Peripheral non-atherosclerotic arterial disorders (NAADs) are a heterogeneous group of rather uncommon conditions that tend to manifest in subjects without atherosclerosis. Each of these conditions has distinctive pathophysiology; however, there are some common clinical and radiological characteristics and in some cases a common treatment approach that unifies these conditions to a specific group, hence the NAADs. Clinicians and radiologists often fail to recognize NAADs, and there might be a delay in the management of such patients; this may result in seriously adverse outcomes that could otherwise have been avoided or minimized. Knowledge of these conditions and of their radiological appearances is therefore important to help establish a correct diagnosis to allow the prompt initiation of treatment.
The purpose of this pictorial review is to present a selection of NAADs cases and to discuss the radiological characteristics and the most common lines of therapeutic approaches.
Introduction
Peripheral vascular disease (PVD) because of atherosclerosis is more prevalent in men older than 50 years, commonly presenting with intermittent claudication and is associated with morbidity (limb loss) and mortality (increased risk of myocardial infarction and stroke) . In a minority of cases, symptoms of intermittent claudication and mimics of PVD are precipitated by non-atherosclerotic arterial disorders (NAADs). The latter patients are often younger, have little or no risk factors for atherosclerosis, and have delayed diagnosis and sometimes, incorrect treatment. Knowledge of these uncommon conditions and their radiological appearance is essential for early diagnosis and initiation of treatment. NAADs are of a heterogeneous group and range from congenital anatomical variations external to the affected vessel to pathologic changes within the vessel wall .
Congenital Anatomical Variation
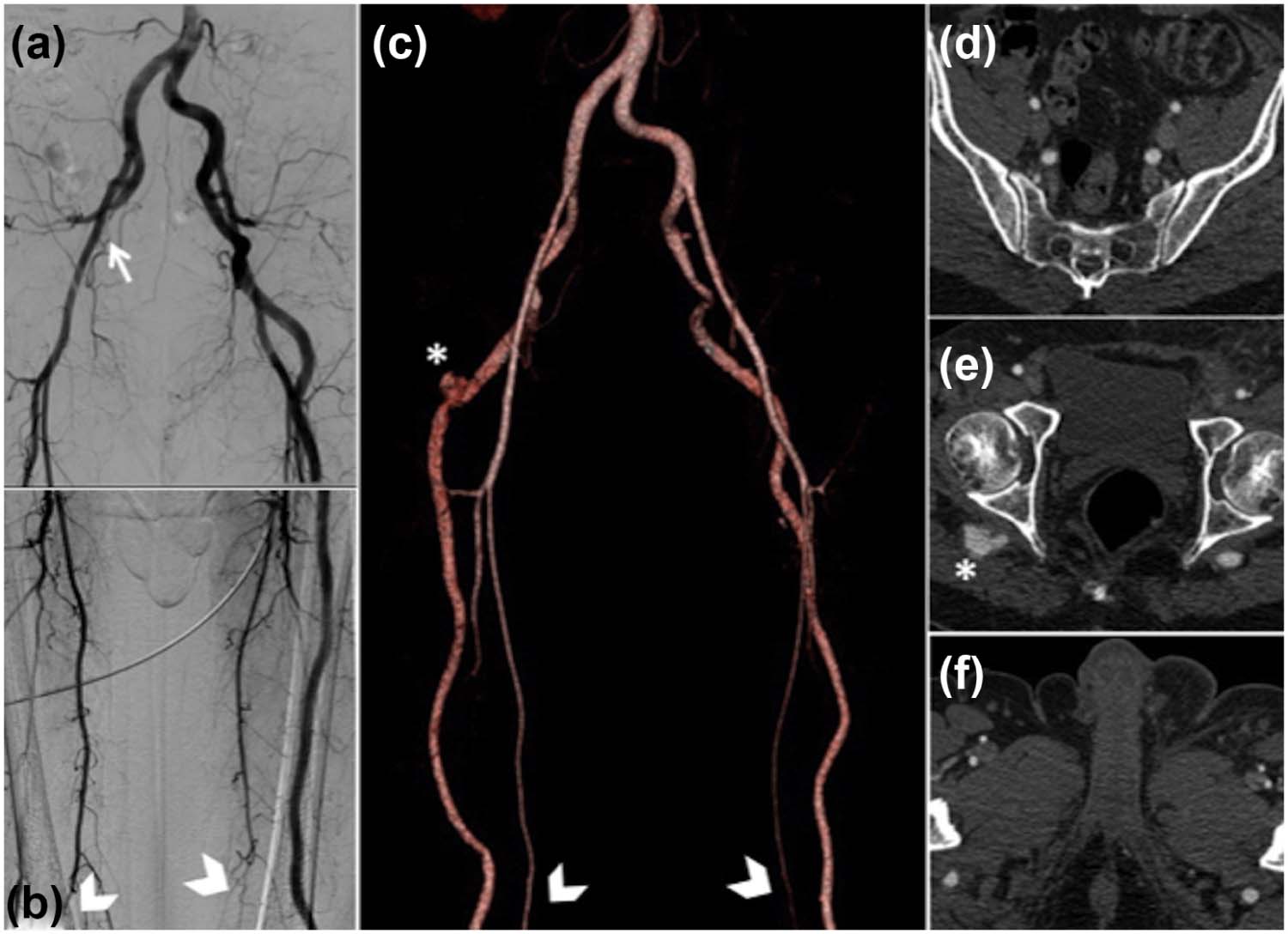
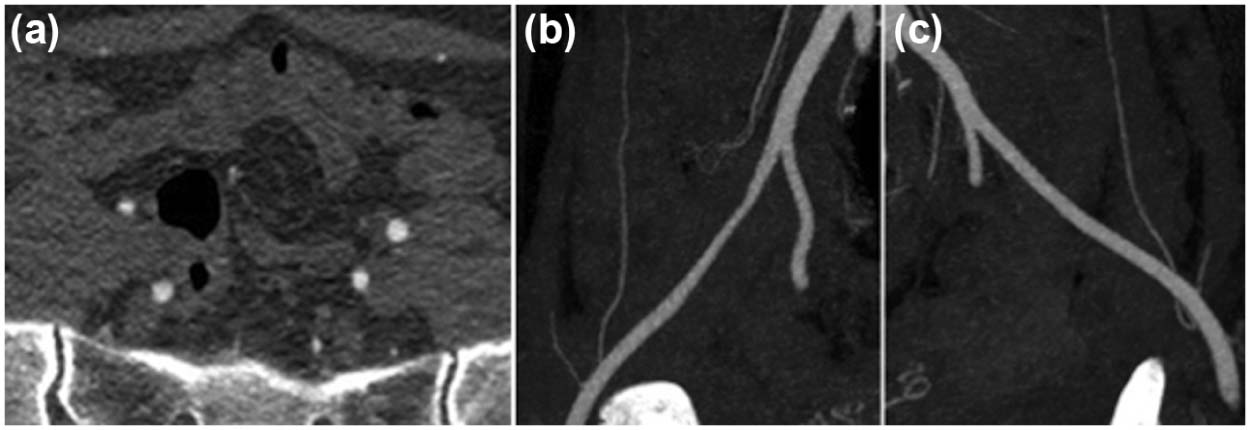
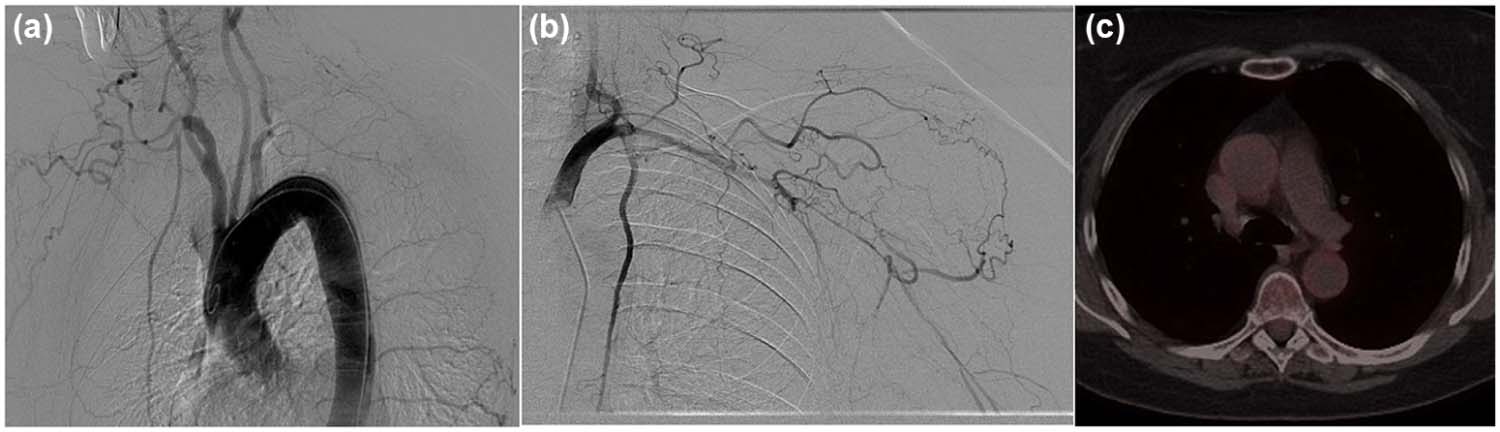
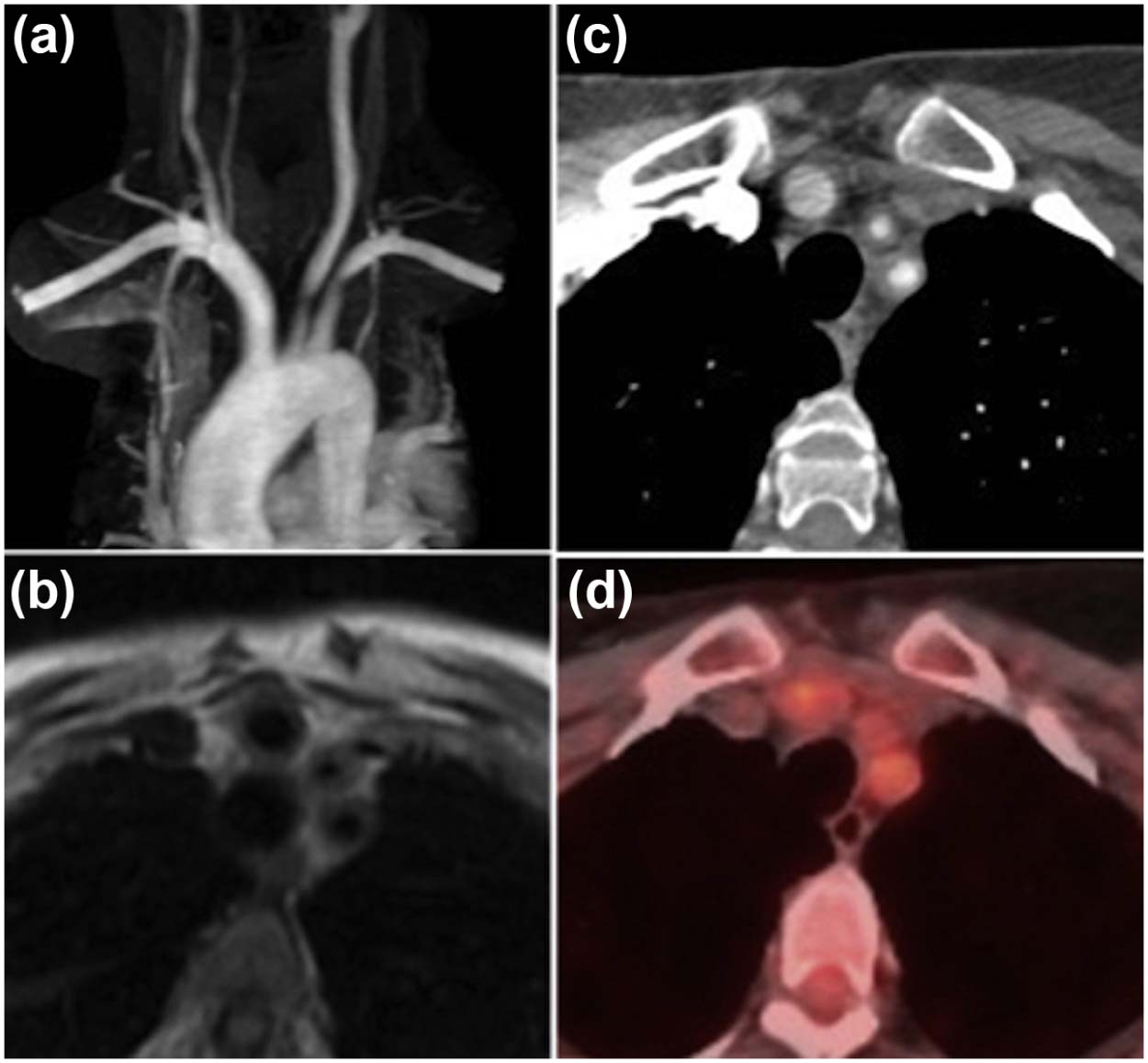
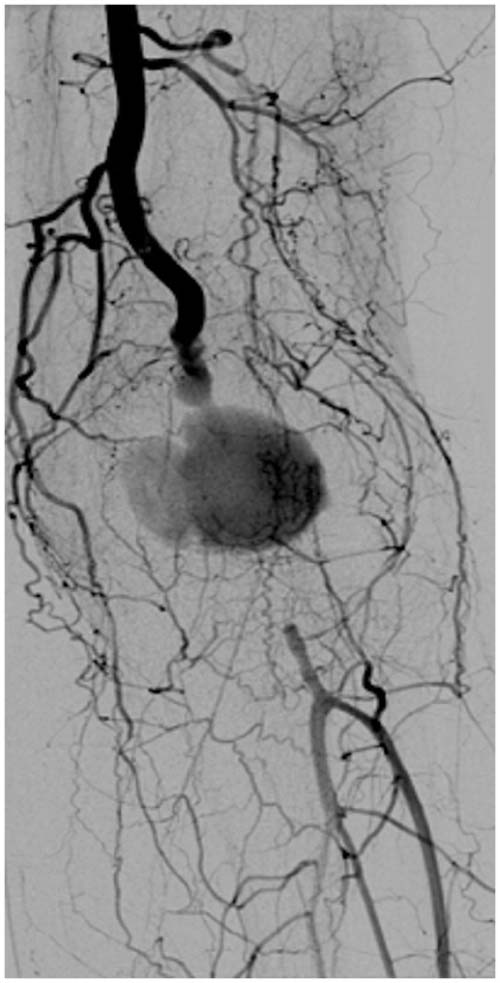
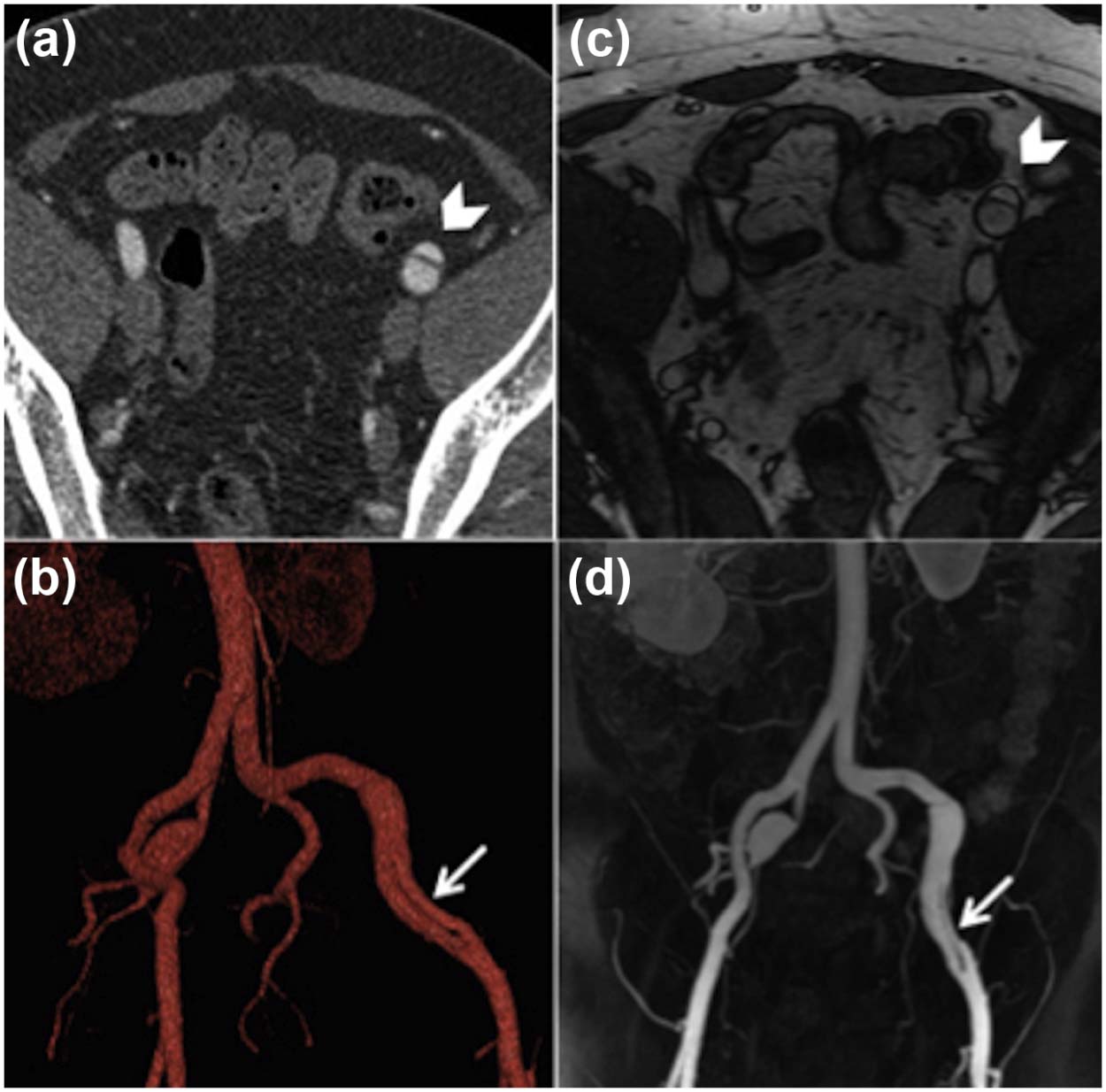
Persistent Sciatic Artery (PSA)
A PSA is a remnant of the embryological vessel that serves as the main blood supply to the lower limb during early fetal development . The persistent vessel is a direct continuation of the iliac artery to the popliteal artery and is classified in complete and incomplete types. In the complete PSA, detected in the majority of cases, there is direct communication between the internal iliac artery and the popliteal artery. This is associated with a hypoplastic short segment of superficial femoral artery that ends high in the thigh. Patients with this condition are characteristically presented with a popliteal pulse in combination with the absence of a groin pulse. In the incomplete variant, alongside a normal femoral arterial system, a partially involuted sciatic artery remains, which communicates with the popliteal artery via collaterals.
Selective catheterization of the internal iliac artery is, therefore, essential to identify this anomalous vessel to avoid a misdiagnosis of a femoral artery occlusion. Clinical findings and symptoms are a result of aneurysm formation as the sciatic artery courses through the sciatic foramen, which can be complicated by thrombosis, embolization, and sciatic nerve compression ( Fig 1 ) .
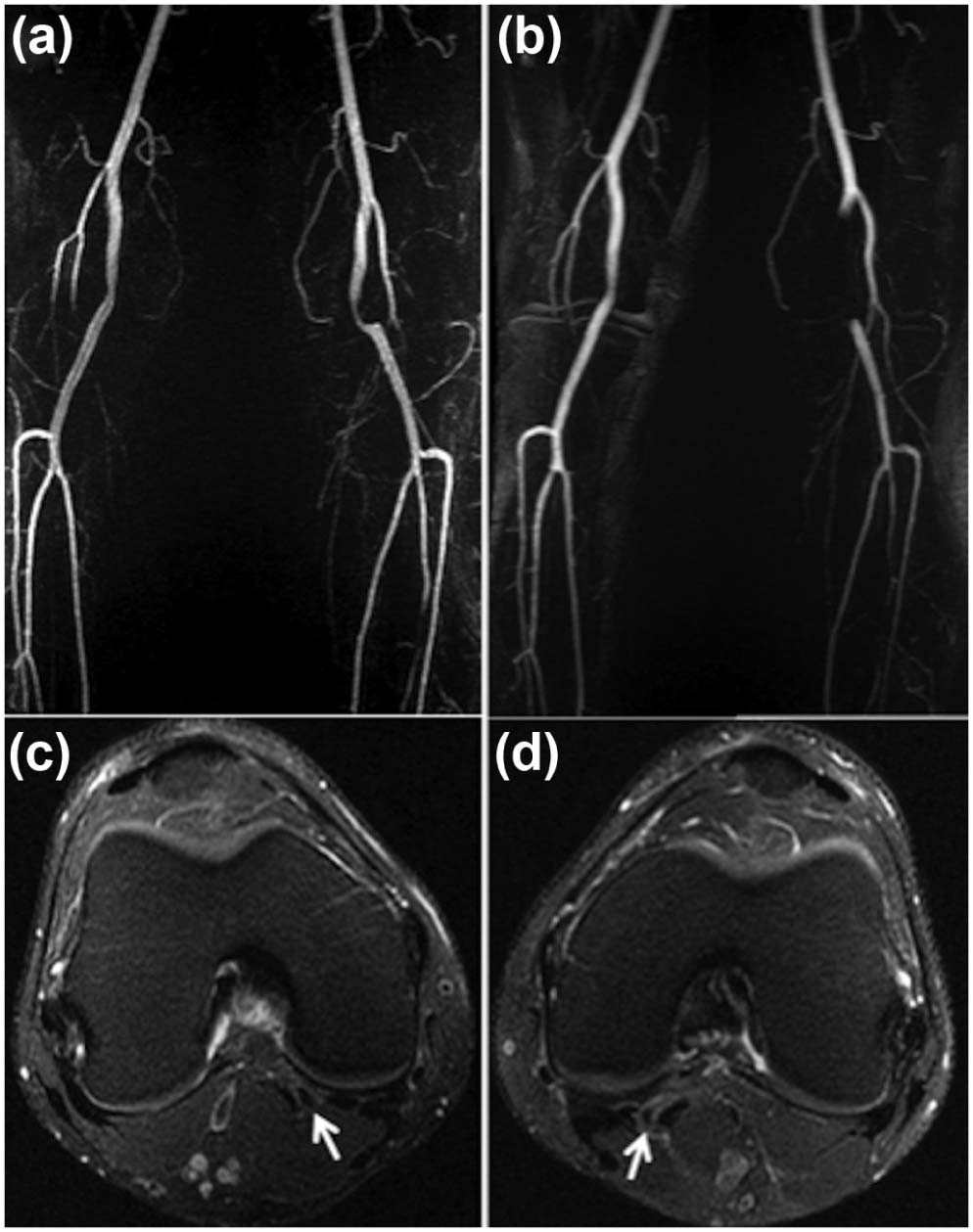
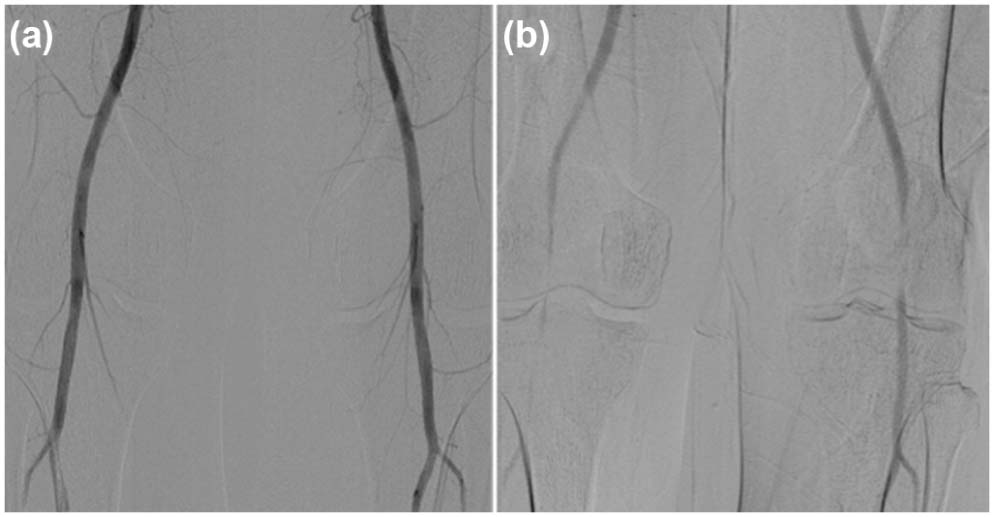
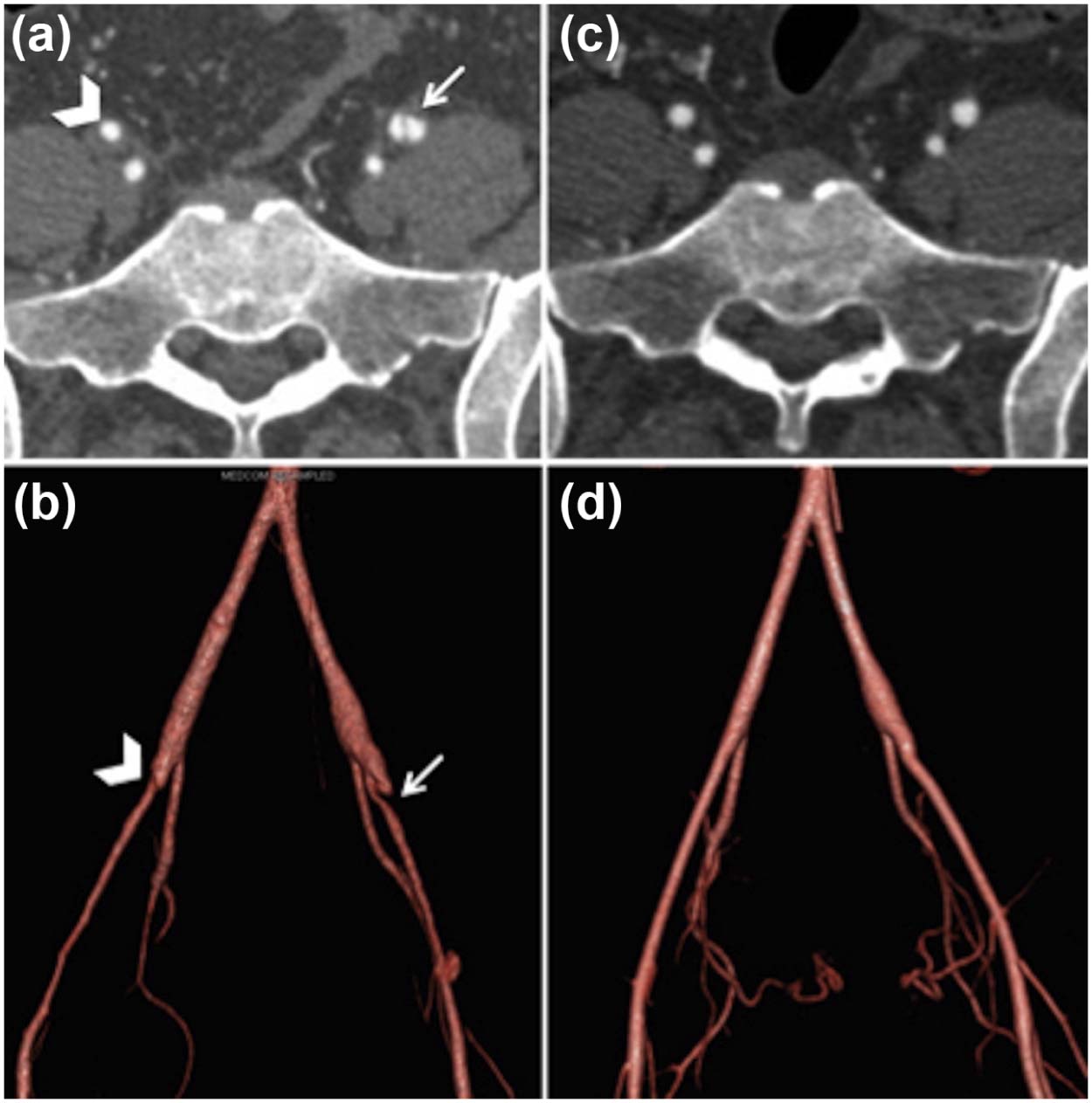
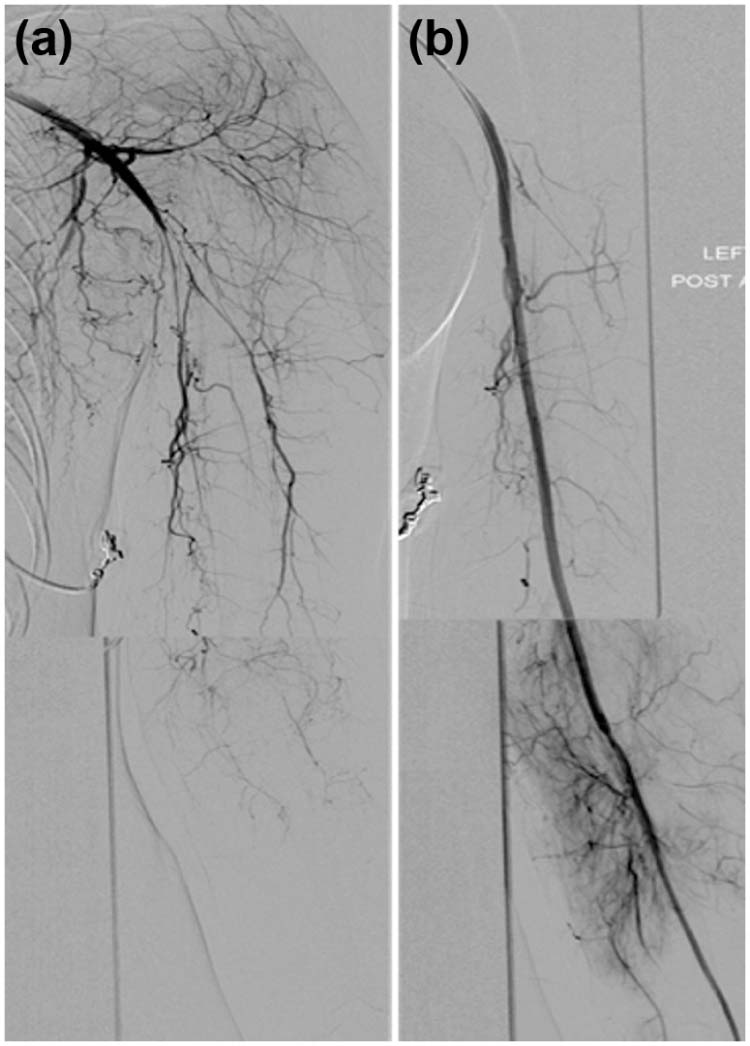
Popliteal Entrapment
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Vasculogenic
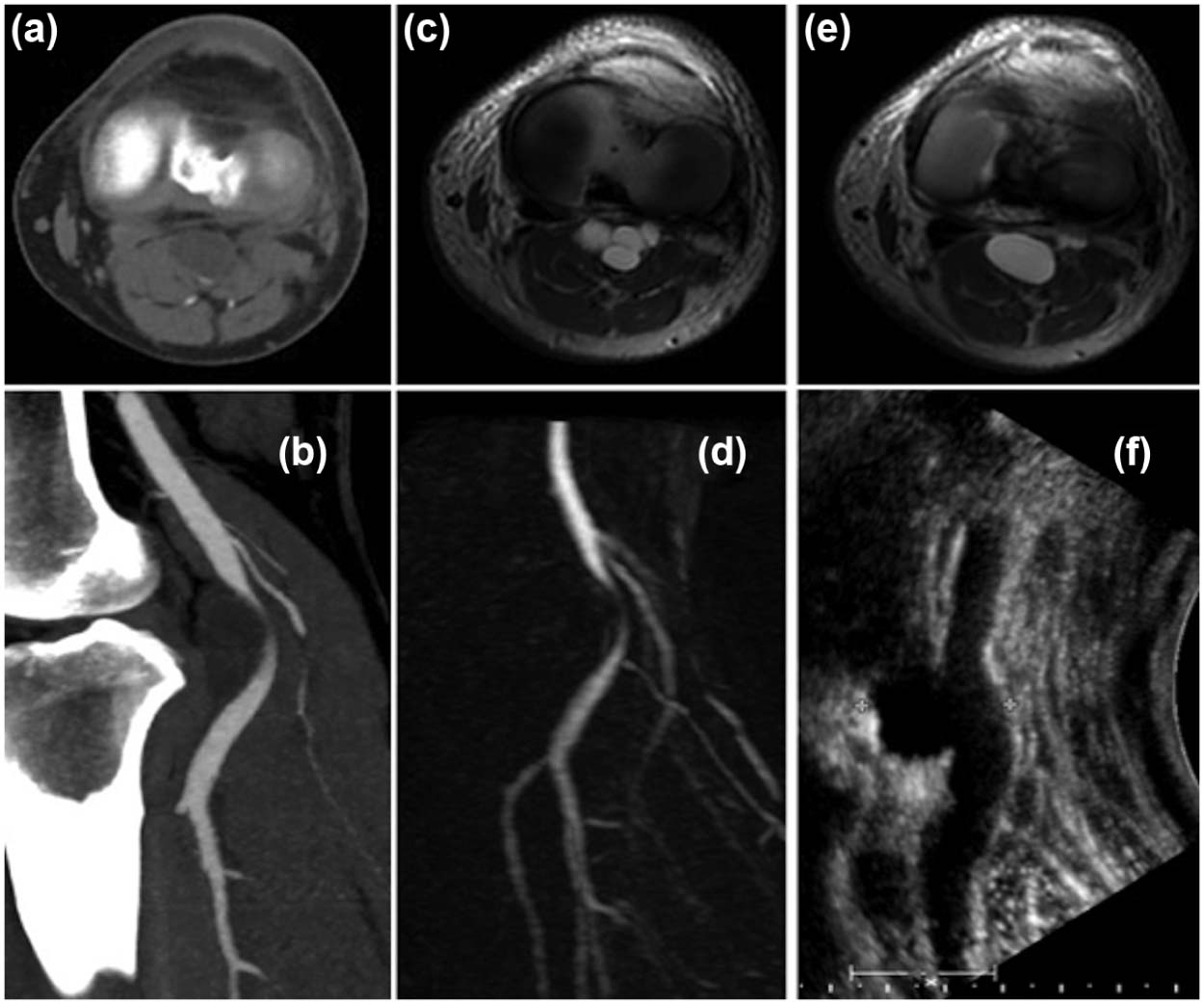
Cystic Adventitial Disease
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Iliac Endofibrosis
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Vasculitis
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Collagen Vascular Disease: Ehlers-Danlos Syndrome (EDS)
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Fibromuscular Dysplasia (FMD)
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Miscellaneous
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Conclusion
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
References
1. Weinberg I., Jaff M.R.: Nonatherosclerotic arterial disorders of the lower extremities. Circulation 2012; 126: pp. 213-222.
2. Tendera M., Aboyans V., Bartelink M.L., et. al.: ESC Guidelines on the diagnosis and treatment of peripheral artery diseases. Eur Heart J 2011; 32: pp. 2851-2906.
3. Bowlin S.J., Medalie J.H., Flocke S.A., et. al.: Epidemiology of intermittent claudication in middle-aged men. Am J Epidemiol 1994; 140: pp. 418-430.
4. Apigian A.K., Gregory J.: Basic data underlying decision making in nonatherosclerotic causes of intermittent claudication. Ann Vasc Surg 2015; 29: pp. 138-153.
5. Van Hooft I.M., Zeebregts C.J., Van Sterkenburg S.M., et. al.: The persistent sciatic artery. Eur J Vasc Endovasc Surg 2009; 37: pp. 585-591.
6. Yamamoto H., Yamamoto F., Ishibashi K., et. al.: Intermediate and long term outcomes after treating symptomatic persistent sciatic artery using different techniques. Ann Vasc Surg 2011; 25: pp. e9-e15.
7. Levien L.J., Veller M.G.: Popliteal artery entrapment syndrome: more common than previously recognized. J Vasc Surg 1999; 30: pp. 587-598.
8. Insua J.A., Young J.R., Humphries A.W.: Popliteal artery entrapment syndrome. Arch Surg 1970; 101: pp. 771-775.
9. McDonald P.T., Easterbrook J.A., Rich N.M., et. al.: Popliteal artery entrapment syndrome. Clinical, noninvasive and angiographic diagnosis. Am J Surg 1980; 139: pp. 318-325.
10. Paravastu S.C., Regi J.M., Turner D.R., et. al.: A contemporary review of cystic adventitial disease. Vasc Endovascular Surg 2012; 46: pp. 5-14.
11. Wright L.B., Matchett W.J., Cruz C.P., et. al.: Popliteal artery disease: diagnosis and treatment. Radiographics 2004; 24: pp. 467-479.
12. Levien L.J., Benn C.A.: Adventitial cystic disease: a unifying hypothesis. J Vasc Surg 1998; 28: pp. 193-205.
13. Brodmann M., Stark G., Pabst E., et. al.: Cystic adventitial degeneration of the popliteal artery—the diagnostic value of duplex. Eur J Radiol 2001; 38: pp. 209-212.
14. Stapff M., Zoller W.G., Spengel F.A.: Image directed Doppler ultrasound findings in adventitial cystic disease of the popliteal artery. J Clin Ultrasound 1989; 17: pp. 689-691.
15. Van Rutte P.W., Rouwet E.V., Belgers E.H., et. al.: In treatment of the popliteal artery cystic adventitial disease, primary bypass graft not always first choice: two case reports and a review of the literature. Eur J Vasc Endovasc Surg 2011; 42: pp. 347-354.
16. Motaganahalli R.L., Pennell R.C., Mantese V.A., et. al.: Cystic adventitial disease of the popliteal artery. J Am Coll Surg 2009; 209: pp. 541.
17. Maged J., Kron I., Hagspiel K.: Recurrent cystic adventitial disease of the popliteal artery: successful treatment with percutaneous transluminal angioplasty. Vasc Endovascular Surg 2009; 43: pp. 399-402.
18. Mertens R., Bergoeing M., Marine L., et. al.: Endovascular treatment of cystic adventitial disease of the popliteal artery. Ann Vasc Surg 2013; 27: pp. 1-3.
19. Rai S., Davies R.S., Vohra R.K.: Failure of endovascular stenting for popliteal cystic disease. Ann Vasc Surg 2009; 23: pp. 1-5.
20. Setacci F., Sirignano P., de Donato G., et. al.: Adventitial cystic disease of the popliteal artery: experience of a single vascular and endovascular center. J Cardiovasc Surg 2008; 43: pp. 235-239.
21. Shalhub S., Zierler R.E., Smith W., et. al.: Vasosapsm as a cause for claudication in athletes with external iliac artery endofibrosis. J Vasc Surg 2013; 58: pp. 105-111.
22. Rousselet M.C., Saint-Andre J.P., L’Hoste P., et. al.: Stenotic intimal thickening of the external iliac artery in competitive cyclists. Hum Pathol 1990; 21: pp. 524-529.
23. Peach G., Schep G., Palfreeman R., et. al.: Endofibrosis and kinking of the iliac arteries in athletes: a systematic review. Eur J Vasc Endovasc Surg 2012; 43: pp. 208-217.
24. Bradshaw C.: Exercise-related lower leg pain: vascular. Med Sci Sports Exerc 2000; 32: pp. 34-36.
25. Kudo T., Chandra F.A., Ahn S.S.: Long term outcomes and predictors of iliac angioplasty with selective stenting. J Vasc Surg 2005; 42: pp. 466-475.
26. Bender M.H., Schep G., Bouts S.W., et. al.: Endurance athletes with intermittent claudication caused by iliac artery stenosis treated by endarterectomy with vein patch—short- and mid-term results. Eur J Vasc Endovasc Surg 2012; 43: pp. 472-477.
27. Giannoukas A.D., Berczi V., Anoop U., et. al.: Endovascular fibrosis in high-performance athletes: diagnostic approach and minimally invasive endovascular treatment. Cardiovasc Intervent Radiol 2006; 29: pp. 866-869.
28. Johnston S.L.: Does this patient have vasculitis?. Clin Med 2011; 11: pp. 385-390.
29. Celecova Z., Krahulec B., Lizicarova D., et. al.: Vasculitis as a rare cause of intermittent claudication. Bratisl Lek Listy 2013; 114: pp. 353-356.
30. Czihal M., Tato F., Rademacher A., et. al.: Involvement of the femoropopliteal arteries in giant cell arteritis: clinical and color duplex sonography. J Rheumatol 2012; 39: pp. 314-321.
31. Assie C., Janvresse A., Plissonnier D., et. al.: Long-term follow up of upper and lower extremity vasculitis related to giant cell arteritis: a series of 36 patients. Medicine (Baltimore) 2011; 90: pp. 40-51.
32. Blockmans D., de Ceuninck L., Vancerschueren S., et. al.: Repetitive 18F-fluorodeoxyglucose positron emission tomography in giant cell arteritis: a prospective study of 35 patients. Arthritis Rheum 2006; 55: pp. 131-137.
33. Garcia Vazquez J.M., Carreira J.M., Seoane C., et. al.: Superior and inferior limb ischaemia in giant cell arteritis: angiography follow-up. Clin Rheumatol 1999; 18: pp. 61-65.
34. Pipitone N., Versari A., Salvarani C.: Role of imaging studies in the diagnosis and follow-up of large-vessel vasculitis: an update. Rheumatology (Oxford) 2008; 47: pp. 403-408.
35. Both M., Aries P.M., Muller-Hulsbeck S., et. al.: Balloon angioplasty of arteries of the upper extremities in patients with extracranial giant-cell arteritis. Ann Rheum Dis 2006; 65: pp. 1124-1130.
36. Loo Z.Y., Thwaites S., Kyaw P.: Giant cell arteritis presenting as critical lower limb ischaemia. Vasc Endovascular Surg 2013; 47: pp. 660-662.
37. Shionoya S.: Diagnostic criteria of Buerger’s disease. Int J Cardiol 1998; 1: pp. 243-245.
38. Olin J.W.: Thromboangiitis obliterans (Buerger’s disease). N Engl J Med 2000; 343: pp. 864-869.
39. Arkkila P.E.: Thromboangiitis obliterans (Buerger’s disease). Orphanet J Rare Dis 2006; 1: pp. 14.
40. Johnston S.L., Lock R.J., Gompels M.M.: Takayasu arteritis: a review. J Clin Pathol 2002; 55: pp. 481-486.
41. Sheikhzadeh A., Tettenborn I., Noohi F., et. al.: Occlusive thromboaortopathy (Takayasu disease): clinical and angiographic features and a brief review of literature. Angiology 2002; 53: pp. 29-40.
42. Anthony W., Stanson M.D., Jeremy L., et. al.: Polyarteritis nodosa: spectrum of angiographic findings. Radiographics 2001; 21: pp. 151-159.
43. Ninomiya T., Sugimoto T., Tanaka Y., et. al.: Symmetric peripheral gangrene as an emerging manifestation of polyarteritis nodosa. J Rheumatol 2007; 34: pp. 440-441.
44. Ewald E.A., Griffin D., McCune W.J.: Correlation of angiographic abnormalities with disease manifestations and disease severity in polyarteritis nodosa. J Rheumatol 1987; 14: pp. 952-956.
45. Cabero Moyano J., Andreu Magarolas M., Castaner González E., et. al.: Patología aórtica no urgente: diagnóstico clínico-radiológico de la aortitis. Radiologia 2013; 55: pp. 469-482.
46. Superti-Furga A., Gugler E., Gitzelmann R., et. al.: Ehlers Danlos Syndrome Type IV: a multi-exon deletion in one of the two col3a1 alleles affecting structure, stability, and processing of type III procollagen. J Biol Chem 1988; 263: pp. 6226-6232.
47. Saadoun D., Wechsler B.: Behcet’s disease. Orphanet J Rare Dis 2012; 7: pp. 20.
48. Ko G.Y., Byun J.Y., Choi B.G., et. al.: The vascular manifestations of Behçet’s disease: angiographic and CT findings. Br J Radiol 2000; 73: pp. 1270-1274.
49. Pauker S., Stoler J.: Clinical manifestations and diagnosis of Ehlers-Danlos syndromes. 8 July http://www.uptodate.com/contents/clinical-manifestations-and-diagnosis-of-ehlers-danlos-syndromes
50. Eder J., Laccone F., Rohrbach M., et. al.: A new COL3A1 mutation in Ehlers–Danlos syndrome type IV. Exp Dermatol 2013; 22: pp. 231-234.
51. Slovut D.P., Olin J.W.: Fibromuscular dysplasia. N Engl J Med 2004; 29: pp. 1862-1871.
52. Harrison E.G., McCormack L.J.: Pathologic classification of renal arterial disease in renovascular hypertension. Mayo Clin Proc 1971; 46: pp. 161-167.
53. Okazaki J., Guntani A., Homma K., et. al.: Fibromuscular dysplasia of the lower extremities. Ann Vasc Dis 2011; 4: pp. 143-149.
54. Iida O., Nanto S., Uematsu M., et. al.: Endovascular therapy for limb salvage in a case of critical limb ischaemia resulting from fibromuscular dysplasia. J Vasc Surg 2007; 46: pp. 803-807.
55. Fonkalsrud E.W., Sanchez M., Zerubavel R., et. al.: Serial changes in arterial structure following radiation therapy. Surg Gynecol Obstet 1977; 145: pp. 395-400.
56. Rodemann H.P., Bamberg M.: Cellular basis of radiation-induced fibrosis. Radiother Oncol 1995; 35: pp. 83-90.
57. Bashar K., Healy D., Clarke-Moloney M., et. al.: Effects of neck radiation therapy on extra-cranial carotid arteries atherosclerosis disease prevalence: systematic review and a meta-analysis. PLoS ONE 2014; 9: e110389
58. Jurado J.A., Bashir R., Burket M.W.: Radiation-induced peripheral artery disease. Catheter Cardiovasc Interv 2008; 72: pp. 563-568.
59. Farrugia M., Gowda K.M., Cheatle T.R., et. al.: Radiotherapy-related axillary artery occlusive disease: percutaneous transluminal angioplasty and stenting. Two case reports and review of the literature. Cardiovasc Intervent Radiol 2006; 29: pp. 1144-1147.
60. Marder V.J., Mellinghoff I.K.: Cocaine and Buerger disease: is there a pathogenic association?. Arch Intern Med 2000; 160: pp. 2057-2060.
61. Zhou W., Lin P.H., Bush R.L., et. al.: Acute arterial thrombosis associated with cocaine abuse. J Vasc Surg 2004; 40: pp. 291-295.
62. Collins C.G., Seoighe D., Ireland A., et. al.: Cocaine-associated lower limb ischemia. Vascular 2008; 16: pp. 297-299.
63. Hohenberger P., Allenberg J.R., Schlag P.M., et. al.: Results of surgery and multimodal therapy for patients with soft tissue sarcoma invading to vascular structures. Cancer 1999; 85: pp. 396-408.
64. McDonald D.K., Kalva S.P., Fan C.M., et. al.: Leiomyosarcoma of the uterus with intravascular tumor extension and pulmonary tumor embolism. Cardiovasc Intervent Radiol 2007; 30: pp. 140-142.
65. Lacroix H., Menten J., Nevelsteen A., et. al.: Lower extremity acute ischaemia due to a metastatic breast fibrosarcoma embolism. Eur J Vasc Surg 1994; 8: pp. 639-641.
66. Tierney K.E., Rogers A., Mhawech-Fauceglia P., et. al.: Recurrent leiomyosarcoma presenting as malignant arterial tumor thrombus. Gynecol Oncol Case Rep 2013; 4: pp. 32-34.
67. Abulafia O., Sclafani S.J., Holcomb K., et. al.: Percutaneous transluminal endovascular graft placement for massive hemorrhage caused by recurrent cervical carcinoma-associated erosion of the external iliac artery. Am J Obstet Gynecol 1998; 178: pp. 618-620.
68. Nassiri N., Kogan S., Gibbon D.G., et. al.: Multimodal endovascular palliation for femoral arterial blowout in the setting of metastatic vulvar carcinoma. Ann Vasc Surg 2015; 29: pp. 127. e11-5