Rationale and Objectives
Completing a systems-based practice project, equivalent to a practice quality improvement project (PQI), is a residency requirement by the Accreditation Council for Graduate Medical Education and an American Board of Radiology milestone. The aim of this study was to assess the residents’ perspectives on quality improvement projects in radiology.
Materials and Methods
Survey data were collected from 154 trainee members of the Association of University Radiologists to evaluate the residents’ views on PQI.
Results
Most residents were aware of the requirement of completing a PQI project and had faculty mentors for their projects. Residents who thought it was difficult to find a mentor were more likely to start their project later in residency ( P < .0001). Publication rates were low overall, and lack of time was considered the greatest obstacle. Having dedicated time for a PQI project was associated with increased likelihood of publishing or presenting the data ( P = .0091). Residents who rated the five surveyed PQI steps (coming up with an idea, finding a mentor, designing a project, finding resources, and finding time) as difficult steps were more likely to not have initiated a PQI project ( P < .0001 for the first four and P = .0046 for time).
Conclusion
We present five practical areas of improvement to make PQI a valuable learning experience: 1) Increasing awareness of PQI and providing ideas for projects, 2) encouraging faculty mentorship and publication, 3) educating residents about project design and implementation, 4) providing resources such as books and funds, and 5) allowing dedicated time.
The world of health care is rapidly changing, and a significant component of that change is the emphasis on accountability to the public for the quality of medical practice. Quality improvement (QI) in medicine has become vital to the daily practice of physicians and the training of future physicians. QI in radiology encompasses improving the effectiveness of diagnostic and therapeutic procedures, selecting the appropriate imaging services, ensuring safety and quality of services delivered, and overseeing the efficiency and management of all imaging services . To highlight the importance of QI, the American Board of Radiology made Practice Quality Improvement (PQI) one of the four core components for Maintenance of Certification (MOC). At least 23 other medical specialty boards besides the American Board of Radiology (ABR) have a requirement for some form of practice improvement under the MOC plan developed by the American Board of Medical Specialties in 2000 . When MOC was officially introduced in 2007 by the ABR, radiologists were only required to perform one PQI project every 10 years . The requirements were then adjusted to three PQI projects every 10 years . Recently, with the introduction of “continuous certification,” the expected change in requirement to one project every 3 years occurred . All the current residents in radiology programs nationally will be certified under this new ABR requirement, and preparing residents for the future has become a vital component of training across the country.
Additionally, one of the six core competencies of the Accreditation Council for Graduate Medical Education (ACGME) during residency is systems-based practice (SBP) . Systems-based practice is defined by the ACGME as “awareness of and responsiveness to the larger context and system of health care and the ability to effectively call on system resources to provide care that is of optimal value” . Since 2008, the ACGME has required participation of radiology residents in at least one systems-based practice project with documentation of participation in such an activity . The ABR has formally incorporated this requirement as one of the 12 required milestones to be achieved by radiology residents during their training . SBP is a challenging competency to define, teach, and evaluate and was reported to be the most difficult competency to implement in radiology residency programs in the 2005 annual survey of the Association of Program Directors in Radiology .
Get Radiology Tree app to read full this article<
Materials and methods
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Results
Overview of Participants, Awareness of QI Projects, and Topics Covered
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Table 1
American Board of Radiology Practice Quality Improvement Categories of Resident-Led Projects by PGY
Patient Safety Accuracy of Interpretation Report Timeliness Practice Guidelines and Technical Standards Referring Physician Surveys PGY-2 25 ∗ 37.5 0 37.5 0 PGY-3 24.53 16.98 13.21 39.62 5.66 PGY-4 20 16.67 0 56.67 6.67 PGY-5 21.43 21.43 28.57 21.43 7.14
PGY, postgraduate year.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
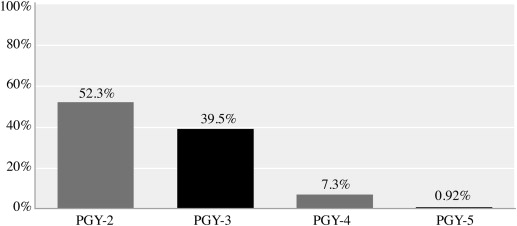
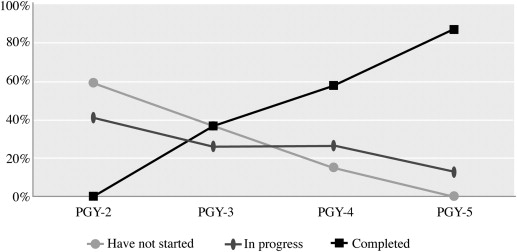
Timeframe of QI Projects
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
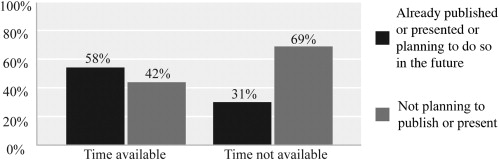
Institutional QI Policy, Faculty Mentorship, and Publication of QI Projects
Get Radiology Tree app to read full this article<
Table 2
Availability of Dedicated QI Process and Time, Faculty Mentorship, and Publication/Presentation Rates of QI Projects among Surveyed Residents
Yes No Availability of a QI process 71 ∗ 29 Availability of time for QI 26 74 Faculty mentorship 81 19 Publication/presentation of a QI project or plans to do so in the future 39 61
QI, quality improvement.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Hindrances Encountered during QI Initiatives
Get Radiology Tree app to read full this article<
Table 3
Resident Rating of Each of the Five Surveyed Quality Improvement Steps by PGY
Coming up with an Idea Finding a Mentor Designing and Implementing a Project Finding Resources Finding Time PGY-2 Very easy 0 ∗ 10 0 0 0 Easy 20 70 30 50 10 Somewhat difficult 70 20 70 50 70 Difficult 10 0 0 0 10 Very difficult 0 0 0 0 10 PGY-3 Very easy 19 32 7 7 3 Easy 46 54 44 49 19 Somewhat difficult 25 5 33 26 32 Difficult 5 5 9 9 23 Very difficult 5 4 7 9 23 PGY-4 Very easy 21 16 6 6 0 Easy 38 36 26 41 15 Somewhat difficult 29 36 47 25 37 Difficult 12 6 21 22 21 Very difficult 0 6 0 6 27 PGY-5 Very easy 13 20 7 7 13 Easy 60 60 73 53 34 Somewhat difficult 20 7 13 26 20 Difficult 7 13 7 7 20 Very difficult 0 0 0 7 13
PGY, postgraduate year.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Discussion
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Appendix
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
References
1. Kruskal J.B., Eisenberg R., Sosna J., et. al.: Quality initiatives: quality improvement in radiology: basic principles and tools required to achieve success. Radiographics 2011; 31: pp. 1499-1509.
2. ABMS Maintenance of Certification. Available at: http://www.abms.org/maintenance_of_certification/ABMS_MOC.aspx . Accessed October 1, 2013.
3. Kouo T.: Experience with a practice quality improvement system in a university radiology department. J Am Coll Radiol 2012; 9: pp. 814-819.
4. Maintenance of Certification Part IV: ABR Guide to Practice Quality Improvement 2012. Available at: http://www.theabr.org/sites/all/themes/abr-media/pdf/PQI_2012.pdf . Accessed October 1, 2013.
5. Dyne P.L., Strauss R.W., Rinnert S.: Systems-based practice: the sixth core competency. Acad Emerg Med 2002; 9: pp. 1270-1277.
6. Amis E.S.: New program requirements for diagnostic radiology: update and discussion of the more complex requirements. AJR Am J Roentgenol 2008; 190: pp. 2-4.
7. The Diagnostic Radiology Milestone Project. Available at: http://www.acgme-nas.org/assets/pdf/Milestones/DiagnosticRadiologyMilestones.pdf . Accessed October 7, 2013.
8. Johnson J.K., Miller S.H., Horowitz S.D.: Systems-based practice: improving the safety and quality of patient care by recognizing and improving the systems in which we work.Henriksen K.Battles J.B.Keyes M.A. et. al.Advances in patient safety: new directions and alternative approaches.2008.Agency for Healthcare Research and QualityRockville, MD: Available at: http://www.ncbi.nlm.nih.gov/books/NBK43731/
9. Buchmann R.F., Deloney L.A., Donepudi S.K., et. al.: Development and implementation of a systems-based practice project requirement for radiology residents. Acad Radiol 2008; 15: pp. 1040-1045.
10. Thrall J.H.: Quality and safety revolution in health care. Radiology 2004; 233: pp. 3-6.
11. Krajewski K., Siewert B., Yam S., et. al.: A quality assurance elective for radiology residents. Acad Radiol 2007; 14: pp. 239-245.
12. Relyea-Chew A., Talner L.B.: A dedicated general competencies curriculum for radiology residents development and implementation. Acad Radiol 2011; 18: pp. 650-654.
13. Brandon C.J., Mullan P.B.: Teaching medical management and operations engineering for systems-based practice to radiology residents. Acad Radiol 2013; 20: pp. 345-350.
14. Deitch C.H., Chan W.C., Sunshine J.H., et. al.: Quality assessment and improvement: what radiologists do and think. AJR Am J Roentgenol 1994; 163: pp. 1245-1254.
15. Boonyasai R.T., Windish D.M., Chakraborti C., et. al.: Effectiveness of teaching quality improvement to clinicians: a systematic review. JAMA 2007; 298: pp. 1023-1037.
16. Patow C.A., Karpovich K., Riesenberg L.A., et. al.: Residents’ engagement in quality improvement: a systematic review of the literature. Acad Med 2009; 84: pp. 1757-1764.
17. Wong B.M., Etchells E.E., Kuper A., et. al.: Teaching quality improvement and patient safety to trainees: a systematic review. Acad Med 2010; 85: pp. 1425-1439.
18. Gaught A.M., Cleveland C.A., Hill J.J.: Publish or perish? Physician research productivity during residency training. Am J Phys Med Rehabil 2013; 92: pp. 710-714.
19. Eliastam M., Mizrahi T.: Quality improvement, housestaff, and the role of chief residents. Acad Med 1996; 71: pp. 670-674.
20. Francis M.D., Varney A.J.: Learning by doing: use of resident-led quality improvement projects to teach clinical practice improvement. Hosp Physician 2006; 42: pp. 52-57.
21. Weingart S.N., Tess A., Driver J., et. al.: Creating a quality improvement elective for medical house officers. J Gen Intern Med 2004; 19: pp. 861-867.
22. Weingart S.N.: A house officer-sponsored quality improvement initiative: Leadership lessons and liabilities. Jt Comm J Qual Improv 1998; 24: pp. 371-378.
23. Headrick L.A., Richardson A., Priebe G.P.: Continuous improvement learning for residents. Pediatrics 1998; 101: pp. 768-773.