Rationale and Objectives
To increase radiologic knowledge, the distribution of mammographic features on prior screening mammograms of missed interval and screen-detected cancers was compared to the distribution on diagnostic mammograms of screen-detected cancers. The same variables were compared on mammograms of discordant and concordant screen-detected cancers.
Materials and Methods
The study was performed in Møre og Romsdal County, Norway, as a part of the quality assurance of the Norwegian Breast Cancer Screening Program. Women were screened using analog techniques and diagnosed from 2002 to 2008. Prior and diagnostic mammograms of 81 interval and 123 screen-detected breast cancers in women aged 50 to 71 years were retrospectively reviewed and classified as either missed or true by four experienced breast radiologists. Mammographic features were classified according to a modified Breast Imaging Reporting and Data System.
Results
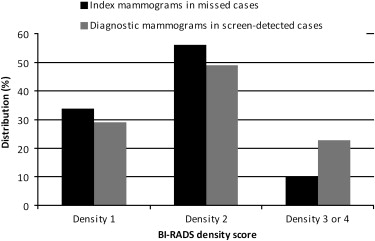
Thirty percent (24 of 81) of the interval cancers and 21% (26 of 123) of the screen-detected cancers were classified as missed. Calcifications, alone or in association with mass or asymmetry, tended to be more common on prior mammograms of missed cancers compared to diagnostic mammograms of screen-detected cancers (34% [17 of 50] vs 21% [26 of 123], P = .114), whereas an opposite trend was seen for mass (54% [27 of 50] vs 68% [84 of 123], P = .109). Similar results were seen when comparing discordant and concordant cancers.
Conclusions
Calcifications represent a challenge in the interpretation of screening mammograms. For educational purposes, the importance of reviewing both interval and screen-detected cancers is obvious. Knowledge gained from systematic reviews might reduce the number of missed cancers on mammographic screening. Performing reviews according to established guidelines would make it possible to compare results across screening programs.
The term “interval cancer” refers to a breast cancer diagnosed in the interval between two screening sessions . Several studies have found that a substantial portion of interval cancers can be classified as missed on retrospective review. Thus, the interval cancer rate is considered a quality measure of a screening program. However, defining interval cancers is somewhat controversial , making comparisons of rates across screening programs difficult. The percentages of missed cancers have varied in previous studies because of different procedures for initial interpretation and review designs . In studies performed with prior screening mammograms and diagnostic mammograms available, roughly 20% to 30% of interval cancers showed signs on screening mammograms that, in a retrospective view, should have resulted in recall for diagnostic workup .
Despite the educational potential of reviewing mammograms of interval and screen-detected cancers in subsequently screened women, neither the European guidelines nor American recommendations describe preferable procedures for reviews or accepted levels for missed cancers . Actually, only a few studies have dealt with review of screen-detected cancers, despite the fact that the percentage of missed cancers seems to adhere to what is found in reviews of interval cancers .
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Materials and methods
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Study Population
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Retrospective Review Design
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Discordant Cancers
Get Radiology Tree app to read full this article<
Statistical Analyses
Get Radiology Tree app to read full this article<
Results
Get Radiology Tree app to read full this article<
Table 1
Interval and Screen-detected Breast Cancer Based on a Retrospective Review of Prior and Diagnostic Mammograms in Women Aged 50 to 71 Years
Classification Group Interval Cancer
(n = 81) Screen-detected Cancer ∗
(n = 123) All
(n = 204) Missed 18 (22.2%) 15 (12.2%) 33 (16.2%) Minimal signs actionable 6 (7.4%) 11 (8.9%) 17 (8.3%) Minimal signs not actionable 26 (32.1%) 46 (37.4%) 72 (35.3%) True 31 (38.3%) 51 (41.5%) 82 (40.2%)
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Table 2
Mammographic Features on Prior Mammograms of Missed Interval and Screen-detected Breast Cancer and on Diagnostic Mammograms of Screen-detected Breast Cancer in Women Aged 50 to 71 Years
Index Mammograms Diagnostic Mammograms Feature Missed Cancers
(n = 50) Screen-detected Cancers ∗
(n = 123) χ 2 P Value Mass 27 (54.0%) 84 (68.3%) .109 Calcification alone or in association with mass or asymmetry 17 (34.0%) 26 (21.1%) .114 Asymmetry 5 (10.0%) 2 (1.6%) .035 Architectural distortion 1 (2.0%) 8 (6.5%) .406 Occult 0 (0%) 3 (2.4%) .637
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Table 3
Shape, Margins, and Density of Mass ∗ Identified on Prior Mammograms of Missed Cancer and on Diagnostic Mammograms of Screen-detected Cancer in Women Aged 50 to 71 Years
Index Mammograms Diagnostic Mammograms Variable Missed Cancers
(n = 30) Screen-detected Cancers †
(n = 89) χ 2 P Value Shape Oval 2 (6.7%) 3 (3.4%) .801 Round 1 (3.3%) 11 (12.4%) .285 Irregular 26 (86.7%) 72 (80.9%) .660 Lobular 1 (3.3%) 3 (3.4%) 1 Margins Circumscribed 1 (3.3%) 1 (1.1%) 1 Indistinct 15 (50.0%) 31 (34.8%) .208 Spiculated 14 (46.7%) 57 (64.0%) .144 Density High 0 (0%) 5 (5.6%) .424 Isodense 30 (100%) 84 (94.4%) .424
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Table 4
Mammographic Features on Diagnostic Mammograms of Discordant and Concordant Screen-detected Breast Cancer ∗ in Women Aged 50 to 71 Years
Feature Discordant Cancer
(n = 30) Concordant Cancer
(n = 93) χ 2 P Value Mass 16 (53.3%) 68 (73.1%) .072 Calcification alone or in association with mass or asymmetry 9 (30.0%) 17 (18.3%) .267 Architectural distortion 4 (13.3%) 4 (4.3%) .187 Asymmetry 1 (3.3%) 1 (1.1%) .984 Occult 0 (0%) 3 (3.2%) .753
Get Radiology Tree app to read full this article<
Table 5
Shape, Margins, and Density of Mass ∗ Identified on Diagnostic Mammograms of Discordant and Concordant Screen-detected Breast Cancer † in Women Aged 50 to 71 Years
Variable Discordant Cancer
(n = 17) Concordant Cancer
(n = 72) χ 2 P Value Shape Oval 0 (0%) 3 (4.2%) .913 Round 3 (17.6%) 8 (11.1%) .744 Irregular 14 (82.4%) 58 (80.6%) 1 Lobular 0 (0%) 3 (4.2%) .913 Margins Circumscribed 0 (0%) 1 (1.4%) 1 Indistinct 9 (52.9%) 22 (30.6%) .144 Spiculated 8 (47.1%) 49 (68.1%) .180 Density High 0 (0%) 5 (6.9%) .594 Isodense 17 (100%) 67 (93.1%) .594
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Discussion
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Conclusions
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
References
1. Perry N., Broeders M.J., de Wolf C., et. al.: European guidelines for quality assurance in breast cancer screening and diagnosis.4th ed.2006.Office for Official Publications of the European CommunitiesLuxembourg
2. Bulliard J.L., Sasieni P., Klabunde C., et. al.: Methodological issues in international comparison of interval breast cancers. Int J Cancer 2006; 119: pp. 1158-1163.
3. Hofvind S., Geller B., Vacek P.M., et. al.: Using the European guidelines to evaluate the Norwegian Breast Cancer Screening Program. Eur J Epidemiol 2007; 22: pp. 447-455.
4. Tornberg S., Kemetli L., Ascunce N., et. al.: A pooled analysis of interval cancer rates in six European countries. Eur J Cancer Prev 2010; 19: pp. 87-93.
5. Moberg K., Grundstrom H., Tornberg S., et. al.: Two models for radiological reviewing of interval cancers. J Med Screen 1999; 6: pp. 35-39.
6. Hofvind S., Skaane P., Vitak B., et. al.: Influence of review design on percentages of missed interval breast cancers: retrospective study of interval cancers in a population-based screening program. Radiology 2005; 237: pp. 437-443.
7. Ciatto S., Catarzi S., Lamberini M.P., et. al.: Interval breast cancers in screening: the effect of mammography review method on classification. Breast 2007; 16: pp. 646-652.
8. D’Orsi C.J., Bassett L., Berg W.: Breast Imaging Reporting and Data System, BI-RADS: Mammography.4th ed.2003.American College of RadiologyReston, VA
9. Rosenberg R.D., Yankaskas B.C., Abraham L.A., et. al.: Performance benchmarks for screening mammography. Radiology 2006; 241: pp. 55-66.
10. Moberg K., Grundstrom H., Lundquist H., et. al.: Radiological review of incidence breast cancers. J Med Screen 2000; 7: pp. 177-183.
11. van Dijck J.A., Verbeek A.L., Hendriks J.H., et. al.: The current detectability of breast cancer in a mammographic screening program. A review of the previous mammograms of interval and screen-detected cancers. Cancer 1993; 72: pp. 1933-1938.
12. Harvey J.A., Fajardo L.L., Innis C.A.: Previous mammograms in patients with impalpable breast carcinoma: retrospective vs blinded interpretation. 1993 ARRS President’s Award. AJR Am J Roentgenol 1993; 161: pp. 1167-1172.
13. Duncan K.A., Needham G., Gilbert F.J., et. al.: Incident round cancers: what lessons can we learn?. Clin Radiol 1998; 53: pp. 29-32.
14. Hofvind S., Geller B.M., Rosenberg R.D., et. al.: Screening-detected breast cancers: discordant independent double reading in a population-based screening program. Radiology 2009; 253: pp. 652-660.
15. Tabàr L., Dean P.B.: Teaching atlas of mammography.1983.Thieme VerlagStuttgart, Germany
16. Kopans D.B.: Breast imaging.3rd ed.2007.Lippincott Williams & WilkinsPhiladelphia, PA
17. Tabar L., Tot T., Dean P.: Breast cancer: early detection with mammography. Perception, interpretation, histopathologic correlation.2007.Thieme VerlagStuttgart, Germany
18. Fischer U., Baum F., Luftner-Nagel S.: Direct diagnosis in radiology. Breast imaging.2008.Thieme VerlagStuttgart, Germany
19. Skaane P.: Studies comparing screen-film mammography and full-field digital mammography in breast cancer screening: updated review. Acta Radiol 2009; 50: pp. 3-14.
20. Karssemeijer N., Bluekens A.M., Beijerinck D., et. al.: Breast cancer screening results 5 years after introduction of digital mammography in a population-based screening program. Radiology 2009; 253: pp. 353-358.
21. Vinnicombe S., Pinto Pereira S.M., McCormack V.A., et. al.: Full-field digital versus screen-film mammography: comparison within the UK breast screening program and systematic review of published data. Radiology 2009; 251: pp. 347-358.
22. Freer T.W., Ulissey M.J.: Screening mammography with computer-aided detection: Prospective study of 12,860 patients in a community breast center. Radiology 2001; 220: pp. 781-786.
23. Cupples T.E., Cunningham J.E., Reynolds J.C.: Impact of computer-aided detection in a regional screening mammography program. AJR Am J Roentgenol 2005; 185: pp. 944-950.
24. Dean J.C., Ilvento C.C.: Improved cancer detection using computer-aided detection with diagnostic and screening mammography: prospective study of 104 cancers. AJR Am J Roentgenol 2006; 187: pp. 20-28.
25. Morton M.J., Whaley D.H., Brandt K.R., et. al.: Screening mammograms: Interpretation with computer-aided detection—prospective evaluation. Radiology 2006; 239: pp. 375-383.
26. Destounis S.V., DiNitto P., Logan-Young W., et. al.: Can computer-aided detection with double reading of screening mammograms help decrease the false-negative rate? Initial experience. Radiology 2004; 232: pp. 578-584.
27. Skaane P., Kshirsagar A., Stapleton S., et. al.: Effect of computer-aided detection on independent double reading of paired screen-film and full-field digital screening mammograms. AJR Am J Roentgenol 2007; 188: pp. 377-384.
28. Gromet M.: Comparison of computer-aided detection to double reading of screening mammograms: review of 231,221 mammograms. AJR Am J Roentgenol 2008; 190: pp. 854-859.