Rationale and Objectives
At the authors’ level 1 trauma center, postgraduate year 3 and 4 radiology residents interpret urgent overnight imaging studies, which are reviewed by attending radiologists the next morning. The goals of this study were to determine the discrepancy rate for torso computed tomography between resident radiologists’ preliminary interpretations and attending radiologists’ final interpretations and to identify adverse patient events secondary to the delayed diagnoses.
Materials and Methods
All torso computed tomographic studies interpreted by weekday night residents (8 pm to 8 am ) from January 1, 2005, to March 13, 2007, were evaluated retrospectively. Major discrepancies between the residents’ interpretations and the attending radiologists’ interpretations were compiled. Exams with major discrepancies were additionally reviewed by two radiology residents and an attending emergency radiologist. The medical records of patients with major discrepant findings were also reviewed to identify adverse events that occurred because of the delays in final interpretation.
Results
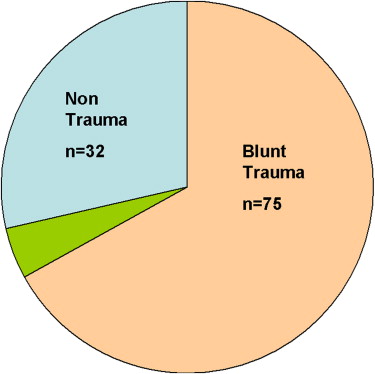
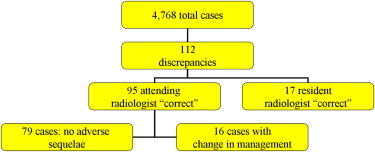
A total of 4768 chest, abdominal, and/or pelvic computed tomographic studies were interpreted during the study period. A total of 112 major discrepancies were collected. In 17 cases (15%), two additional radiology residents and an attending emergency radiologist agreed with the initial residents’ interpretations, decreasing the major discrepancy rate to 95 of 4768 (2.0%), consistent with data from the literature (0.4%–10%). Management was changed in 16 patients (0.3%) because of the major discrepancies: 13 patients underwent additional investigations, and 3 patients were recalled to the emergency room. No mortality or morbidity was directly attributed to the delays in diagnosis.
Conclusion
At the authors’ institution, there was a 2.0% discrepancy rate between residents’ preliminary interpretations and attending radiologists’ final interpretations of overnight torso computed tomography, with a small rate of additional intervention as a result of the major discrepancies. No adverse patient effects were directly attributable to discrepant interpretations. In discrepant cases, there was a 15% disagreement rate (17 of 112) between attending radiologists, suggesting some degree of interreader variance in interpretation. In addition, this disagreement rate among attending radiologists may imply that these cases were complex. Because there is educational value in overnight call, independent radiology resident coverage should continue.
At our level 1 trauma center, overnight in-house radiology coverage is provided by radiology residents. There are a number of advantages to this. Allowing residents to interpret studies independently tests their knowledge, problem solving, and case management, preparing them for future practice. Also, not having an in-house attending radiologist overnight helps with staffing constraints and cost savings. To ensure that radiology residents’ performance is adequate, our institution records data for all discrepancies in interpretation between radiology residents and attending radiologists.
Our hypothesis was that there is a small but acceptable overnight resident error rate. When these errors occur, they typically do not have adverse effects on patient outcomes. The aims of this study were to determine the discrepancy rate between residents and attending radiologists for overnight emergency radiology computed tomographic (CT) interpretation and to determine the clinical impact of these discrepancies.
Materials and methods
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Table 1
Classification of the Study Types of the 112 Discrepant Cases in Torso CT
Classification Included Protocols Number of Cases CT abdomen and pelvis CT abdomen with contrast; CT abdomen aortic protocol; CT abdomen mesenteric protocol 59 CT chest, abdomen, and pelvis CTA chest (aortic protocol); CT chest with/without contrast; CT chest, abdomen, pelvis aortic protocol; CT abdomen and pelvis with contrast 35 CT chest CT chest with/without contrast; CT chest aortic protocol; CT chest pulmonary embolism protocol 16 CT KUB CT abdomen and pelvis without contrast; CT KUB 2
CT, computed tomography; CTA, computed tomographic angiography; KUB, kidneys, ureter, and bladder.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Results
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Table 2
Types of Discrepant Cases
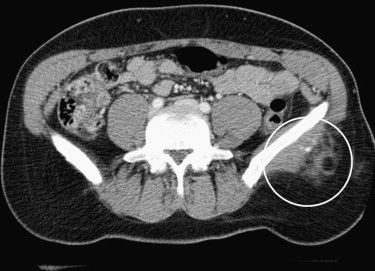
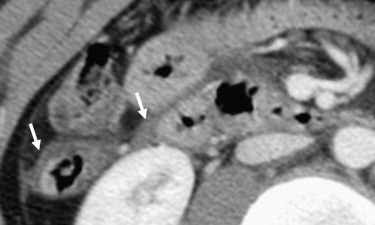
Discrepant Case Number Abdomen and pelvis Liver injury (trauma) 6 Renal injury (trauma) 3 Splenic injury (trauma) 3 Possible gastric, bowel, or mesenteric injury (trauma) 13 Fluid or blood in the abdomen, pelvis, or retroperitoneum 4 Appendicitis 2 Adrenal hematoma or mass 4 Nontraumatic bowel pathology (eg, possible SBO, colitis, inflammation) 9 Nontraumatic renal pathology (eg, cystic renal disease, pyelonephritis, infarct) 5 Nontraumatic pancreatic or biliary pathology (eg, possible mass, pseudocyst) 3 Venous or arterial thrombus 3 Renal or bladder calculi 3 Miscellaneous 6 Total 64 Chest Pulmonary emboli or IVC thrombus 4 Pneumothorax 8 Aortic dissection or pseudoaneurysm 2 Lung nodule or mass 2 Mediastinal hematoma, mass, or adenopathy 4 Lung parenchymal findings (eg, pneumonia, laceration, contusion) 5 Miscellaneous 6 Total 31
IVC, inferior vena cava; SBO, small-bowel obstruction.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Table 3
Results Summary
Result (n = 95) % of Discrepancies (n = 4768) % of Total Number of Studies Total major discrepancies (95 studies) 100% 2% Missed finding (87 studies) 92% 2% Change in recommendation (22 studies) 23% 0.5% Change in differential diagnosis (8 studies) 8% 0.2% Additional intervention performed (16 studies) 17% 0.3% Adverse patient outcome secondary to delay in final interpretation (0 studies) 0% 0%
Get Radiology Tree app to read full this article<
Discussion
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Table 4
Summary of Discrepancy Rates Between Residents and Attending Radiologists When Interpreting Torso Computed Tomography
Study Major Minor Adverse Effects This study 0.3%–2.0% N/A 0% Carney et al 1% 5% 0% Wechsler et al 2.8% 10% No definite Strub et al 0.4% 1.4% 0.1% Stevens et al 0.5% 2.2% 0% Cooper et al 2.5% 7.3% Not obtained Velmahos et al , ∗ 5% 6% No deaths Tieng et al 10% 20% 0%
N/A, not available.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Conclusion
Get Radiology Tree app to read full this article<
References
1. Lal N.R., Murray U.M., Eldevik O.P., Desmond J.S.: Clinical consequences of misinterpretations of neuroradiologic CT scans by on-call radiology residents. AJNR Am J Neuroradiol 2000; 21: pp. 124-129.
2. Strub W.M., Vagal A.A., Tomsick T., Moulton J.S.: Overnight resident preliminary interpretations on CT examinations: should the process continue?. Emerg Radiol 2006; 13: pp. 19-23.
3. Tieng N., Grinberg D., Li S.F.: Discrepancies in interpretation of ED body computed tomographic scans by radiology residents. Am J Emerg Med 2007; 25: pp. 45-48.
4. Velmahos G.C., Fili C., Vassiliu P., Nicolaou N., Radin R., Wilcox A.: Around-the-clock attending radiology coverage is essential to avoid mistakes in the care of trauma patients. Am Surg 2001; 67: pp. 1175-1177.
5. Wechsler R.J., Spettell C.M., Kurtz A.B., et. al.: Effects of training and experience in interpretation of emergency body CT scans. Radiology 1996; 199: pp. 717-720.
6. Wong C., Taubman K., Hoehne F., et. al.: The quality of surgical resident interpretation of after-hour CT scans of the head and abdomen in trauma. Am Surg 2005; 71: pp. 772-775.
7. Wysoki M.G., Nassar C.J., Koenigsberg R.A., Novelline R.A., Faro S.H., Faerber E.N.: Head trauma: CT scan interpretation by radiology residents versus staff radiologists. Radiology 1998; 208: pp. 125-128.
8. Stevens K., Griffiths K., Rosenberg J., Mahadevan S., Zatz L., Leung A.: Discordance rates between preliminary and final radiology reports on cross-sectional imaging studies at a level 1 trauma center. Acad Radiol 2008; 15: pp. 1217-1226.
9. Cooper V., Goodhartz L., Nemcek A.J., Ryu R.: Radiology resident interpretations of on-call imaging studies the incidence of major discrepancies. Acad Radiol 2008; 15: pp. 1198-1204.
10. Carney E., Kempf J., DeCarvalho V., Yudd A., Nosher J.: Preliminary interpretations of after-hours CT and sonography by radiology residents versus final interpretations by body imaging radiologists at a level 1 trauma center. AJR Am J Roentgenol 2003; 181: pp. 367-373.
11. Yoon L.S., Haims A.H., Brink J.A., Rabinovici R., Forman H.P.: Evaluation of an emergency radiology quality assurance program at a level I trauma center: abdominal and pelvic CT studies. Radiology 2002; 224: pp. 42-46.
12. Bechtold R.E., Chen M.Y., Ott D.J., et. al.: Interpretation of abdominal CT: analysis of errors and their causes. J Comput Assist Tomogr 1997; 21: pp. 681-685.
13. Hillman B.J., Swensson R.G., Hessel S.J., Gerson D.E., Herman P.G.: The value of consultation among radiologists. AJR Am J Roentgenol 1976; 127: pp. 807-809.
14. Herman P.G., Gerson D.E., Hessel S.J., et. al.: Disagreements in chest roentgen interpretation. Chest 1975; 68: pp. 278-282.