Abstract
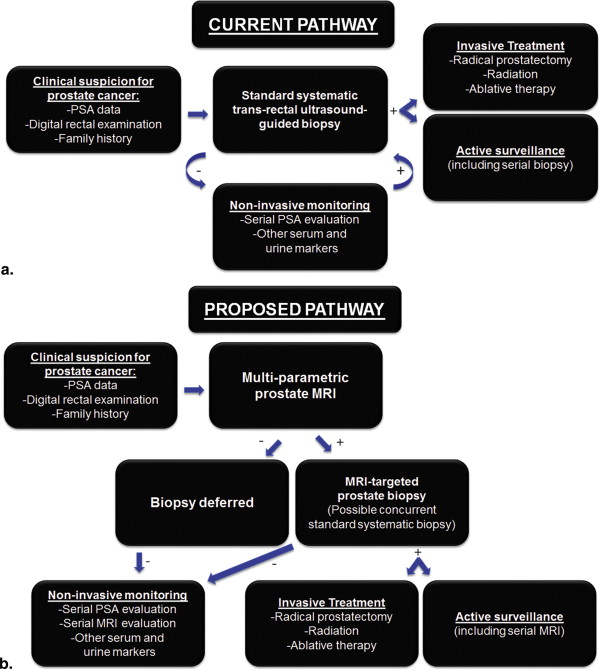
The contemporary management of prostate cancer (PCa) has been criticized as fostering overdetection and overtreatment of indolent disease. In particular, the historical inability to identify those men with an elevated PSA who truly warrant biopsy, and, for those needing biopsy, to localize aggressive tumors within the prostate, has contributed to suboptimal diagnosis and treatment strategies. This article describes how modern multi-parametric MRI of the prostate addresses such challenges and reduces both overdiagnosis and overtreatment. The central role of diffusion-weighted imaging (DWI) in contributing to MRI’s current impact is described. Prostate MRI incorporating DWI achieves higher sensitivity than standard systematic biopsy for intermediate-to-high risk tumor, while having lower sensitivity for low-grade tumors that are unlikely to impact longevity. Particular applications of prostate MRI that are explored include selection of a subset of men with clinical suspicion of PCa to undergo biopsy as well as reliable confirmation of only low-risk disease in active surveillance patients. Various challenges to redefining the standard of care to incorporate solely MRI-targeted cores, without concomitant standard systematic cores, are identified. These include needs for further technical optimization of current systems for performing MRI-targeted biopsies, enhanced education and expertise in prostate MRI among radiologists, greater standardization in prostate MRI reporting across centers, and recognition of the roles of pre-biopsy MRI and MRI-targeted biopsy by payers. Ultimately, it is hoped that the medical community in the United States will embrace prostate MRI and MRI-targeted biopsy, allowing all patients with known or suspected prostate cancer to benefit from this approach.
The time has come to change the manner by which prostate cancer is diagnosed and treated. Widespread population screening via serum prostate-specific antigen (PSA) testing has received harsh criticism within the media and medical community owing to the risk of overtreatment of indolent disease that is unlikely to result in disease-related morbidity or mortality . Most recently, the US Preventive Services Task Force has advised against PSA screening of the general population, regardless of age . Such criticism is noteworthy in view of a reduction in mortality through PSA screening that even opponents of screening generally acknowledge . For instance, the European Randomized Study of Screening for Prostate Cancer, which is the largest reported clinical trial to date of PSA screening, observed a 20% reduction in mortality . In addition, the Goteborg randomized screening trial reported a reduction in mortality of almost 50% at 14 years of follow-up, with a benefit from PSA screening that compared favorably to screening programs for other cancers . However, critics emphasize the indolent nature of prostate cancer in most cases, such that the cancer would fail to ever harm the patient if never diagnosed or treated, as supported by the frequent incidental detection of prostate cancer in autopsy series . This balance of benefit versus harm from treatment is at the crux of the concern regarding overdiagnosis from PSA screening . Although a large number of men with indolent disease must be diagnosed with, and treated for, prostate cancer to save one life, this number-needed-to-treat has varied widely among studies, ranging between five and 48 men , indicating the difficulty in quantifying the magnitude of the burden of overdiagnosis. A critical dichotomy in the interpretation of the problem and its solution exists between opponents and proponents of PSA screening. Although both groups recognize the overdetection problem, proponents of testing argue that modification of the screening paradigm offers the ability to reduce overdetection without compromising the observed improvements in survival.
Proponents of screening argue that the underlying problem is not inherently the PSA test itself but rather the next steps that occur after a positive result . These problems fundamentally relate to the historical inability to identify men with an elevated PSA level who truly are in need of biopsy, and, for those who do need biopsy, to localize aggressive tumors within the prostate . This limitation has led to clearly suboptimal diagnosis and treatment strategies and legitimate claims of overdiagnosis and overtreatment . In terms of the diagnostic technique, an abnormal PSA level has typically resulted in a systematic biopsy in which needles sample multiples areas of the prostate in a nontargeted fashion in hopes of identifying any tumor that may be present. This approach commonly identifies indolent tumor and cannot confidently exclude the presence of aggressive tumor and therefore is unable to reliably differentiate patients with low risk from intermediate-to-high-risk prostate cancer. In terms of treatment, prostate cancer has historically been managed via whole-gland therapy (surgery or radiation), in which the entire prostate is treated, even if there is evidence of only a tiny amount of tumor in one small part of the gland. Patients with low-risk disease are unlikely to receive any benefit from such interventions and instead are subject to harm because of the intervention’s negative impact on quality of life, including impotence and incontinence, in a considerable fraction of patients. For instance, one study estimated that >90% of prostatectomy patients with no previous problems reported sexual difficulties at 3-year follow-up, whereas >50% had urinary problems . Much of the impetus to treat men with low-risk disease has arisen from biopsy’s poor localization capability. In men with low-risk disease demonstrated on standard biopsy, >40% demonstrate higher Gleason score and/or locally advanced disease at the time of radical prostatectomy .
To address these issues, three closely linked paradigm shifts must occur. First, a means of determining which men with an elevated PSA level will benefit from biopsy is necessary. A multitude of PSA isoforms, serum and urine biomarkers, as well as clinical nomograms have been evaluated for their ability to improve the specificity of PSA . Although generally achieving improved specificity, the majority result in reductions in sensitivity without distinction between high- and low-risk disease. Second, a better biopsy is needed. Specifically, the biopsy that is performed after an abnormal PSA must reliably separate low- and intermediate-to-high-risk disease. Third, the diagnosis itself of prostate cancer must be “dissociated” from treatment . Rather than routinely offering aggressive therapy to all new diagnoses, such interventions should be primarily provided to patients having intermediate-to-high-risk disease, whereas patients with low-risk disease receive less-invasive treatment options or even no immediate intervention at all. This shift in approach incorporating individualized treatment selection can only be effective if the initial diagnostic pathway is trusted to give an accurate prognostic assessment. Indeed, “active surveillance” (AS) defers immediate intervention for patients with suspected low-risk disease, instead of closely monitoring the patient for any subsequent evidence of higher risk disease, which in turn triggers intervention with curative intent . By reducing overtreatment, AS reduces the potential burden resulting from overdiagnosis. Although of growing interest, AS remains heavily underused, representing the selected treatment approach in a minority of patients with low-risk disease .
In this article, we describe how magnetic resonance (MR) imaging (MRI) can address these challenges and reduce both overdiagnosis and overtreatment for prostate cancer. This aim requires not only high-quality acquisition and interpretation of multiparametric prostate MRI examinations but also implementation of targeted biopsies of MRI-defined lesions. Challenges to the incorporation of MRI and MRI-targeted biopsy into routine clinical practice are also considered.
Improved risk stratification and treatment selection using MRI
The accuracy of prostate MRI has improved over the past decade, partly relating to advances in scanner and receiver coil hardware . However, it has been the emergence of diffusion-weighted imaging (DWI) as a central component of prostate MRI acquisition and interpretation that has been crucial to MRI’s current impact. Apparent diffusion coefficient (ADC) values derived from DWI are significantly associated with tumor Gleason score , which is firmly established as the single best available predictor of prostate cancer outcome and currently serves as the primary determinant of a patient’s level of risk . Furthermore, prostate MRI incorporating DWI achieves high sensitivity for intermediate-to-high-risk tumor . Indeed, numerous recent studies report a negative predictive value of modern prostate MRI protocols for clinically significant cancer of >90% . Systems are currently commercially available to perform targeted biopsies either directly within the bore of the scanner or using real-time MRI/ultrasound fusion as guidance. These systems can be used to target MRI findings suspicious for clinically significant cancer and thereby improve the sensitivity of biopsy for such lesions.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Decreased detection of low-risk tumor
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Challenges
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Conclusions
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
References
1. Lefevre M.: PSA screening: the USPSTF got it right. J Fam Pract 2013; 62: pp. 617. 619
2. Ablin R.J.: The great prostate mistake.March 9, 2010.The New York Times Available at: http://www.nytimes.com/2010/03/10/opinion/10Ablin.html Accessed December 29, 2014
3. Moyer V.A., Force USPST: Screening for prostate cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med 2012; 157: pp. 120-134.
4. Klotz L.: Prostate cancer overdiagnosis and overtreatment. Curr Opin Endocrinol Diabetes Obes 2013; 20: pp. 204-209.
5. Schroder F.H., Hugosson J., Roobol M.J., et. al.: Screening and prostate-cancer mortality in a randomized European study. N Engl J Med 2009; 360: pp. 1320-1328.
6. Hugosson J., Carlsson S., Aus G., et. al.: Mortality results from the Goteborg randomised population-based prostate-cancer screening trial. Lancet Oncol 2010; 11: pp. 725-732.
7. Stamatiou K., Alevizos A., Agapitos E., et. al.: Incidence of impalpable carcinoma of the prostate and of non-malignant and precarcinomatous lesions in Greek male population: an autopsy study. Prostate 2006; 66: pp. 1319-1328.
8. Crawford E.D., Grubb R., Black A., et. al.: Comorbidity and mortality results from a randomized prostate cancer screening trial. J Clin Oncol 2011; 29: pp. 355-361.
9. Ahmed H.U.: Introduction—targeting the lesion, not the organ. Urol Oncol 2014; 32: pp. 901-902.
10. Loeb S., Bjurlin M.A., Nicholson J., et. al.: Overdiagnosis and overtreatment of prostate cancer. Eur Urol 2014; 65: pp. 1046-1055.
11. Pardo Y., Guedea F., Aguilo F., et. al.: Quality-of-life impact of primary treatments for localized prostate cancer in patients without hormonal treatment. J Clin Oncol 2010; 28: pp. 4687-4696.
12. Mufarrij P., Sankin A., Godoy G., et. al.: Pathologic outcomes of candidates for active surveillance undergoing radical prostatectomy. Urology 2010; 76: pp. 689-692.
13. Stephan C., Rittenhouse H., Cammann H., et. al.: New markers and multivariate models for prostate cancer detection. Anticancer Res 2009; 29: pp. 2589-2600.
14. Klotz L.: Point: active surveillance for favorable risk prostate cancer. J Natl Compr Canc Netw 2007; 5: pp. 693-698.
15. Ganz P.A., Barry J.M., Burke W., et. al.: National Institutes of Health State-of-the-Science Conference: role of active surveillance in the management of men with localized prostate cancer. Ann Intern Med 2012; 156: pp. 591-595.
16. Loeb S., Berglund A., Stattin P.: Population based study of use and determinants of active surveillance and watchful waiting for low and intermediate risk prostate cancer. J Urol 2013; 190: pp. 1742-1749.
17. Hoeks C.M., Barentsz J.O., Hambrock T., et. al.: Prostate cancer: multiparametric MR imaging for detection, localization, and staging. Radiology 2011; 261: pp. 46-66.
18. Barentsz J.O., Richenberg J., Clements R., et. al.: ESUR prostate MR guidelines 2012. Eur Radiol 2012; 22: pp. 746-757.
19. Hambrock T., Somford D.M., Huisman H.J., et. al.: Relationship between apparent diffusion coefficients at 3.0-T MR imaging and Gleason grade in peripheral zone prostate cancer. Radiology 2011; 259: pp. 453-461.
20. Hugosson J., Carlsson S.: Overdetection in screening for prostate cancer. Curr Opin Urol 2014; 24: pp. 256-263.
21. Turkbey B., Mani H., Shah V., et. al.: Multiparametric 3T prostate magnetic resonance imaging to detect cancer: histopathological correlation using prostatectomy specimens processed in customized magnetic resonance imaging based molds. J Urol 2011; 186: pp. 1818-1824.
22. Grey A.D., Chana M.S., Popert R., et. al.: Diagnostic accuracy of magnetic resonance imaging (MRI) prostate imaging reporting and data system (PI-RADS) scoring in a transperineal prostate biopsy setting. BJU Int 2014; [Epub ahead of print]
23. Abd-Alazeez M., Ahmed H.U., Arya M., et. al.: The accuracy of multiparametric MRI in men with negative biopsy and elevated PSA level—can it rule out clinically significant prostate cancer?. Urol Oncol 2014; 32: pp. 45.e17-45.e22.
24. Ouzzane A., Puech P., Villers A.: How accurately can MRI detect indolent disease?. Curr Opin Urol 2014; 24: pp. 264-269.
25. Pepe P., Garufi A., Priolo G., et. al.: Can 3-Tesla pelvic phased-array multiparametric MRI avoid unnecessary repeat prostate biopsy in patients with PSA < 10 ng/mL?. Clin Genitourin Cancer 2015; 13: pp. e27-e30.
26. Da Rosa M.R., Milot L., Sugar L., et. al.: A prospective comparison of MRI-US fused targeted biopsy versus systematic ultrasound-guided biopsy for detecting clinically significant prostate cancer in patients on active surveillance. J Magn Reson Imaging 2015; 41: pp. 220-225.
27. Overduin C.G., Futterer J.J., Barentsz J.O.: MRI-guided biopsy for prostate cancer detection: a systematic review of current clinical results. Curr Urol Rep 2013; 14: pp. 209-213.
28. Marks L., Young S., Natarajan S.: MRI-ultrasound fusion for guidance of targeted prostate biopsy. Curr Opin Urol 2013; 23: pp. 43-50.
29. Hoeks C.M., Somford D.M., van Oort I.M., et. al.: Value of 3-T multiparametric magnetic resonance imaging and magnetic resonance-guided biopsy for early risk restratification in active surveillance of low-risk prostate cancer: a prospective multicenter cohort study. Invest Radiol 2014; 49: pp. 165-172.
30. Stamatakis L., Siddiqui M.M., Nix J.W., et. al.: Accuracy of multiparametric magnetic resonance imaging in confirming eligibility for active surveillance for men with prostate cancer. Cancer 2013; 119: pp. 3359-3366.
31. Vourganti S., Rastinehad A., Yerram N.K., et. al.: Multiparametric magnetic resonance imaging and ultrasound fusion biopsy detect prostate cancer in patients with prior negative transrectal ultrasound biopsies. J Urol 2012; 188: pp. 2152-2157.
32. Delongchamps N.B., Peyromaure M., Schull A., et. al.: Prebiopsy magnetic resonance imaging and prostate cancer detection: comparison of random and targeted biopsies. J Urol 2013; 189: pp. 493-499.
33. Puech P., Rouviere O., Renard-Penna R., et. al.: Prostate cancer diagnosis: multiparametric MR-targeted biopsy with cognitive and transrectal US–MR fusion guidance versus systematic biopsy—prospective multicenter study. Radiology 2013; 268: pp. 461-469.
34. Moore C.M., Petrides N., Emberton M.: Can MRI replace serial biopsies in men on active surveillance for prostate cancer?. Curr Opin Urol 2014; 24: pp. 280-287.
35. Moore C.M., Ridout A., Emberton M.: The role of MRI in active surveillance of prostate cancer. Curr Opin Urol 2013; 23: pp. 261-267.
36. Valerio M., Ahmed H.U., Emberton M., et. al.: The role of focal therapy in the management of localised prostate cancer: a systematic review. Eur Urol 2014; 66: pp. 732-751.
37. Oto A., Sethi I., Karczmar G., et. al.: MR imaging-guided focal laser ablation for prostate cancer: phase I trial. Radiology 2013; 267: pp. 932-940.
38. Ahmed H.U., Hindley R.G., Dickinson L., et. al.: Focal therapy for localised unifocal and multifocal prostate cancer: a prospective development study. Lancet Oncol 2012; 13: pp. 622-632.
39. Ahmed H.U., Emberton M.: Active surveillance and radical therapy in prostate cancer: can focal therapy offer the middle way?. World J Urol 2008; 26: pp. 457-467.
40. McClure T.D., Margolis D.J., Reiter R.E., et. al.: Use of MR imaging to determine preservation of the neurovascular bundles at robotic-assisted laparoscopic prostatectomy. Radiology 2012; 262: pp. 874-883.
41. Langer D.L., van der Kwast T.H., Evans A.J., et. al.: Intermixed normal tissue within prostate cancer: effect on MR imaging measurements of apparent diffusion coefficient and T2—sparse versus dense cancers. Radiology 2008; 249: pp. 900-908.
42. Rosenkrantz A.B., Mendrinos S., Babb J.S., et. al.: Prostate cancer foci detected on multiparametric magnetic resonance imaging are histologically distinct from those not detected. J Urol 2012; 187: pp. 2032-2038.
43. Pokorny M.R., de Rooij M., Duncan E., et. al.: Prospective study of diagnostic accuracy comparing prostate cancer detection by transrectal ultrasound-guided biopsy versus magnetic resonance (MR) imaging with subsequent MR-guided biopsy in men without previous prostate biopsies. Eur Urol 2014; 66: pp. 22-29.
44. Radtke J.P., Kuru T.H., Boxler S., et. al.: Comparative analysis of transperineal template-saturation prostate biopsy versus MRI-targeted biopsy with MRI-US fusion-guidance. J Urol 2015; 193: pp. 87-94.
45. Rouse P., Shaw G., Ahmed H.U., et. al.: Multi-parametric magnetic resonance imaging to rule-in and rule-out clinically important prostate cancer in men at risk: a cohort study. Urol Int 2011; 87: pp. 49-53.
46. Yerram N.K., Volkin D., Turkbey B., et. al.: Low suspicion lesions on multiparametric magnetic resonance imaging predict for the absence of high-risk prostate cancer. BJU Int 2012; 110: pp. E783-E788.
47. American Urological Association. White Paper: AUA/Optimal Techniques of Prostate Biopsy and Specimen Handling. Available at: http://www.auanet.org/common/pdf/education/clinical-guidance/Prostate-Biopsy-WhitePaper.pdf . Accessed December 29, 2014.
48. Quentin M., Blondin D., Arsov C., et. al.: Prospective evaluation of magnetic resonance imaging guided in-bore prostate biopsy versus systematic transrectal ultrasound guided prostate biopsy in biopsy naive men with elevated prostate specific antigen. J Urol 2014; 192: pp. 1374-1379.
49. Habchi H., Bratan F., Paye A., et. al.: Value of prostate multiparametric magnetic resonance imaging for predicting biopsy results in first or repeat biopsy. Clin Radiol 2014; 69: pp. e120-e128.
50. Abd-Alazeez M., Kirkham A., Ahmed H.U., et. al.: Performance of multiparametric MRI in men at risk of prostate cancer before the first biopsy: a paired validating cohort study using template prostate mapping biopsies as the reference standard. Prostate Cancer Prostatic Dis 2014; 17: pp. 40-46.
51. Martin P.R., Cool D.W., Romagnoli C., et. al.: Magnetic resonance imaging-targeted, 3D transrectal ultrasound-guided fusion biopsy for prostate cancer: quantifying the impact of needle delivery error on diagnosis. Med Phys 2014; 41: pp. 073504.
52. de Rooij M., Crienen S., Witjes J.A., et. al.: Cost-effectiveness of magnetic resonance (MR) imaging and MR-guided targeted biopsy versus systematic transrectal ultrasound-guided biopsy in diagnosing prostate cancer: a modelling study from a health care perspective. Eur Urol 2014; 66: pp. 430-436.
53. Akin O., Riedl C.C., Ishill N.M., et. al.: Interactive dedicated training curriculum improves accuracy in the interpretation of MR imaging of prostate cancer. Eur Radiol 2010; 20: pp. 995-1002.
54. Seltzer S.E., Getty D.J., Tempany C.M., et. al.: Staging prostate cancer with MR imaging: a combined radiologist-computer system. Radiology 1997; 202: pp. 219-226.
55. Elliott M.L., Houn F.: Mammography improves under MQSA oversight. Diagn Imaging (San Franc) 1998; 20: pp. 37-38.
56. American College of Radiology. Magnetic Resonance Prostate Imaging Reporting and Data System (MR PI-RADS). Available at: http://www.acr.org/Quality-Safety/Resources/PIRADS . Accessed December 29, 2014.
57. Giles S.L., Morgan V.A., Riches S.F., et. al.: Apparent diffusion coefficient as a predictive biomarker of prostate cancer progression: value of fast and slow diffusion components. AJR Am J Roentgenol 2011; 196: pp. 586-591.
58. Roe K., Kakar M., Seierstad T., et. al.: Early prediction of response to radiotherapy and androgen-deprivation therapy in prostate cancer by repeated functional MRI: a preclinical study. Radiat Oncol 2011; 6: pp. 65.
59. Chamie K., Sonn G.A., Finley D.S., et. al.: The role of magnetic resonance imaging in delineating clinically significant prostate cancer. Urology 2014; 83: pp. 369-375.
60. Litjens G.J., Hambrock T., Hulsbergen-van de Kaa C., et. al.: Interpatient variation in normal peripheral zone apparent diffusion coefficient: effect on the prediction of prostate cancer aggressiveness. Radiology 2012; 265: pp. 260-266.
61. Carter H.B., Partin A.W., Walsh P.C., et. al.: Gleason score 6 adenocarcinoma: should it be labeled as cancer?. J Clin Oncol 2012; 30: pp. 4294-4296.