Rationale and Objectives
Transjugular intrahepatic portosystemic shunt (TIPS) is an established method for portal hypertension. This study was to investigate the long-term safety, technical success, and patency of TIPS, and to determine the risk factors and clinical impacts of shunt dysfunction.
Materials and Methods
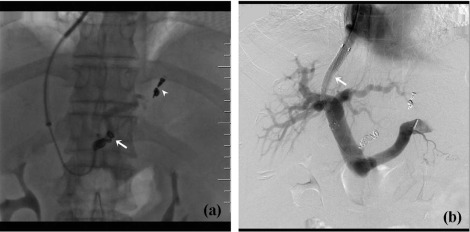
A total of 154 consecutive patients undergoing embolotherapy of gastric coronary vein and/or short gastric vein and TIPS creation were prospectively studied. Follow-up data included technical success, patency and revision of TIPS, and overall survival of patients.
Results
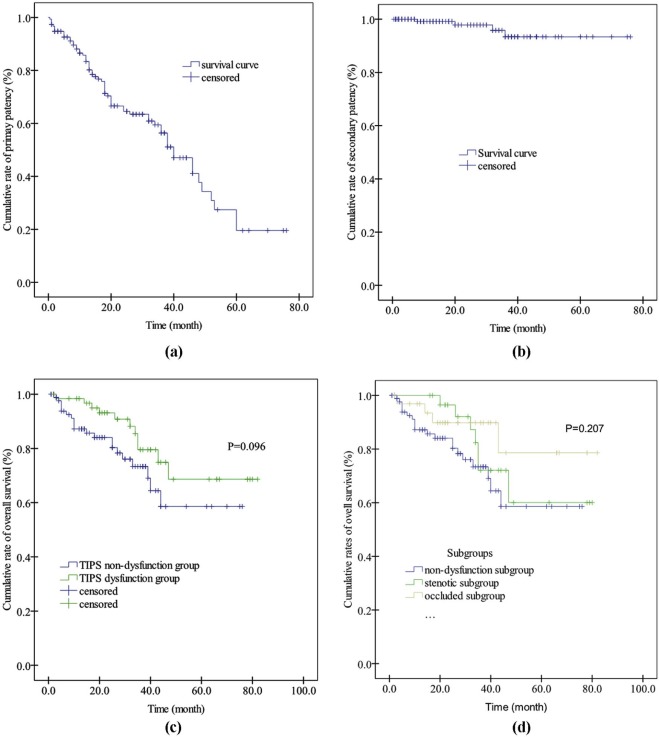
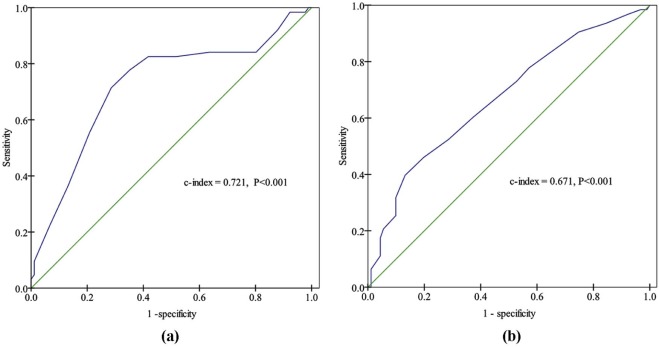
During the study, the primary and secondary technical success rates were 98.7% and 100%, respectively. Sixty-three patients developed shunt dysfunction, 30 with shunt stenosis and 33 with shunt occlusion. The cumulative 60-month primary, primary assisted, and secondary patency rates were 19.6%, 43.0%, and 93.4%, respectively. The cumulative 60-month overall survival rates were similar between the TIPS dysfunction group and the TIPS non-dysfunction group (68.6% vs. 58.6%, P = .096). Baseline portal vein thrombosis ( P < .001), use of bare stents ( P = .018), and portal pressure gradient (PPG) ( P = .020) were independent predictors for shunt dysfunction, hepatocellular carcinoma ( P < .001), and ascites ( P = .003) for overall survival. The accuracy of PPG for shunt dysfunction was statistically significant ( P < .001), and a cutoff value of 8.5 had 77.8% sensitivity and 64.8% specificity.
Conclusions
The long-term safety, technical success, and patency of TIPS were good; baseline portal vein thrombosis, use of bare stents, and PPG were significantly associated with shunt dysfunction; shunt dysfunction has little impact on patients’ long-term survival because of high secondary patency rates.
Introduction
Transjugular intrahepatic portosystemic shunt (TIPS) is an established method to manage sequelae of portal hypertension, that is, variceal hemorrhage and refractory ascites . Initially, TIPS was created by using bare metal stents that led to high rates of shunt dysfunction, often above 50% at 1 year . Shunt dysfunction is associated with recurrence of ascites and variceal hemorrhage , which requires sometimes repeated revisions that bear additional procedural risks and expenses . After the advent of expanded polytetrafluoroethylene (ePTFE)-covered stent grafts, numerous studies have demonstrated that ePTFE-covered stent grafts are better than bare metal stents in long-term patency .
However, shunt dysfunction remains a major concern of TIPS creation with ePTFE-covered stent grafts in the long run. Weber et al. reported that shunt patency rates gradually decreased, mortality rates continued to increase, and the chance of recurrent ascites or bleeding remained present beyond 2 years after TIPS creation with ePTFE-covered stent grafts. Except the type of stent used, there are limited data regarding the risk factors for shunt dysfunction and its impact on clinical outcomes in patients who underwent TIPS creation to prevent variceal rebleeding with ePTFE-covered stent grafts .
Get Radiology Tree app to read full this article<
Materials and Methods
Patients
Get Radiology Tree app to read full this article<
TIPS Procedure
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Follow-up Protocol
Get Radiology Tree app to read full this article<
Shunt Dysfunction and TIPS Revisions
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Diagnosis and Definitions
Get Radiology Tree app to read full this article<
Statistical Analysis
Get Radiology Tree app to read full this article<
Results
Patient Characteristics
Get Radiology Tree app to read full this article<
Table 1
Baseline Characteristics
Variables Results Patients ( n = 154) Sex: male, n (%) 101 (65.6) Age 52.1 ± 10.8 Etiology, n (%) Hepatitis B virus 74 (48.1) Hepatitis C virus 26 (16.9) Alcohol 14 (9.1) Autoimmune liver disease 10 (6.5) Cryptogenic 30 (19.5) Spleen surgery, n (%) Splenectomy 5 (3.2) Partial splenic embolization 2 (1.3) Thrombosis within the portal venous system, n (%) 53 (34.4) Comorbidity, n (%) Diabetes mellitus 38 (24.7) Hypertension 5 (3.2) Hepatocellular carcinoma 17 (11.0) Endoscopic varices, n (%) Gastroesophageal varices 113 (72.9) Esophageal varices 41 (26.6) Ascites, n (%) None 88 (57.1) Mild 35 (22.7) Moderate to severe 31 (20.1) White blood cell count (3.5–9.5 × 10 9 /L) 2.71 (IQR: 2.08–3.78) Hemoglobulin (female:115–150 g/L; male:130–175 g/L) 87.7 ± 18.9 Platelet count (125–350 × 10 9 /L) 56.0 (IQR: 48.0–77.0) Prothrombin time (10.0-16.0 s) 19.6 ± 3.7 International normalized ratio 1.64 ± 0.33 Albumin (35–50 g/L) 28.9 ± 4.9 Alanine aminotransferase (5–40 U/L) 25.5 (IQR: 18.0–41.0) Aspartate aminotransferase (8–40 U/L) 42.5 (IQR: 31.0–60.0) Total bilirubin (3.4–20.5 µmol/L) 29.4 (IQR: 19.6–39.5) direct bilirubin (0.0–6.8 µmol/L) 12.9 (IQR: 8.8–17.9) Creatinine (53–97 µmol/L) 68.0 (IQR: 59.0–78.0) Child-Turcotte-Pugh score 8.0 (IQR: 7.0–9.0) Child class, n (%) A 32 (20.8) B 96 (62.3) C 26 (16.9) Model for end stage liver disease score 10.5 ± 4.3 Stent site, n (%) From middle hepatic vein to left portal branch 94 (61.0) From right hepatic vein to right portal branch 42 (27.3) From inferior vena cava to the portal vein 18 (11.7) Stent number, n (%) One stent 105 (68.2) Two stents 47 (30.5) Three stents 2 (1.3) ePTFE-covered stent, n (%) 8 mm × 40 mm 19 (12.3) 8 mm × 60 mm 103 (66.9) 8 mm × 80 mm 32 (20.8) Bare stent, n (%) 8 mm × 40 mm 5 (3.2) 8 mm × 60 mm 32 (20.8) 8 mm × 80 mm 7 (4.5) Baseline portal pressure (mm Hg) 28.0 (IQR: 25.0–32.0) Postoperative portal pressure (mm Hg) 19.0 (IQR: 15.0–22.0) Intrashunt pressure (mm Hg) 10.5 (IQR: 9.0–12.0) Right atrial pressure (mm Hg) 7.0 (IQR: 5.0–9.3) Portal pressure reduction (mm Hg) 8.0 (IQR: 6.0–12.0) Portosystemic venous collaterals, n (%) Short gastric vein 21 (13.6) Coronary gastric vein 66 (42.9) Both short gastric and coronary vein 67 (43.5) Spontaneous shunts, n (%) Splenorenal shunt 12 (7.8) Intrahepatic arteriovenous fistula 4 (2.6) Gastrorenal shunt 1 (0.6)
ePTFE, expanded polytetrafluoroethylene.
Get Radiology Tree app to read full this article<
TIPS Procedure and Complications
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Shunt Dysfunction, Primary Patency Rate, and Risk Factors
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Table 2
Univariate and multivariate analysis for the factors predictive of shunt dysfunction
Baseline factors Univariate analysis Multivariate analysis HR 95%CI_P_ Value HR 95%CI_P_ Value Baseline PVT 3.561 2.151–5.895 .000 4.544 2.643–7.810 .000 Bare stent use \* 0.356 0.215–0.589 .000 0.377 0.167–0.848 .018 PPR 0.870 0.809–0.936 .000 0.913 0.846–0.986 .020 Stent number 1.720 1.145–2.585 .009 Bare stent type § 1.347 1.056–1.718 .017 Postoperative portal pressure 1.077 1.027–1.129 .002
CI, confidence interval; HR, Hazard ratio; PPR, portal pressure reduction before and after TIPS creation; PVT, thrombosis at any site of the portal venous system.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
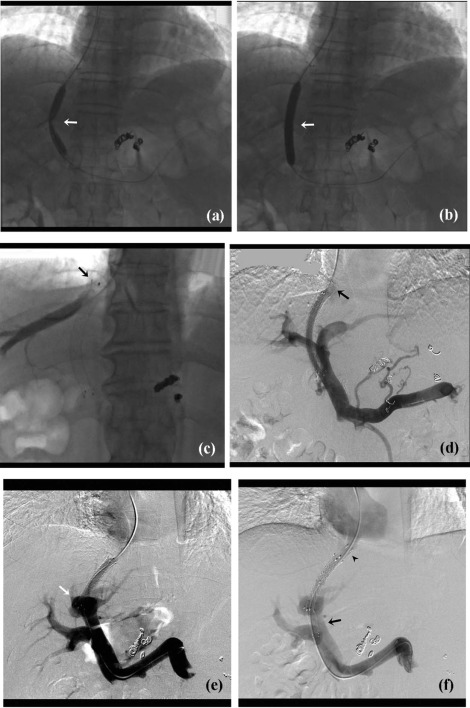
Shunt Occlusion, Primary Assisted Patency Rate, and Risk Factors
Get Radiology Tree app to read full this article<
Shunt Revision and Secondary Patency Rate
Get Radiology Tree app to read full this article<
Impacts of Shunt Dysfunction on Overall Survival
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Table 3
Univariate and Multivariate Analysis for the Factors Predictive of Overall Survival
Baseline Factors Univariate Analysis Multivariate Analysis HR 95%CI_P_ Value HR 95%CI_P_ Value HCC 9.234 4.229–20.164 .000 6.615 2.863–15.283 .000 Ascites \* 1.788 1.148–2.784 .010 2.166 1.298–3.615 .003 Right atrium pressure 1.117 1.002–1.244 .045 Age 1.048 1.016–1.081 .003 WBC 0.659 0.481–0.904 .010
CI, confidence interval; HCC, hepatocellular carcinoma; HR, hazard ratio; WBC, white blood cell count.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Discussion
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Conclusions
Get Radiology Tree app to read full this article<
Supplementary Data
Get Radiology Tree app to read full this article<
Appendix S1
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
References
1. Suhocki P.V., Lungren M.P., Kapoor B., et. al.: Transjugular intrahepatic portosystemic shunt complications: prevention and management. Semin Intervent Radiol 2015; 32: pp. 123-132.
2. Sanyal A.J., Freedman A.M., Luketic V.A., et. al.: The natural history of portal hypertension after transjugular intrahepatic portosystemic shunts. Gastroenterology 1997; 112: pp. 889-898.
3. Tan H.K., James P.D., Sniderman K.W., et. al.: Long-term clinical outcome of patients with cirrhosis and refractory ascites treated with transjugular intrahepatic portosystemic shunt insertion. J Gastroenterol Hepatol 2015; 30: pp. 389-395.
4. Casado M., Bosch J., Garcia-Pagan J.C., et. al.: Clinical events after transjugular intrahepatic portosystemic shunt: correlation with hemodynamic findings. Gastroenterology 1998; 114: pp. 1296-1303.
5. Zurera L.J., Espejo J.J., Lombardo S., et. al.: Safety and efficacy of expanded polytetrafluoroethylene-covered transjugular intrahepatic portosystemic shunts in children with acute or recurring upper gastrointestinal bleeding. Pediatr Radiol 2015; 45: pp. 422-429.
6. Perarnau J.M., Le Gouge A., Nicolas C., et. al.: Covered vs. uncovered stents for transjugular intrahepatic portosystemic shunt: a randomized trial. J Hepatol 2014; 60: pp. 962-968.
7. Di Giorgio A., Agazzi R., Alberti D., et. al.: Feasibility and efficacy of transjugular intrahepatic portosystemic shunt (TIPS) in children. J Pediatr Gastroenterol Nutr 2012; 54: pp. 594-600.
8. Yang Z., Han G., Wu Q., et. al.: Patency and clinical outcomes of transjugular intrahepatic portosystemic shunt with polytetrafluoroethylene-covered stents versus bare stents: a meta-analysis. J Gastroenterol Hepatol 2010; 25: pp. 1718-1725.
9. Sommer C.M., Gockner T.L., Stampfl U., et. al.: Technical and clinical outcome of transjugular intrahepatic portosystemic stent shunt: bare metal stents (BMS) versus viatorr stent-grafts (VSG). Eur J Radiol 2012; 81: pp. 2273-2280.
10. Boyer T.D., Haskal Z.J.: The role of transjugular intrahepatic portosystemic shunt (TIPS) in the management of portal hypertension: update 2009. Hepatology 2010; 51: pp. 306.
11. Bureau C., Garcia-Pagan J.C., Otal P., et. al.: Improved clinical outcome using polytetrafluoroethylene-coated stents for TIPS: results of a randomized study. Gastroenterology 2004; 126: pp. 469-475.
12. Weber C.N., Nadolski G.J., White S.B., et. al.: Long-term patency and clinical analysis of expanded polytetrafluoroethylene–covered transjugular intrahepatic portosystemic shunt stent grafts. J Vasc Interv Radiol 2015; 26: pp. 1257-1265.
13. Qi X., Guo W., He C., et. al.: Transjugular intrahepatic portosystemic shunt for Budd-Chiari syndrome: techniques, indications and results on 51 Chinese patients from a single centre. Liver Int 2014; 34: pp. 1164-1175.
14. Hayek G., Ronot M., Plessier A., et. al.: Long-term outcome and analysis of dysfunction of transjugular intrahepatic portosystemic shunt placement in chronic primary Budd-Chiari syndrome. Radiology 2017; 283: pp. 280-292.
15. Yue-Meng W., Li Y.H., Wu H.M., et. al.: Portal vein thrombosis in patients with cirrhosis undergoing elective transjugular intrahepatic portosystemic shunt: risk factors, warfarin efficacy, and clinical outcomes. Clin Appl Thromb Hemost 2017; 1: 1076029616689593. [Epub ahead of print]
16. Cai J., Guo W., He C., et. al.: Shunt dysfunction: is it suitable as the primary end point in transjugular intrahepatic portosystemic shunt trials?. J Hepatol 2015; 62: pp. 245-247.
17. Qi X., He C., Guo W., et. al.: Transjugular intrahepatic portosystemic shunt for portal vein thrombosis with variceal bleeding in liver cirrhosis: Outcomes and predictors in a prospective cohort study. Liver Int 2016; 36: pp. 667-676.
18. Schuppan D., Afdhal N.H.: Liver cirrhosis. Lancet 2008; 371: pp. 838-851.
19. Zhou C., Hou C., Cheng D., et. al.: Predictive accuracy comparison of MELD and Child-Turcotte-Pugh scores for survival in patients underwent TIPS placement: a systematic meta-analytic review. Int J Clin Exp Med 2015; 8: pp. 13464-13472.
20. Haskal Z.J., Rees C.R., Ring E.J., et. al.: Reporting standards for transjugular intrahepatic portosystemic shunts. J Vasc Interv Radiol 2003; 14: pp. S419-S426.
21. Hanley J.A., McNeil B.J.: A method for comparing the areas under the receiver operating characteristic curves derived from the same cases. Radiology 1983; 148: pp. 839-843.
22. Gaba R.C., Omene B.O., Podczerwinski E.S., et. al.: TIPS for treatment of variceal hemorrhage: clinical outcomes in 128 patients at a single institution over a 12-year period. J Vasc Interv Radiol 2012; 23: pp. 227-235.
23. Saad W.E.A., Darwish W.M., Davies M.G., et. al.: Stent-grafts for transjugular intrahepatic portosystemic shunt creation: specialized TIPS stent-graft versus generic stent-graft/bare stent combination. J Vasc Interv Radiol 2010; 21: pp. 1512-1520.
24. La Mura V., Abraldes J.G., Berzigotti A., et. al.: Right atrial pressure is not adequate to calculate portal pressure gradient in cirrhosis: a clinical-hemodynamic correlation study. Hepatology 2010; 51: pp. 2108-2116.
25. Silva-Junior G., Turon F., Baiges A., et. al.: Timing affects measurement of portal pressure gradient after placement of transjugular intrahepatic porto-systemic shunts in patients with portal hypertension. Gastroenterology 2017; 152: pp. 1358-1365.
26. Han G., Qi X., He C., et. al.: Transjugular intrahepatic portosystemic shunt for portal vein thrombosis with symptomatic portal hypertension in liver cirrhosis. J Hepatol 2011; 54: pp. 78-88.
27. Nicolas C., d’Alteroche L., Perarnau J.M.: Reply to: “shunt dysfunction: is it suitable as the primary end point in transjugular intrahepatic portosystemic shunt trials?”. J Hepatol 2015; 62: pp. 247-248.
28. Cura M., Cura A., Suri R., et. al.: Causes of TIPS dysfunction. AJR Am J Roentgenol 2008; 191: pp. 1751-1757.