Rationale and Objectives
Stereology is a simple, fast method for object segmentation that involves counting the number of intersections of a randomly positioned grid over an object. The objectives of this study were to determine observer reliability in making stereologic- and ellipsoid-based measurements of uterine and leiomyoma volumes and to test the agreement between these two methods of measurement.
Materials and Methods
Two observers made uterine and dominant leiomyoma volume measurements on MR images in 30 patients using stereology and the popular ellipsoid-based technique. Stereologic volume measurements were made from high-resolution T2 images in two perpendicular planes (axial and sagittal). Ellipsoid volume was calculated by multiplying the maximal sagittal, anteroposterior, and transverse dimensions by π/6. For these measurements, interobserver reliability was tested with paired t -tests and percent differences were determined. A mean stereologic volume and a mean ellipsoid volume were determined and tested for agreement with a paired t -test. Percent differences were also calculated.
Results
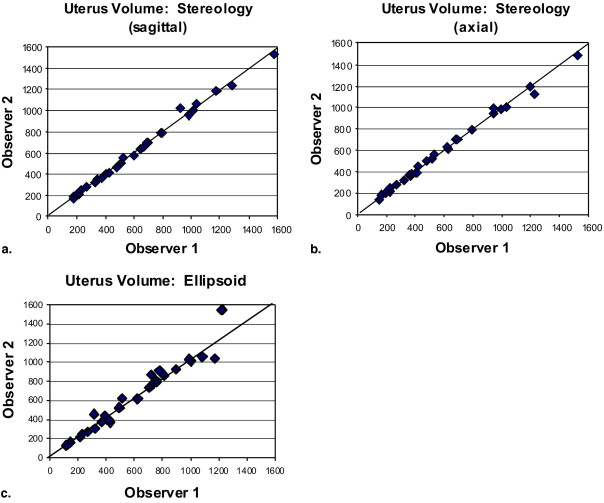
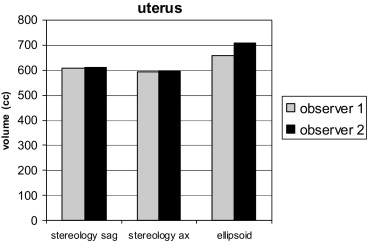
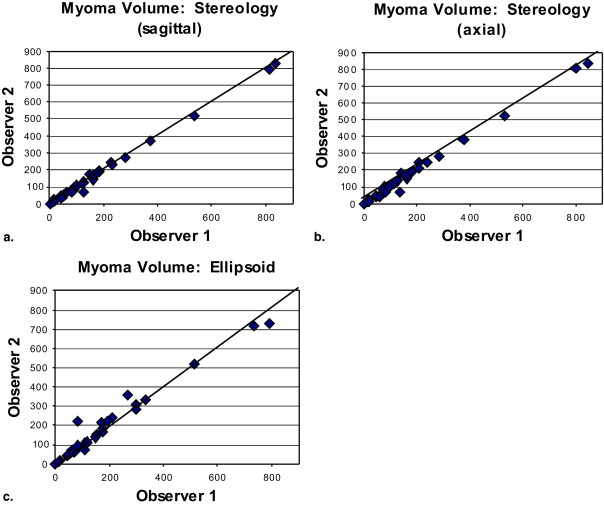
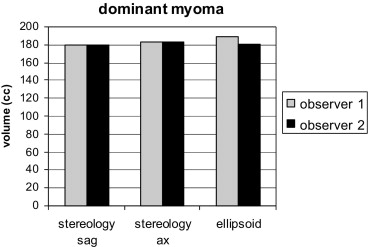
Stereologic measurements demonstrated excellent interobserver reliability with 0.3% difference in mean uterine volumes ( P = .69) and 0.3% difference ( P = .81) in mean leiomyoma volumes. The ellipsoid method resulted in poorer interobserver reliability with 7% difference ( P = .01) in mean uterine volumes and 4% difference ( p = .24) in mean leiomyoma volumes. The ellipsoid method also significantly overestimated uterine volumes by 14% ( P < .01) compared with stereology.
Conclusion
Stereology provided high interobserver reliability for leiomyoma and overall uterine volume measurements and was more reliable than the ellipsoid method, which uses linear measurements. Stereology appears well suited when precise volume measurements are desired for assessing response to uterine arterial embolization treatments.
Measurements of uterine and dominant leiomyoma volumes are an integral part of the treatment evaluation of uterine artery embolization and other techniques for treating symptomatic leiomyomata. Given the increasing popularity of uterine arterial embolization treatment and the more recent addition of magnetic resonance-guided focused ultrasound as a treatment option ( ), a reliable method for volume measurement is desirable. Uterine and leiomyoma sizes are commonly assessed with the ellipsoid-based volume measurement method, i.e., the volume is estimated from linear measurements in three perpendicular directions using the equation for an ellipsoid. The reliability of this method, however, has previously been addressed in only one study, which focused on patients undergoing hormonal treatment of symptomatic leiomyomata ( ).
While direct volume measurement techniques are more time consuming than volume estimations from linear measurements, they have been shown to be more reliable ( ). One such technique is stereology (also known as point counting), a simple, fast method for object segmentation that involves counting the number of intersections of a randomly positioned grid over an object. This method has the advantage of not relying on border tracing or threshold determination. Instead, it relies on the operator’s visual perception to select all points that lie within the object of interest. Stereology, which has gained popularity in cytopathology and medical imaging analysis, has been previously shown to be a reliable and accurate method for measuring cyst and renal volumes at MRI in patients with polycystic kidney disease ( ) and in neuroimaging applications ( ). Moreover, stereology (point counting) has been shown to be faster than manual planimetry (border tracing) for measuring liver volumes at MRI ( ). Our hypothesis was that stereologic volume measurements would provide more reliable volume measurements than the commonly used ellipsoid method that estimates volumes from linear measurements. We could not address accuracy in this study because the patients did not undergo hysterectomy that would be required for a true volume determination. Thus, the objectives of this study were to determine observer reliability in making stereologic- and ellipsoid-based measurements of uterine and leiomyoma volumes and to test the agreement between these two methods of measurement.
Materials and methods
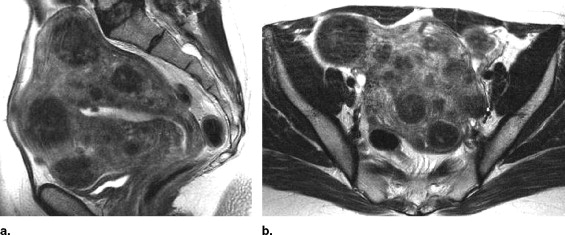
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
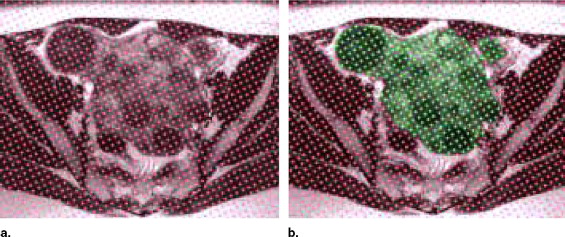
Volume Measurement With Stereology
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
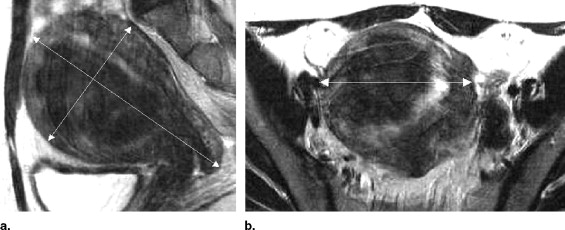
Ellipsoid Measurements
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Statistical Analysis
Get Radiology Tree app to read full this article<
Results
Uterine Volume Measurement
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
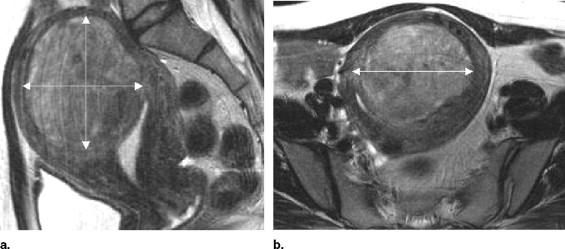
Dominant Leiomyoma Volume Measurement
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Discussion
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
References
1. Smart O.C., Hindley J.T., Regan L., Gedroyc W.M.: Magnetic resonance guided focused ultrasound surgery of uterine fibroids—The tissue effects of GnRH agonist pre-treatment. Eur J Radiol 2006; 59: pp. 163-167.
2. Siskin G.P., Shlansky-Goldberg R.D., Goodwin S.C., et. al.: A prospective multicenter comparative study between myomectomy and uterine artery embolization with polyvinyl alcohol microspheres: Long-term clinical outcomes in patients with symptomatic uterine fibroids. J Vasc Interv Radiol 2006; 17: pp. 1287-1295.
3. McDannold N., Tempany C.M., Fennessy F.M., et. al.: Uterine leiomyomas: MR imaging-based thermometry and thermal dosimetry during focused ultrasound thermal ablation. Radiology 2006; 240: pp. 263-272.
4. Pron G., Bennett J., Common A., Wall J., Asch M., Sniderman K.: The Ontario Uterine Fibroid Embolization Trial. Fertil Steril 2003; 79: pp. 120-127.
5. deSouza N.M., Williams A.D.: Uterine arterial embolization for leiomyomas: Perfusion and volume changes at MR imaging and relation to clinical outcome. Radiology 2002; 222: pp. 367-374.
6. Broekmans F.J., Heitbrink M.A., Hompes P.G., Schoute E., Falke T., Schoemaker J.: Quantitative MRI of uterine leiomyomas during triptorelin treatment: Reproducibility of volume assessment and predictability of treatment response. Magn Reson Imaging 1996; 14: pp. 1127-1135.
7. Joe B.N., Fukui M.B., Meltzer C.C., et. al.: Brain tumor volume measurement: Comparison of manual and semiautomated methods. Radiology 1999; 212: pp. 811-816.
8. Julin P., Melin T., Andersen C., Isberg B., Svensson L., Wahlund L.O.: Reliability of interactive three-dimensional brain volumetry using MP-RAGE magnetic resonance imaging. Psychiatry Res 1997; 76: pp. 41-49.
9. Chapman A.B., Guay-Woodford L.M., Grantham J.J., et. al.: Renal structure in early autosomal-dominant polycystic kidney disease (ADPKD): The Consortium for Radiologic Imaging Studies of Polycystic Kidney Disease (CRISP) cohort. Kidney Int 2003; 64: pp. 1035-1045.
10. Bae K.T., Commean P.K., Lee J.: Volumetric measurement of renal cysts and parenchyma using MRI: Phantoms and patients with polycystic kidney disease. J Comput Assist Tomogr 2000; 24: pp. 614-619.
11. Ronan L., Doherty C.P., Delanty N., Thornton J., Fitzsimons M.: Quantitative MRI: A reliable protocol for measurement of cerebral gyrification using stereology. Magn Reson Imaging 2006; 24: pp. 265-272.
12. Doherty C.P., Fitzsimons M., Holohan T., et. al.: Accuracy and validity of stereology as a quantitative method for assessment of human temporal lobe volumes acquired by magnetic resonance imaging. Magn Reson Imaging 2000; 18: pp. 1017-1025.
13. Mazonakis M., Damilakis J., Maris T., Prassopoulos P., Gourtsoyiannis N.: Comparison of two volumetric techniques for estimating liver volume using magnetic resonance imaging. J Magn Reson Imaging 2002; 15: pp. 557-563.
14. Portney L., Watkins M.: 2003.Appleton and LangeNorwalk, CT
15. Brunereau L., Herbreteau D., Gallas S., et. al.: Uterine artery embolization in the primary treatment of uterine leiomyomas: Technical features and prospective follow-up with clinical and sonographic examinations in 58 patients. AJR Am J Roentgenol 2000; 175: pp. 1267-1272.
16. McLucas B., Adler L., Perrella R.: Uterine fibroid embolization: Nonsurgical treatment for symptomatic fibroids. J Am Coll Surg 2001; 192: pp. 95-105.
17. Bradley E.A., Reidy J.F., Forman R.G., Jarosz J., Braude P.R.: Transcatheter uterine artery embolisation to treat large uterine fibroids. Br J Obstet Gynaecol 1998; 105: pp. 235-240.
18. Katsumori T., Nakajima K., Tokuhiro M.: Gadolinium-enhanced MR imaging in the evaluation of uterine fibroids treated with uterine artery embolization. AJR Am J Roentgenol 2001; 177: pp. 303-307.
19. Jha R.C., Ascher S.M., Imaoka I., Spies J.B.: Symptomatic fibroleiomyomata: MR imaging of the uterus before and after uterine arterial embolization. Radiology 2000; 217: pp. 228-235.
20. Roth A.R., Spies J.B., Walsh S.M., Wood B.J., Gomez-Jorge J., Levy E.B.: Pain after uterine artery embolization for leiomyomata: Can its severity be predicted and does severity predict outcome?. J Vasc Interv Radiol 2000; 11: pp. 1047-1052.
21. Burn P.R., McCall J.M., Chinn R.J., Vashisht A., Smith J.R., Healy J.C.: Uterine fibroleiomyoma: MR imaging appearances before and after embolization of uterine arteries. Radiology 2000; 214: pp. 729-734.
22. Siskin G.P., Stainken B.F., Dowling K., Meo P., Ahn J., Dolen E.G.: Outpatient uterine artery embolization for symptomatic uterine fibroids: Experience in 49 patients. J Vasc Interv Radiol 2000; 11: pp. 305-311.
23. Cotter D., Miszkiel K., Al-Sarraj S., et. al.: The assessment of postmortem brain volume: A comparison of stereological and planimetric methodologies. Neuroradiology 1999; 41: pp. 493-496.