-S254.