Rationale and Objectives
In this retrospective case series, we utilize arthroscopy as the gold standard to determine if magnetic resonance imaging (MRI) of the knee can predict osteochondritis dissecans (OCD) lesion stability, the most important information to guide patient treatment decisions. It is hypothesized that the classification system of the International Cartilage Repair Society (ICRS) will allow for improved assessment of lesion grade and stability in OCD.
Materials and Methods
Routine MRI studies of 46 consecutive patients with arthroscopically proven OCD lesions (mean age: 23.7 years; 26 male, 16 female) were assessed by three radiologists who were blinded to arthroscopic results. Arthroscopic images were evaluated by two orthopedic surgeons in consensus. The OCD criteria of the ICRS were applied to arthroscopy and imaging interpretations. Inter-rater correlation statistics and accuracy of magnetic resonance (MR) grading with respect to arthroscopy were determined.
Results
Only 56% of the available MR reports assigned a label of stable or unstable to the lesion description. Of these, 58% of the lesions were deemed unstable and 42% were stable. Accuracy was 53% when reports addressed stability. Utilizing the ICRS classification system, for all three readers combined, the respective sensitivity, specificity, and accuracy of MR imaging to determine lesion stability were 70%, 81%, and 76%. When compared to the original MRI report, the overall accuracy increased from 53% to 76% when readers were given the specific criteria of the OCD ICRS classification. However, inter-reader variability remained high, with Krippendorf’s alpha ranging from 0.48 to 0.57.
Conclusions
In this paper, we utilize arthroscopy as the gold standard to determine if MRI can predict OCD lesion stability, the most important information to guide patient treatment decisions. To our surprise, the analysis of the existing radiology reports that addressed stability revealed an overall accuracy in defining OCD lesion stability of about 53%. The classification system of the ICRS, created by an international multidisciplinary, multi-expert consortium, did markedly improve the accuracy, but consistency among different readers was lacking. This retrospective study on OCD reporting and classification highlights the inadequacy of existing classification schemes, and emphasizes the critical need for improved diagnostic MRI protocols in musculoskeletal radiology in order to propel it toward evidence-based medicine.
Introduction
Osteochondritis dissecans (OCD) is the term first utilized in 1887 to describe the occurrence of a progeny osteochondral fragment separated from the parent bone. The etiology remains controversial considering genetic , traumatic , and vascular causes . In the knee, OCD most commonly occurs in the central aspect of the medial femoral condyle, followed by the lateral femoral condyle, the trochlea, and the patella . Treatment of OCD largely depends on the presence or absence of stability of the progeny and the parent bone . Surgical fixation is recommended for stable OCD lesions that have failed nonoperative management, as well as for all unstable lesions .
There is a general consensus that OCD lesion stability is determined based on both clinical and radiological examinations . Magnetic resonance imaging (MRI) has been shown to be reliable in predicting the stability of OCD once a patient’s physis has closed . However, the same research has shown poor correlation between magnetic resonance (MR) findings and stability on arthroscopy prior to skeletal maturity . Another study concluded that MRI should not be used in isolation to assess lesion stability in juvenile OCD . Frequently, stability is not specifically assessed on preoperative imaging reports. This has left the preoperative diagnosis of stability to be heavily based on clinical rather than imaging findings .
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Materials and Methods
Study Design and Patient Selection
Get Radiology Tree app to read full this article<
MR Examination
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
TABLE 1
(A) MRI Grading of Osteochondral defects (ICRS Classification System for OCD Lesions) and (B) International Cartilage Repair Society (ICRS Classification System for OCD Lesions)
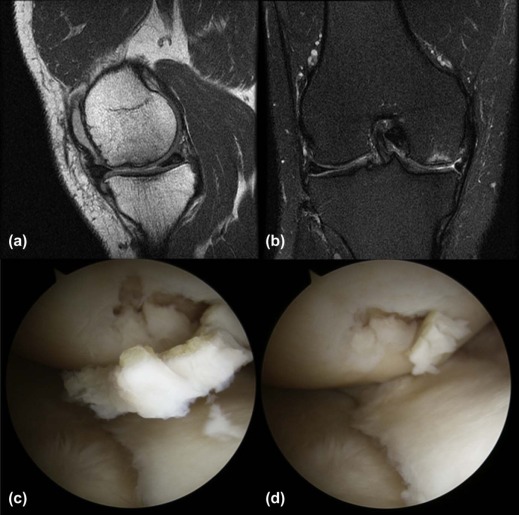
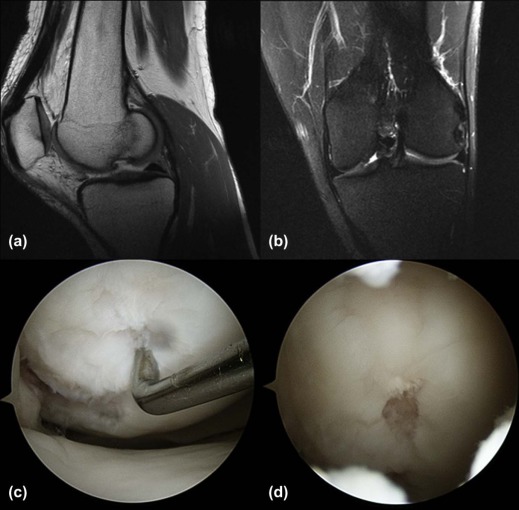
(A) Grade 1: Thickening of cartilage without disruption 1a: Bone marrow edema 1b: Fluid at lesion–bone interface Grade 2: Cartilage breached, fluid at interface, but not entire interface Grade 3: Cartilage completely disrupted with fluid interface surrounding lesion Grade 4: Displaced fragment Dipaola et al. (1991) (B) ICRS OCD I: Stable lesions with a continuous but softened area covered by intact cartilage ICRS OCD II (A with intact cartilage, B cartilage lesion): lesions with partial discontinuity at the lesion and bone interface that are stable when probed ICRS OCD III (A intact articular cartilage, B cartilage lesion): lesions with a complete discontinuity that are not yet dislocated (“dead in situ”) ICRS OCD IV: Empty defects and defects with a dislocated fragment or a loose fragment within the bed Brittberg and Winalski (2003)
MRI, magnetic resonance imaging; OCD, osteochondritis dissecans.
Get Radiology Tree app to read full this article<
Arthroscopic Evaluation
Get Radiology Tree app to read full this article<
Statistical Analysis
Get Radiology Tree app to read full this article<
Results
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
TABLE 2
Arthroscopic Grade Distribution
ICRS OCD I ICRS OCD IIA ICRS OCD IIB ICRS OCD IIIA ICRS OCD IIIB ICRS OCD IV 6 (52%) 1 (2%) 15 (36%) 0 (0%) 7 (17%) 13 (31%)
ICRS, International Cartilage Repair Society; OCD, osteochondritis dissecans.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
TABLE 3
Agreement Between MR Readers and Arthroscopy
MR Reader \* Agreement of Grade (Krippendorf’s Alpha) Agreement of Stability ( P -value) 1 0.52 [0.26–0.73] <0.01 2 0.60 [0.37–0.77] <0.01 3 0.68 [0.45–0.86] 0.065
MR, magnetic resonance; MSK, musculoskeletal.
Note: Numbers in brackets are 95% confidence intervals.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
TABLE 4
Inter-rater Agreement Between MR Readers
MR Readers \* Agreement of Grade (Krippendorf’s Alpha) 1 and 2 0.52 [0.25–0.74] 1 and 3 0.48 [0.19–0.72] 2 and 3 0.57 [0.32–0.74]
MR, magnetic resonance; MSK, musculoskeletal.
Note: Numbers in brackets are 95% confidence intervals.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Discussion
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Conclusions
Get Radiology Tree app to read full this article<
Acknowledgment
Get Radiology Tree app to read full this article<
References
1. König F.: Über freie Körper in den Gelenken. Dtsch Z Chir 1887; 27: pp. 90-109.
2. Edmonds E.W., Polousky J.: A review of knowledge in osteochondritis dissecans: 123 years of minimal evolution from Konig to the ROCK study group. Clin Orthop Relat Res 2013; 471: pp. 1118-1126.
3. Bates J.T., Jacobs J.C., Shea K.G., et. al.: Emerging genetic basis of osteochondritis dissecans. Clin Sports Med 2014; 33: pp. 199-220.
4. Polousky J.D.: Juvenile osteochondritis dissecans. Sports Med Arthrosc 2011; 19: pp. 56-63.
5. Shea K.G., Jacobs J.C., Grimm N.L., et. al.: Osteochondritis dissecans development after bone contusion of the knee in the skeletally immature: a case series. Knee Surg Sports Traumatol Arthrosc 2013; 21: pp. 403-407.
6. McCoy A.M., Toth F., Dolvik N.I., et. al.: Articular osteochondrosis: a comparison of naturally-occurring human and animal disease. Osteoarthritis Cartilage 2013; 21: pp. 1638-1647.
7. Linden B.: The incidence of osteochondritis dissecans in the condyles of the femur. Acta Orthop Scand 1976; 47: pp. 664-667.
8. Kocher M.S., Tucker R., Ganley T.J., et. al.: Management of osteochondritis dissecans of the knee: current concepts review. Am J Sports Med 2006; 34: pp. 1181-1191.
9. Pascual-Garrido C., Moran C.J., Green D.W., et. al.: Osteochondritis dissecans of the knee in children and adolescents. Curr Opin Pediatr 2013; 25: pp. 46-51.
10. Schulz J.F., Chambers H.G.: Juvenile osteochondritis dissecans of the knee: current concepts in diagnosis and management. Instr Course Lect 2013; 62: pp. 455-467.
11. Abouassaly M., Peterson D., Salci L., et. al.: Surgical management of osteochondritis dissecans of the knee in the paediatric population: a systematic review addressing surgical techniques. Knee Surg Sports Traumatol Arthrosc 2013; 22: pp. 1216-1224.
12. Erickson B.J., Chalmers P.N., Yanke A.B., et. al.: Surgical management of osteochondritis dissecans of the knee. Curr Rev Musculoskelet Med 2013; 6: pp. 102-114.
13. Trinh T.Q., Harris J.D., Flanigan D.C.: Surgical management of juvenile osteochondritis dissecans of the knee. Knee Surg Sports Traumatol Arthrosc 2012; 20: pp. 2419-2429.
14. Vannini F., Battaglia M., Buda R., et. al.: “One step” treatment of juvenile osteochondritis dissecans in the knee: clinical results and T2 mapping characterization. Orthop Clin North Am 2012; 43: pp. 237-244. vi
15. Kijowski R., Blankenbaker D.G., Shinki K., et. al.: Juvenile versus adult osteochondritis dissecans of the knee: appropriate MR imaging criteria for instability. Radiology 2008; 248: pp. 571-578.
16. Heywood C.S., Benke M.T., Brindle K., et. al.: Correlation of magnetic resonance imaging to arthroscopic findings of stability in juvenile osteochondritis dissecans. Arthroscopy 2010; 27: pp. 194-199.
17. Jacobs J.C., Archibald-Seiffer N., Grimm N.L., et. al.: A review of arthroscopic classification systems for osteochondritis dissecans of the knee. Clin Sports Med 2014; 33: pp. 189-197.
18. Brittberg M., Winalski C.S.: Evaluation of cartilage injuries and repair. J Bone Joint Surg Am 2003; 85-A: pp. 58-69.
19. Dipaola J.D., Nelson D.W., Colville M.R.: Characterizing osteochondral lesions by magnetic resonance imaging. Arthroscopy 1991; 7: pp. 101-104.
20. Chen C.H., Liu Y.S., Chou P.H., et. al.: MR grading system of osteochondritis dissecans lesions: comparison with arthroscopy. Eur J Radiol 2013; 82: pp. 518-525.
21. De Smet A.A., Ilahi O.A., Graf B.K.: Reassessment of the MR criteria for stability of osteochondritis dissecans in the knee and ankle. Skeletal Radiol 1996; 25: pp. 159-163.
22. Zbojniewicz A.M., Laor T.: Imaging of osteochondritis dissecans. Clin Sports Med 2014; 33: pp. 221-250.
23. De Smet A.A., Fisher D.R., Graf B.K., et. al.: Osteochondritis dissecans of the knee: value of MR imaging in determining lesion stability and the presence of articular cartilage defects. AJR Am J Roentgenol 1990; 155: pp. 549-553.
24. Mesgarzadeh M., Sapega A.A., Bonakdarpour A., et. al.: Osteochondritis dissecans: analysis of mechanical stability with radiography, scintigraphy, and MR imaging. Radiology 1987; 165: pp. 775-780.
25. Nelson D.W., DiPaola J., Colville M., et. al.: Osteochondritis dissecans of the talus and knee: prospective comparison of MR and arthroscopic classifications. J Comput Assist Tomogr 1990; 14: pp. 804-808.
26. Samora W.P., Chevillet J., Adler B., et. al.: Juvenile osteochondritis dissecans of the knee: predictors of lesion stability. J Pediatr Orthop 2012; 32: pp. 1-4.
27. Kramer J., Stiglbauer R., Engel A., et. al.: MR contrast arthrography (MRA) in osteochondrosis dissecans. J Comput Assist Tomogr 1992; 16: pp. 254-260.
28. Toth F., Nissi M.J., Wang L., et. al.: Surgical induction, histological evaluation, and MRI identification of cartilage necrosis in the distal femur in goats to model early lesions of osteochondrosis. Osteoarthritis Cartilage 2015; 23: pp. 300-307.
29. Gold G.E., Chen C.A., Koo S., et. al.: Recent advances in MRI of articular cartilage. AJR Am J Roentgenol 2009; 193: pp. 628-638.
30. Ellermann J., Ling W., Nissi M.J., et. al.: MRI rotating frame relaxation measurements for articular cartilage assessment. Magn Reson Imaging 2013; 31: pp. 1537-1543.
31. Laor T., Zbojniewicz A.M., Eismann E.A., et. al.: Juvenile osteochondritis dissecans: is it a growth disturbance of the secondary physis of the epiphysis?. AJR Am J Roentgenol 2012; 199: pp. 1121-1128.