Rationale and Objectives
This study aimed to investigate whether a simplified breast magnetic resonance imaging (MRI) protocol consisting of a localizer, one precontrast sequence, and three time-point postcontrast sequences (at 28 seconds, 84 seconds and 252 seconds after the contrast agent administration) is suitable for the characterization of breast lesions as compared to a full diagnostic protocol (FDP). This study also aimed to review the current literature concerning abbreviated breast MRI protocols and offer an alternative protocol.
Materials and Methods
Breast magnetic resonance (MR) examinations with detected breast lesions of 98 patients were retrospectively evaluated. Two expert radiologists in consensus reviewed the simplified breast protocol (SBP) first and only thereafter the regular FDP, recording a diagnosis for each detected lesion for both protocols. Receiver operating characteristic curve analysis was performed to determine the diagnostic performance of the SBP compared to the standard FDP. A revision of the previously reported abbreviated breast magnetic resonance protocols was also carried out.
Results
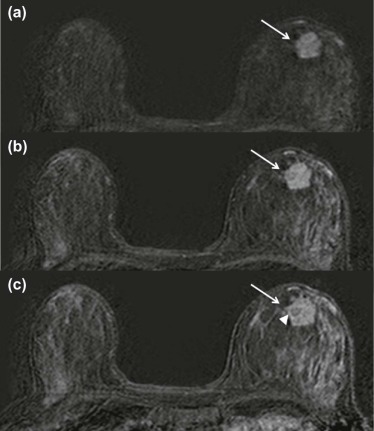
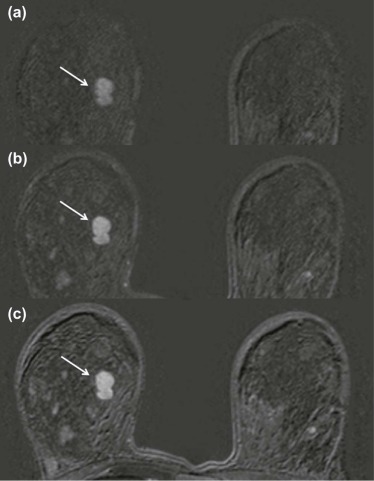
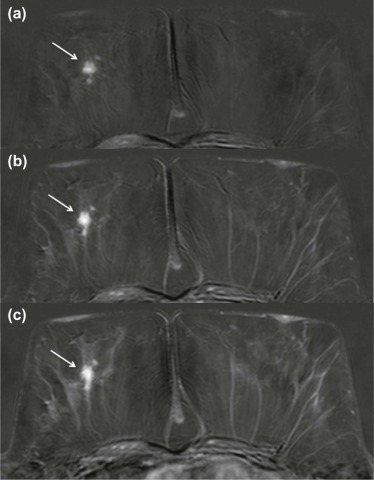
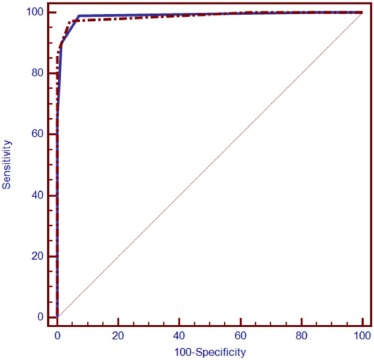
A total of 180 lesions were identified; of these, 110 (61%) were malignant and 70 (39%) were benign. Of the 110 malignant lesions, 86 (78%) were invasive ductal carcinoma, 18 (16%) were invasive lobular carcinoma, and 6 (6%) were ductal carcinoma in situ. Areas under the curve for the receiver operating characteristic curves for the SBP vs the FDP were equivalent (0.98 vs 0.99, respectively; P = 0.76). The SBP could be performed in approximately 6 minutes and 58 seconds, compared to 14 minutes and 48 seconds for the FDP.
Conclusions
An SBP protocol including a late postcontrast time point is accurate for the characterization of breast lesions and was comparable to the standard FDP protocol, allowing a potential reduction of the total acquisition and interpretation times.
Introduction
MMagnetic resonance imaging (MRI) is widely recognized as a useful imaging modality for the screening of high-risk women because of its higher sensitivity, for preoperative and post-treatment evaluation, for the investigation of carcinoma of unknown primary tumor or syndrome, and for patients without conclusive mammographic or sonographic imaging findings . Recently, there is increasing evidence on the use of abbreviated protocols (APs) for diagnostic purposes; many different abbreviated breast MRI protocols have been proposed as possible alternatives to the standard full breast MRI protocol to reduce acquisition time for breast cancer screening and for lesion characterization . In particular, Kuhl et al. have recently shown the accuracy of an AP for screening purpose, consisting of only one precontrast and one postcontrast acquisition and their derived images (first postcontrast subtracted and maximum intensity projection images). We have noticed that almost all the APs reported in the literature include a combination of morphologic T2-weighted sequence or early dynamic postcontrast time points; none of the above-mentioned APs include the later postcontrast time point, which is, according to our experience, as important as the first postcontrast time point to detect essential morphologic and dynamic breast lesions details. Therefore, the aim of this study was to investigate whether a breast MRI protocol consisting of a localizer, a precontrast acquisition, and three time-point postcontrast sequences (at 28, 84, and 252 seconds after the contrast agent administration), which we defined as a “simplified breast protocol” (SBP), is accurate for the characterization of breast lesions and faster as well, compared to a full diagnostic breast MRI protocol; we also aimed to revise the current literature concerning abbreviated breast MRI protocols.
Materials and Methods
Study Population
This retrospective study was approved by our local institutional review board.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Standard Full Diagnostic MRI Protocol
Get Radiology Tree app to read full this article<
Simplified Breast MRI Protocol (SBP)
Get Radiology Tree app to read full this article<
Table 1
Comparison of the Full Diagnostic MRI Protocol vs the Simplified Breast MRI Protocol
Full Diagnostic MRI Protocol (14 min and 48 s) Simplified Breast MRI Protocol (6 min and 58 s) Scout view or localizer ( ~ 1 min) Scout view or localizer ( ~ 1 min) Axial T2-weighted sequence (5 min) Dynamic contrast-enhanced axial T1-weighted 3D sequence (5 min and 58 s) Dynamic contrast-enhanced axial T1-weighted 3D sequence (5 min and 58 s) \* Axial T1-weighted high-resolution THRIVE sequence (2 min and 50 s)
3D, three-dimensional; MRI, magnetic resonance imaging; THRIVE, T1-weighted high-resolution isovolumetric examination.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Image Analysis
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Statistical Analysis
Get Radiology Tree app to read full this article<
Results
Get Radiology Tree app to read full this article<
Table 2
Final Diagnosis of Malignant and Benign Breast Lesions
Malignant Lesion_n_ = 110 61% Standard of Reference IDC 86 78% Histology ILC 18 16% Histology DCIS 6 6% Histology
Benign Lesion_n_ = 70 39% Standard of Reference Fibroadenoma 44 63% Follow-up ( n = 23) Histology ( n = 21) BI-RADS 3 lesions 18 26% Follow-up BI-RADS 2 lesions 8 11% Follow-up
BI-RADS, Breast Imaging Reporting and Data System; DCIS, ductal carcinoma in situ; IDC, invasive ductal carcinoma; ILC, invasive lobular carcinoma.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Table 3
Sensitivity, Specificity, PPV, NPV, Diagnostic Accuracy and 95% Confidence Intervals (in Brackets) for the FDP vs the SBP for the Characterization of Breast Lesions in the Patient Population ( n = 98)
Sensitivity (%) Specificity (%) PPV (%) NPV (%) Accuracy \* FDP 97 (92–99) 95 (88–99) 97 (92–99) 95 (88–99) 0.990 (0.96–0.99) SBP 99 (95–99) 93 (84–97) 95 (90–98) 98 (91–99) 0.989 (0.96–0.99)P Value 0.62 0.72 0.72 0.62 0.76
FDP, full diagnostic protocol; NPV, negative predictive value; PPV, positive predictive value; SBP, simplified breast protocol.
Get Radiology Tree app to read full this article<
Table 4
Summary of the Previous Published Articles Concerning Abbreviated Breast Magnetic Resonance Imaging Protocols
Author Purpose Abbreviated Protocol Duration Kuhl et al. 2014 Screening
3 minutes Mango et al. 2015 Screening
15 minutes Grimm et al. 2015 Screening Abbreviated 1
11 minutes Abbreviated 2
13 minutes Harvey et al. 2016 High-risk screening
4.4 minutes Moschetta et al. 2016 Characterization of breast lesions
10 minutes Machida et al. 2016 Screening
Not specified Chen et al. 2016 Screening in dense breast tissue
3 minutes Heacock et al. 2016 Evaluation of known breast cancer
12 minutes
MIP, maximum intensity projection; VIBE, volumetric interpolated breath-hold examination.
Get Radiology Tree app to read full this article<
Discussion
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
References
1. Spick C., Szolar D.H., Preidler K.W., et. al.: Breast MRI used as a problem-solving tool reliably excludes malignancy. Eur J Radiol 2015; 84: pp. 61-64.
2. Leung J.W.: MR imaging in the evaluation of equivocal clinical and imaging findings of the breast. Magn Reson Imaging Clin N Am 2010; 18: pp. 295-308.
3. Iacconi C., Galman L., Zheng J., et. al.: Multicentric cancer detected at breast MR imaging and not at mammography: important or not?. Radiology 2016; 279: pp. 378-384.
4. Lee C.H.: Problem solving MR imaging of the breast. Radiol Clin North Am 2004; 42: pp. 919-934.
5. Moy L., Elias K., Patel V., et. al.: Is breast MRI helpful in the evaluation of inconclusive mammographic findings?. AJR Am J Roentgenol 2009; 193: pp. 986-993.
6. Price J., Chen S.W.: Mammographically screen-detected asymmetric densities with architectural distortion and normal ultrasound at assessment: value of MRI as a problem-solving tool. J Med Imaging Radiat Oncol 2015; 59: pp. 312-319.
7. Mann R.M., Balleyguier C., Baltzer P.A., et. al.: Breast MRI: EUSOBI recommendations for women’s information. Eur Radiol 2015; 25: pp. 3669-3678.
8. Mann R.M., Kuhl C., Kindel K., et. al.: Breast MRI: guidelines from the European Society of Breast Imaging. Eur Radiol 2008; 18: pp. 1307-1318.
9. Lin D., Moy L., Axelrod D., et. al.: Utilization of magnetic resonance imaging in breast cancer screening. Curr Oncol 2015; 22: pp. e332-e335.
10. Yi A., Cho N., Yang K.S., et. al.: Breast cancer recurrence in patients with newly diagnosed breast cancer without and with preoperative MR imaging: a matched cohort study. Radiology 2015; 276: pp. 695-705.
11. Parsyan A., Moldoveanu D., Balram B., et. al.: Influence of preoperative magnetic resonance imaging on the surgical management of breast cancer patients. Am J Surg 2016; 211: pp. 1089-1094.
12. Diguisto C., Ouldamer L., Arbion F., et. al.: MRI evaluation of residual breast cancer after neoadjuvant chemotherapy: influence of patient, tumor and chemotherapy characteristics on the correlation with pathological response. Anticancer Res 2015; 35: pp. 581-585.
13. Mango V.L., Morris E., David Dershaw D., et. al.: Abbreviated protocol for breast MRI: are multiple sequences needed for cancer detection?. Eur J Radiol 2015; 84: pp. 65-70.
14. Kuhl C.K., Schrading S., Strobel K., et. al.: Abbreviated breast magnetic resonance imaging (MRI): first post contrast subtracted images and maximum-intensity projection—a novel approach to breast cancer screening with MRI. J Clin Oncol 2014; 32: pp. 2304-2310.
15. Grimm L.J., Soo M.S., Yoon S., et. al.: Abbreviated screening protocol for breast MRI: a feasibility study. Acad Radiol 2015; 22: pp. 1157-1162.
16. Harvey S.C., Di Carlo P.A., Lee B., et. al.: An abbreviated protocol for high-risk screening breast MRI saves time and resources. J Am Coll Radiol 2016; 13: pp. 374-380.
17. Moschetta M., Telegrafo M., Rella L., et. al.: Abbreviated combined MR protocol: a new faster strategy for characterizing breast lesions. Clin Breast Cancer 2016; 11: pii: S1526-8209(16)30028-3
18. Heacock L., Melsaether A.N., Heller S.L., et. al.: Evaluation of a known breast cancer using an abbreviated breast MRI protocol: correlation of imaging characteristics and pathology with lesion detection and conspicuity. Eur J Radiol 2016; 85: pp. 815-823.
19. Chen S.Q., Huang M., Shen Y.Y., et. al.: Application of abbreviated protocol of magnetic resonance imaging for breast cancer screening in dense breast tissue. Acad Radiol 2016;
20. Machida Y., Shimauchi A., Kanemaki Y., et. al.: Feasibility and potential limitations of abbreviated breast MRI: an observer study using an enriched cohort. Breast Cancer 2016; 24: pp. 411-419.
21. Morris E.A., Comstock C.E., Lee C.H., et. al.: ACR BI-RADS ® magnetic resonance imaging..2013.American College of RadiologyReston, VA:
22. Hanley J.A., McNeil B.J.: The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology 1982; 143: pp. 29-36.
23. De Long E.R., De Long D.M., Clarke-Pearson D.L.: Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 1988; 44: pp. 837-845.
24. Youden W.J.: An index for rating diagnostic tests. Cancer 1950; 3: pp. 32-35.
25. Partridge S.C., Stone K.M., Strigel R.M., et. al.: Breast DCE-MRI: influence of postcontrast timing on automated lesion kinetics assessments and discrimination of benign and malignant lesions. Acad Radiol 2014; 21: pp. 1195-1203.
26. Medved M., Li H., Abe H., et. al.: Fast bilateral breast coverage with high spectral and spatial resolution (HiSS) MRI at 3T. J Magn Reson Imaging 2017;
27. Bickelhaupt S., Laun F.B., Tesdorff J., et. al.: Fast and noninvasive characterization of suspicious lesions detected at breast cancer X-ray screening: capability of diffusion-weighted MR imaging with MIPs. Radiology 2016; 278: pp. 689-697.