Rationale and Objectives
The aim of this study was to evaluate the magnetic resonance imaging (MRI) interpretation proficiency of musculoskeletal fellows in training.
Materials and Methods
Between July 2003 and June 2007, 14 musculoskeletal fellows were independently tested with 20 MRI studies of the knee and shoulder at four separate time points during their fellowship years. Trends in true-positive and false-positive interpretation results were evaluated. Fellows who completed their residencies at the fellowship institution (internal fellows) were compared with those from other residencies (external fellows).
Results
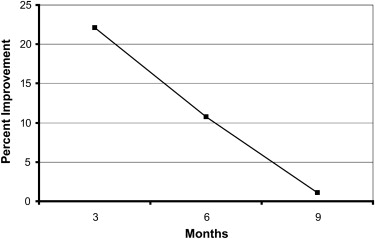
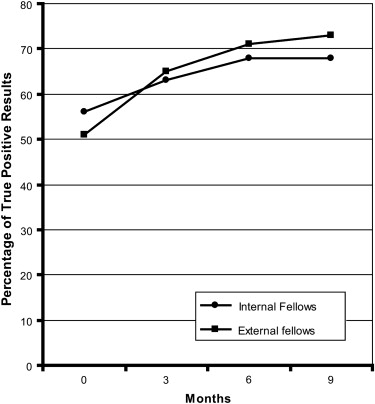
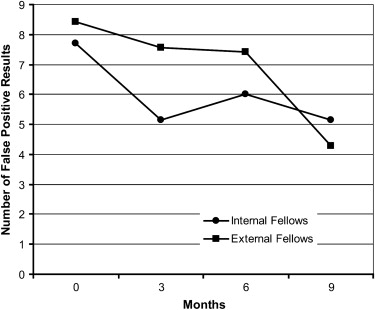
There was a significant improvement in proficiency between the initial and final (9-month) evaluations ( P < .0001). At the initial evaluation, there was a mean of 52.8% (41.7 of 79) true-positive results (range, 32–51); at 9 months, there was a mean of 71.0% (56.1 of 79; range, 40–72). The number of false-positive results also declined during this time period from a mean of 8.1 (range, 2–13) at initial evaluation to 4.7 (range, 2–8) at 9 months ( P < .001). External fellows had more incorrect diagnoses initially but showed greater improvement than internal fellows at 9 months.
Conclusion
Fellows continued to improve their MRI interpretation skills throughout the first 9 months of their fellowships. External fellows were slightly less proficient at the start of their fellowships but slightly more proficient at 9 months compared to internal fellows.
Although the aims of fellowship training are primarily to provide experience and to increase knowledge in a specialized area beyond that achieved during residency , the structure of fellowship training can vary widely. There is a variety of opinions and practices regarding the length of such training, the degree of supervision, the continuity of training, and the choice of staying at the residency institute or going to an outside institution for a fellowship. Although there are many ways to assess the effectiveness of fellowship training and fellows’ competence, image interpretation accuracy is one important method.
In this study, we evaluated the magnetic resonance imaging (MRI) interpretation proficiency of musculoskeletal fellows in training. We sought to determine how fellows’ MRI interpretation skills changed throughout the course of their fellowships. We also wanted to compare the progress of internal fellows (those remaining at the same institution after residency) working in a familiar environment to that of external fellows (those who completed their residency training at different institutions from their fellowships).
Materials and methods
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Results
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Discussion
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Acknowledgments
Get Radiology Tree app to read full this article<
References
1. Berquist T.H.: Postgraduate musculoskeletal fellowship training in the United States: current trends and future direction. Skeletal Radiol 2003; 32: pp. 337-342.
2. Glauser S.J., Maynard C.D.: Residency and fellowship training in radiology: survey of all United States programs. Acad Radiol 1994; 1: pp. 159-163.
3. Prasad R.S.: Jack of all trades, master of none: why do a fellowship?. J Am Coll Radiol 2004; 1: pp. 607-608.
4. Wood J., Collins J., Burnside E.S., et. al.: Patient, faculty, and self-assessment of radiology resident performance: a 360-degree method of measuring professionalism and interpersonal/communication skills. Acad Radiol 2004; 11: pp. 931-939.
5. Jamadar D.A., Carlos R., Caoili E.M., et. al.: Estimating the effects of informal radiology resident teaching on radiologist productivity—what is the cost of teaching?. Acad Radiol 2005; 12: pp. 123-128.
6. Joiner K.A., Dismukes W.E., Britigan B.E., et. al.: Adequacy of fellowship training: results of a survey of recently graduated fellows. Clin Infect Dis 2001; 32: pp. 255-262.
7. Kempainen R.R., Hallstrand T.S., Culver B.H., Tonelli M.R.: Fellows as teachers: the teacher-assistant experience during pulmonary subspecialty training. Chest 2005; 128: pp. 401-406.
8. Flemming D., Davis K.W., Dinauer P.A., et. al.: Musculoskeletal radiology curriculum for radiology residents. J Am Coll Radiol 2007; 4: pp. 636-639.
9. Wald C., Luchs J., Davila J., et. al.: Residents’ perception of MRI training in the United States. J Am Coll Radiol 2004; 1: pp. 331-337.
10. De Smet A.A., Tuite M.J.: Use of the “two-slice-touch” rule for the MRI diagnosis of meniscal tears. AJR Am J Roentgenol 2006; 187: pp. 911-914.
11. Urbaniak J.R., Cruft G.E., Biester T.W.: The initial examination for a certificate of added qualifications in surgery of the hand. J Bone Joint Surg Am 1990; 72: pp. 639-642.
12. Cruft G.E., Humphreys J.W., Hermann R.E., Meskauskas J.A.: Recertification in surgery, 1980. Ach Surg 1981; 116: pp. 1093-1096.