Rationale and Objectives
Our objective was to evaluate the frequency with which patients viewed their online radiology reports in relation to clinical and laboratory notes and identify sociodemographic factors associated with report viewing.
Method and Materials
We conducted a cross-sectional study of 129,419 patients who had online patient portal access in our large health system in 2014. We determined whether patients viewed their radiology reports, laboratory reports, and clinical notes. We also collected patient sociodemographic information including gender, age, primary spoken language, race/ethnicity, and insurance status. We performed multivariate analyses to determine significant associations between viewing of radiology reports and viewing of other types of clinical reports and patient characteristics.
Results
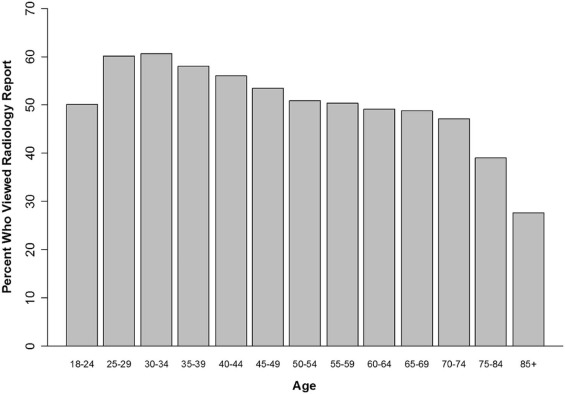
Of 61,131 patients with at least one radiology report available, 31,308 (51.2%) viewed them. Patients who also viewed laboratory reports or clinical notes were significantly more likely to view their radiology reports ( P < 0.001). Women (56.2%), patients 25–39 years old (59.5%), and English speakers (53.6%) were most likely to view radiology reports. In multivariate analysis, Asian-Americans were more likely and African-Americans were less likely to view their radiology reports compared to whites (OR = 1.07 and OR = 0.39, respectively; P < 0.001 for both). Patients with Medicaid were less likely to view radiology reports compared to patients with commercial insurance (OR = 0.38, P < 0.001).
Conclusion
More than half of patients with access to online radiology reports viewed them, with higher viewing rates associated with viewing other types of reports and lower rates associated with characteristics of traditionally underserved patient populations.
Introduction
Patient web portals are online tools that provide patients direct and secure access to their personal medical records. Recent trends leaning toward increased transparency and improved communication between doctors and patients have led to the rapid proliferation of web portals, changing the dynamics of shared health information and decision-making . These changes have been highlighted by federal policies enacted to promote meaningful use of health information technology with the aims of improving productivity and efficiency of healthcare delivery . Although initial doctor and patient adoption of online web portal tools was modest, demand has steadily increased over the past couple of decades . Financial incentives by Medicare and private insurers have aided in successful implementation of online web portals at large, integrated health systems, where use has been established for numerous functions including patient scheduling, test result notification, and doctor-patient communication .
Although long-term outcome data are limited, potential benefits include improvements in medication adherence, patient safety, patient engagement, rates of screening, patient-provider communication, efficiency of office visits, and satisfaction with care . Initial research has been mostly positive, but patient- and doctor-related obstacles have been identified including privacy concerns, increases in clinical report preparation time, and difficulty addressing controversial issues related to candid, written assessments by doctors regarding their patients’ substance abuse, mental health issues, and obesity . Despite these possible challenges, both doctors and patients remain enthusiastic about patients playing a more active role in their healthcare through direct access to their medical record .
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Materials and Methods
Study Setting and Population
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Data Collection
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Statistical Analysis
Get Radiology Tree app to read full this article<
Results
Get Radiology Tree app to read full this article<
Table 1
Sociodemographic Characteristics of Patients with Available Radiology Reports
Characteristic % ( n ) Sex Male 34.7%(21,223) Female 65.3%(39,908) Age in years Mean ± SD 52 ± 17years 18–24 5.8%(3,551) 25–39 19.3%(11,814) 40–64 50.5%(30,875) 65 or older 24.4%(14,891) Race American Indian or Alaska Native 0.8%(522) Asian or Pacific Islander 10.4%(6,376) Black or African American 6.2%(3,817) Hispanic or Latino 3.0%(1,850) White 72.2%(44,163) Other/more than one race 1.1%(675) Unknown 6.1%(3,728) Primary spoken language English 93.0%(56,879) Non-English 6.1%(3,739) Unknown 0.8%(513) Insurance status Commercial 55.6%(33,968) Medicare 27.7%(16,952) Medicaid 13.4%(8,167) Self-pay 2.8%(1,716) Other 0.5%(328)
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Table 2
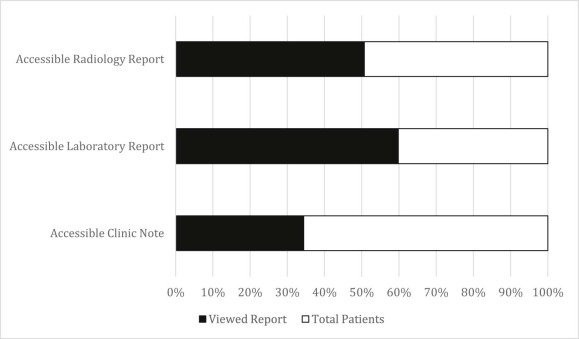
Frequency of Viewing Online Reports by Type
Patient Online Accessible Reports Viewed Radiology Report Viewed Laboratory Report Viewed Clinical Note Radiology report ( n = 61,131) 31,308(51.2%) — — Laboratory report( n = 45,332) 26,219(57.8%) 28,991(64.0%) — Clinical note( n = 1,298) 910(70.1%) — 998(76.9%) Laboratory report( n = 110,260) — 65,966(59.8%) — Clinical note( n = 5,731) — — 1,971(34.4%)
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Table 3
Association Between Viewing Radiology Reports and Other Clinical Reports
Rate of Viewing Radiology Report(s) Multivariate Model for the Probability of Viewing a Radiology Report % (No./Total No.) OR \* (95% CI)P Value Laboratory report(s) No report(s) 32.5% (5,129/15,799) (ref) <0.001 Had report(s) but did not view any 4.4% (722/16,341) 0.12 (0.11–0.13) Had report(s) and viewed at least one 87.8% (25,457/28,991) 14.82 (14.09–15.58) Clinical notes No notes(s) 50.8% (30,398/59,833) (ref) <0.001 Had notes(s) but did not view any 1.3% (4/300) 0.02 (0.01–0.05) Had notes(s) and viewed at least one 90.8% (906/998) 9.25 (7.42–11.52)
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Table 4
Association Between Patient Characteristics with Viewing Radiology Report
Rate of Viewing Radiology Report(s) Multivariate Model for the Probability of Viewing a Radiology Report Variable % (No./Total No.) OR \* (95% CI)P Value Sex Male 41.9%(8,882/21,223) (ref) <0.001 Female 56.2%(22,426/39,908) 1.71(1.65–1.77) Age(52 years ± 17) 18–24 50.1%(1,781/3,551) (ref) <0.001 25–39 59.5%(7,033/11,814) 1.49(1.38–1.62) 40–64 51.6%(15,940/30,875) 1.03(0.96–1.11) 65 or older 44.0%(6,554/14,891) 1.31(1.20–1.44) Race White 54.8%(24,212/44,163) (ref) <0.001 American Indian or Alaska Native 37.2%(194/522) 0.57(0.47–0.68) Asian or Pacific Islander 50.6%(3,224/6,376) 1.07(1.01–1.13) Black or African American 24.8%(948/3,817) 0.39(0.36–0.42) Hispanic or Latino 29.5%(545/1,850) 0.56(0.50–0.63) Other/more than one race 56.1%(379/675) 0.98(0.83–1.15) Unknown 48.4%(1,806/3,728) 0.78(0.72–0.84) Primary spoken language English 53.6%(30,484/56,879) (ref) <0.001 Non-English 16.1%(600/3,739) 0.24(0.22–0.27) Unknown 43.7%(224/513) 0.64(0.54–0.77) Insurance status Commercial 62.4%(21,185/33,968) (ref) <0.001 Medicare 40.2%(6,816/16,952) 0.40(0.38–0.43) Medicaid 33.0%(2,693/8,167) 0.38(0.36–0.41) Self-pay 29.0%(498/1,716) 0.38(0.34–0.42) Other 35.4%(116/328) 0.37(0.29–0.47)
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Discussion
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Funding
Get Radiology Tree app to read full this article<
Acknowledgments
Get Radiology Tree app to read full this article<
References
1. Leveille S.G., Walker J., Ralston J.D., et. al.: Evaluating the impact of patients’ online access to doctors’ visit notes: designing and executing the OpenNotes project. BMC Med Inform Decis Mak 2012; 12: pp. 32.
2. Blumenthal D., Tavenner M.: The “meaningful use” regulation for electronic health records. N Engl J Med 2010; 363: pp. 501-504.
3. Reti S.R., Feldman H.J., Ross S.E., et. al.: Improving personal health records for patient-centered care. J Am Med Inform Assoc 2010; 17: pp. 192-195.
4. Clingan S.A.: Going online: the role of web-based initiatives in health information technology. J Med Pract Manage 2011; 26: pp. 225-227.
5. Centers for Medicare & Medicaid Services (CMS) : Medicare and Medicaid programs; electronic health record incentive program—stage 3 and modifications to meaningful use in 2015 through 2017. Final rules with comment period. Fed Regist 2015; 80: pp. 62761-62955.
6. Baer D.: Patient-physician e-mail communication: the Kaiser Permanente experience. J Oncol Pract 2011; 7: pp. 230-233.
7. Bartlett C., Simpson K., Turner A.N.: Patient access to complex chronic disease records on the Internet. BMC Med Inform Decis Mak 2012; 12: pp. 87.
8. Woods S.S., Schwartz E., Tuepker A., et. al.: Patient experiences with full electronic access to health records and clinical notes through the My HealtheVet Personal Health Record Pilot: qualitative study. J Med Internet Res 2013; 15: pp. e65.
9. Bhavnani V., Fisher B., Winfield M., et. al.: How patients use access to their electronic GP record—a quantitative study. Fam Pract 2011; 28: pp. 188-194.
10. Wade-Vuturo A.E., Mayberry L.S., Osborn C.Y.: Secure messaging and diabetes management: experiences and perspectives of patient portal users. J Am Med Inform Assoc 2013; 20: pp. 519-525.
11. Tierney W.M., Alpert S.A., Byrket A.: Provider responses to patients controlling access to their electronic health records: a prospective cohort study in primary care. J Gen Intern Med 2015; 30: pp. S31-S37.
12. de Lusignan S., Mold F., Sheikh A., et. al.: Patients’ online access to their electronic health records and linked online services: a systematic interpretative review. BMJ Open 2014; 4: pp. e006021.
13. Delbanco T., Walker J., Bell S.K.: Inviting patients to read their doctors’ notes: a quasi-experimental study and a look ahead. Ann Intern Med 2012; 157: pp. 461-470.
14. Zarcadoolas C., Vaughon W.L., Czaja S.J., et. al.: Consumers’ perceptions of patient-accessible electronic medical records. J Med Internet Res 2013; 15: pp. e168.
15. Nazi K.M., Hogan T.P., McInnes D.K., et. al.: Evaluating patient access to Electronic Health Records: results from a survey of veterans. Med Care 2013; 51: pp. S52-S56.
16. Johnson A.J., Easterling D., Williams L.S., et. al.: Insight from patients for radiologists: improving our reporting systems. J Am Coll Radiol 2009; 6: pp. 786-794.
17. Leekha S., Thomas K.G., Chaudhry R., et. al.: Patient preferences for and satisfaction with methods of communicating test results in a primary care practice. Jt Comm J Qual Patient Saf 2009; 35: pp. 497-501.
18. Johnson A.J., Easterling D., Nelson R., et. al.: Access to radiologic reports via a patient portal: clinical simulations to investigate patient preferences. J Am Coll Radiol 2012; 9: pp. 256-263.
19. Lyles C.R., Sarkar U., Ralston J.D., et. al.: Patient-provider communication and trust in relation to use of an online patient portal among diabetes patients: the Diabetes and Aging Study. J Am Med Inform Assoc 2013; 20: pp. 1128-1131.
20. UW Medicine : UW Medicine Overview. Available at: http://www.uwmedicine.org/about/documents/UW-Medicine-Fact-sheet.pdf Accessed February 24, 2016
21. Sarkar U., Karter A.J., Liu J.Y., et. al.: The literacy divide: health literacy and the use of an internet-based patient portal in an integrated health system—results from the diabetes study of northern California (DISTANCE). J Health Commun 2010; 15: pp. 183-196.
22. Sarkar U., Karter A.J., Liu J.Y., et. al.: Social disparities in internet patient portal use in diabetes: evidence that the digital divide extends beyond access. J Am Med Inform Assoc 2011; 18: pp. 318-321.
23. Nazi K.M., Turvey C.L., Klein D.M., et. al.: VA OpenNotes: exploring the experiences of early patient adopters with access to clinical notes. J Am Med Inform Assoc 2015; 22: pp. 380-389. Epub 2014 Oct 28
24. Vodicka E., Mejilla R., Leveille S.G., et. al.: Online access to doctors’ notes: patient concerns about privacy. J Med Internet Res 2013; 15: pp. e208.
25. Mafi J.N., Mejilla R., Feldman H., et. al.: Patients learning to read their doctors’ notes: the importance of reminders. J Am Med Inform Assoc 2016; 0: pp. 1-5.
26. Turvey C., Klein D., Fix G.: Blue Button use by patients to access and share health record information using the Department of Veterans Affairs’ online patient portal. J Am Med Inform Assoc 2014; 21: pp. 657-663.
27. Weingart S.N., Rind D., Tofias Z., et. al.: Who uses the patient internet portal? The PatientSite experience. J Am Med Inform Assoc 2006; 13: pp. 91-95.
28. Cimino J.J., Patel V.L., Kushniruk A.W.: What do patients do with access to their medical records?. Stud Health Technol Inform 2001; 84: pp. 1440-1444.
29. Agarwal R., Anderson C., Zarate J., et. al.: If we offer it, will they accept? Factors affecting patient use intentions of personal health records and secure messaging. J Med Internet Res 2013; 15: pp. e43.
30. Nazi K.M.: The personal health record paradox: health care professionals’ perspectives and the information ecology of personal health record systems in organizational and clinical settings. J Med Internet Res 2013; 15: pp. e70.
31. Hsu J., Huang J., Kinsman J., et. al.: Use of e-Health services between 1999 and 2002: a growing digital divide. J Am Med Inform Assoc 2005; 12: pp. 164-171.
32. Wen K.Y., Kreps G., Zhu F., et. al.: Consumers’ perceptions about and use of the internet for personal health records and health information exchange: analysis of the 2007 Health Information National Trends Survey. J Med Internet Res 2010; 12: pp. e73.
33. Rutten L.J., Squiers L., Hesse B.: Cancer-related information seeking: hints from the 2003 Health Information National Trends Survey (HINTS). J Health Commun 2006; 11: pp. 147-156.
34. Choudhry A., Hong J., Chong K., et. al.: Patients’ preferences for biopsy result notification in an era of electronic messaging methods. JAMA Dermatol 2015; 151: pp. 513-521.
35. Lober W.B., Zierler B., Herbaugh A., et. al.: Barriers to the use of a personal health record by an elderly population. AMIA Annu Symp Proc 2006; pp. 514-518.
36. Ketterer T., West D.W., Sanders V.P., et. al.: Correlates of patient portal enrollment and activation in primary care pediatrics. Acad Pediatr 2013; 13: pp. 264-271.
37. Ralston J.D., Silverberg M.J., Grothaus L., et. al.: Use of Web-based shared medical records among patients with HIV. Am J Manag Care 2013; 19: pp. e114-e124.
38. Miller H., Vandenbosch B., Ivanov D., et. al.: Determinants of personal health record use. J Healthc Inf Manag 2007; 21: pp. 44-48.
39. Roblin D.W., Houston T.K., Allison J.J., et. al.: Disparities in use of a personal health record in a managed care organization. J Am Med Inform Assoc 2009; 16: pp. 683-689.
40. Yamin C.K., Emani S., Williams D.H., et. al.: The digital divide in adoption and use of a personal health record. Arch Intern Med 2011; 171: pp. 568-574.
41. Leveille S.G., Mejilla R., Ngo L., et. al.: Do patients who access clinical information on patient internet portals have more primary care visits?. Med Care 2016; 54: pp. 17-23.